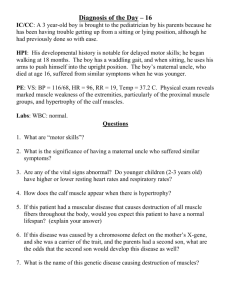
muscular dystrophy
advertisement

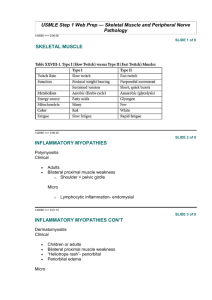
Approach to myopathy • Hereditary & Acquired • Hereditary Myopathy Classification • • • • Dystrophy Congenital myopathy Channelopathies & myotonia Metabolic (fatty acid/glycogensis/mitochondrial) Muscular dystrophy • Inherited myopathy characterized by progressive muscles weakness &degeneration &subsequent replacement by fibrous & fatty connective tissue • . Muscular Dystrophy affects muscular strength and action, some of which first become obvious in infancy, and others which develop in adolescence or young adulthood. The syndromes are marked by either generalized or localized muscle weakness, difficulties with walking or maintaining posture, muscle spasms, and in some instances, neurological, behavioral, cardiac, or other functional limitations Classification of Muscular Dystrophy Sex-linked: DMD, BMD, EDMD Autosomal recessive: LGMD, infantile FSHD Autosomal dominant: FSHD, distalMD, ocular MD, oculopharyngeal MD. Progressive Muscular Dystrophy Type Onset Age (years) Clinical Features Other organ systems involved Duchenne Before 5 1.Progressive weakness of girdle muscles. 2.unable to walk after age 12 3.progressive kyphoscoliosis 4.Respiratory failure in 2dor 3d decade. Cardiomyopathy Mental impairment Becker 5-25yr early childhood to adult 1.Progressive weakness of girdle muscles 2. able to walk after age 15. 1.3. respiratory failure may develop by 4th grade Cardiomyopathy Emery-Dreifuss Childhood to adult Elbow contractures, humeral and perineal weakness Cardiomyopathy Limb-Girdle early childhood to adult Slow progressive weakness of shoulder and hip girdle muscles Cardiomyopathy Progressive Muscular Dystrophy Type Onset Age (years) Clinical Features Other organ systems involved Congenital At birth or within 1st few months .Hypotonia, contractures, delayed milestones Progression to respiratory failure in some; CNS and Eye abnormalities Facioscapulohumeral Before age 20 Slowly progressive weakness of face, shoulder girdle, and foot dorsiflexion Deafness Coat’s (eye) disease Oculopharyngeal 5th to 6th decade Slowly progressive weakness of extraocular, pharyngeal, and limb muscles ______ Myotonic Usually 2nd decade May be infancy if mother affected Slowly progressive weakness of face, shoulder girdle, and foot dorsiflexion Cardiac conduction defects Mental impairment Cataracts Frontal baldness Gonadal atrophy Duchenne MD • • • • • Incidence: 1/3500 male birth 1/3 new mutation c/p:as early as 2-3y with delay milestones Progressive limb girdle pattern Fall 5-6y/difficult climb stair 8y, confined to wheelchair 12y DMD: Clinical manifestation • Onset : age 3-6 years • Progressive weakness • Pseudohypertrophy of calf muscles • Spinal deformity • Cardiopulmonary involvement • Mild - moderate MR DMD: Diagnosis Gower’s sign DMD: Natural history Progress slowly and continuously muscle weakness ( lower --> upper extremities, Progressive kyphscliosis due to Paraspinal muscles weakness unable to ambulate: 10 year (7-12) death from pulmonary/ cardiac failure: 2-3rd decade Beckers MD • • • • • • • • Is milder form 5/100,000 Age :5-15y Wheelchair at 30y Equinous and varus foot High rate of scoliosis Cardiac similar to duchenne Death by age 40 Emery-dreifuss • X linked • onset :childhood • Triad of: 1-early contracture elbow, ankle &posterior cervical 2-progressive scapulohumroperoneal 3-cardiomyopathy with atrial conduction defect EDMD • Diagnosis – Gower’s sign – Mildly/moderately elevated CPK – EMG: myopathic – Normal dystrophin • Natural history – 1st 10 y: mild weakness – Later: contracture, cardiac abnormality – 5th-6th decade: can ambulate – Poor prognosis in obesity, untreated equinus contractures. Limb girdle dystrophy • AR majority • Onset: adolescence or late • Clinical manifestation – Slow progression, contracture & disability – Rarely significant scoliosis • Classification – Pelvic girdle type • common – Scapulohumeral type • rare Fascioscapulohumeral muscular dystrophy Autosomal dominant • • Epidemiology Female > male Clinical manifestation – Age of onset: late childhood/ early adult - No cardiac, CNS involvement Clinical manifestation – – – – – Muscle weakness ( face, shoulder, upper arm ) Lack of facial mobility Incomplete eye closure Pouting lips Transverse smile Absence of eye and forehead wrinkles • Sparing – Deltoid – Distal pectoralis major – Erector spinae FSMD: Clinical manifestation Winging scapula Markedly decreased shoulder flexion & abduction Horizontal clavicles forward sloping Rare scoliosis Congenital muscular dystrophy – Autosomal recessive • c/p: Hypotonia &proximal weakness, arthrogryposis, Stiffness of joint, Congenital hip dislocation, subluxation Achillis tendon contracture, talipes equinovarus,Scoliosis • Two types • CNS involvement: sever mental retardation ,visual, seizure ..cerebrocular dysplasia, progressive death by age 10-12 • No CNS :classic type MRI (hypomyelination), benign outcome, non progressive • Muscle biopsy :dystrophy… Myotonic dystrophy Autosomal dominant • Affect : skeletal,cardiac, smooth muscles, eye,endocrine &brain • Onset :at any age ,usually at late 2nd decade • Some