محاضرة رقم 3
advertisement

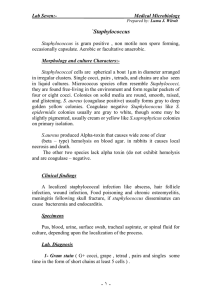
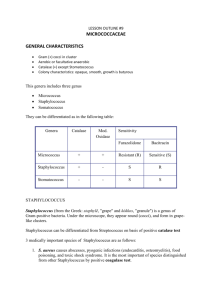
Staphyloccocci - derived from Greek “stapyle” (bunch of grapes) Gram positive cocci arranged in clusters Hardy organisms surviving many non physiologic conditions Include a major human pathogen and skin commensals Spherical cells arranged in irregular clusters Gram-positive Lack spores and flagella May have capsules 31 species 3 Staphylococcus species are generally nonfastidious They grow well on media without blood or other special supplements Micrococcus species and R. mucilaginosa are mildly fastidious and grow more slowly than Staphylococcus sp. Staphylococcus and Micrococcus tolerate a high salt concentrations; they grow on media containing 5%-7.5% NaCl (e.g. Mannitol Salt Agar) Staphylococcus species are facultatively anaerobic, as is Rothia. Micrococcus is an obligate aerobe. Staphylococcus species produce a variety of hemolysins and other toxins Staphylococcus species can be differentiated from Micrococcus species based upon oxygen requirements: Staph is facultative and Micrococcus species are obligate aerobes Rothia can be differentiated from Staphylococcus and Micrococcus by its lack of growth on a high-salt medium, its negative catalase reaction, and its tendency to adhere firmly to an agar surface All Staph group organisms that grow in air are catalase positive Rothia is catalase negative (or weakly positive). Catalase POS Staphylococcus Catalase NEG Gram Positive Coccus Catalase + Salt Tolerant Yes Facultative Yes Staphylococcus No Rothia No Micrococcus _ Streptococcus Group Coagulase negative Coagulase positive S. aureus S. epidermidis S. saprophyticus S. haemolyticus Gram-positive spherical cells (0.5-1.5 mm) in singles, pairs, and clusters Appear as “bunches of grapes” Gram-stained smear of staphylococci from colony Scanning electron micrograph of staphylococci Nonmotile Non–spore-forming Nonencapsulated Catalase-producing Oxidase: negative Glucose fermenters Primarily aerobic, some facultatively anaerobic Bacitracin resistant Grow on agar that contains peptone Inhibited by media that has high bile salt concentration Some are ß-hemolytic Colony morphology: buttery looking, cream or white colored Staph. Are gram positive cocci arranged in grape like clusters. The genus Staphylococcus includes 3 species of medical importance; staph. aureus, staph.epidermidis and staph. Saprophyticus. Of the three, staph. aureus is the most important. Staph.aureus is distinguished from the others by being coagulase positive, manitol positive and by causing haemolysis of RBCs in vitro. Staph epidermidis and staph. Saprophyticus are coagulase negative and are usually commensals. However, they are considered to be potentially pathogenic. Staph. aureus causes pyogenic infections which can be hospital acquired, food poisoning and toxic shock syndrome. (catalase positive)Coagulase-positive Staphylococcus aureus Coag.-neg. Staphylococcus epidermidis, S. saprophyticus Impetigo is a contagious superficial pyoderma, caused by Staphylococcus aureus and/or group A Capsule or slime layer (glycocalyx) Peptidoglycan (PG) Teichoic acid is covalently linked to PG and is species specific: S. aureus S. epidermidis Protein ribitol teichoic acid (polysaccharide A) glycerol teichoic acid (polysaccharide B) A is covalently linked to PG Clumping factor (bound coagulase) Coagulases (bound or free) Antigenic Hyaluronidase “spreading factor” of S. aureus Nuclease Cleaves DNA and RNA in S. aureus Protease Staphylokinase (fibrinolysin) Lipases Esterases Differential Characteristics S. aureus Coagulase Fibrinogen Fibrin Staphylococcus aureus Coagulase POS Coagulase NEG Biochemical reactions: 1) Catalase test- Positive. 2) Coagulase testi) Slide coagulase test- Positive. ii) Tube coagulase test- Positive. SLIDE COAGULASE TEST TUBE COAGULASE TEST 3) Reduces nitrate to nitrite. 4) Ferments mannitol anaerobically with acid only. 5) Urea hydrolysis test- Positive. 6) Gelatin liquefaction test- Positive. 7) Produces Lipase. 8) Produces Phosphatase. 9) Produces Thermostable nuclease. PATHOGENICITY: Source of infection: A) Exogenous: patients or carriers B) Endogenous: From colonized site Mode of transmission: A) Contact: direct or indirect( through fomites) B) Inhalation of air borne