individual can be symptoms free their entire life • Sever form :congenital myotonic dystrophy • C/P: weakness: (facial,temporalis wasting,ptosis,neck flexor,distal weakness progress to involve limb girdle) oculopharengeal Autosomal dominant • Onset:5th &6th decade • Ptosis &dysphagea later all extra ocular muscles &extremities affected (limb girdle) but distal can be significant in some variant • Slow progressive ,death from aspiration pneumonia or starvation Congenital myopathy • • • • Are distinguished from dystrophy in three respect: Characteristic morphologic alteration At birth Non progressive • c/p: hypotonia with subsequent developmental delay Reduce muscles bulk, slender body build &long narrow face Skeletal abnormalities: high arched palate ,pectus exacavitum, kyphscliosis, dislocated hip, pes cavus) • • • Absent or reduced muscle stretch reflex • Weakness: limb girdle mostly, but distal weakness exist Muscular Dystrophy: Rehabilitation Management Respiratory Management Patients with DMD are at increased risk of respiratory complications Because of progressive loss of muscle strength: – Cough may be ineffective – Nocturnal hypoventilation – Sleep-disordered breathing PT can assist with respiratory management by having patient breathe against a resistive load (water in pool), breath-holding, bubble-blowing, to improve ventilatory strength and endurance. Important to note signs and symptoms of hypoventilation to refer patient to respiratory physician. – Fatigue, dyspnea, tachycardia, morning/continuous headaches, sleep dysfunction, nightmares, difficulty concentrating Cardiac Management Cardiomyopathy and/or cardiac arrhythmia are major sources of mortality in DMD The heart/myocardium have areas of hypertrophy, atrophy, and fibrosis Failure to see a cardiac specialist early in the disease process have led to late treatment and poor outcomes Higher levels of fitness are associated with better cardiac health Goals of Physical Therapy Prolong independent ambulation Maximize functional ability Prevent complications of inactivity Improve emotional well-being Physical Therapy Interventions Stretching/Positioning Management of contractures Assistive devices Exercise Objective measures and testing to monitor progression Objective measures Strength testing- MMT to monitor disease progression and predict functional losses, assess responses to treatment and monitor muscle imbalances – Test Lower exermiies every 6 months when ambulatory; test UE and LE every 6 months when non-ambulatory ROM: goniometry to identify hypomobility, jt contractures that may contribute to functional deterioration or to musculoskeletal/integumentary complications, or to note need of splinting/orthotics. – In ambulatory phase, measure hips, knees, ankles (ITB, H/S, heelcords). In non-ambulatory phase, measure UE as well as LE (elbows, wrists, finger flexors) Stretching • Combination of AROM, AAROM, PROM, prolonged elongation (splinting, positioning) • Minimum of 4-6 days per week, at home/school and in the clinic • Heelcords: Gastrocnemius/ Achilles Tendon lengthening into dorsiflexion • Tensor Fascia Latae/Iliotibial Band: stretch hip into adduction, internal rotation, and extension. • Other muscles throughout the hips, knees and ankles • In non-ambulatory phase, also focus on upper extremities: finger flexors, wrist flexors, elbow and shoulder joints Self stretches Ilio-tibial band (ITB) Active assisted stretches Assistive Devices: AFOs • Custom-molded and comfortable for optimum foot and ankle alignment • Throughout life: AFO’s are appropriate at night to prevent or minimize the progression of equinus contractures • Late stages: – KAFOs for non-ambulatory boys to prevent contracture and deformity (not for use at night) – Resting hand splints for finger flexors Assistive Devices Con’t • Wheelchair: Need appropriate postural positioning to prevent scoliosis and back pain/aches – Powered for more involved patients. – Manual Lightweight for less involved patients so can self propel and increase independence, as well as provide arm exercise • Standing Frames: A few hours per day, even with minimal weight bearing, to prevent and reduce the severity of contractures, decubitis ulcers, and scoliosis. • Also improves bone mineral density, circulation, and GI and respiratory functions. Recommended Exercise for DMD • Low resistive and aerobic exercise are justified to: – Prevent deconditioning, decreased fitness, disuse atrophy and joint contractures – Counteract secondary complications of inactivity such as obesity, Diabetes, osteoporosis and cardiovascular diseases • Long term, low-intensity, preferably no load (or low-load) weight-bearing activity to reduce mechanical stress on the muscle – Increased Type I fibers, which are less vulnerable to degeneration – Will not promote hypertrophy Recommended Exercise for DMD, Con’t • Use caution to ensure that cardiovascular or muscular complications do not develop • High-resistance and eccentric exercise is NOT recommended, although it has not actually been proven harmful for a DMD patient • Aquatic Therapy! Excellent for improving/ maintaining mobility, strength, flexibility, and aerobic conditioning and cardiopulmonary fitness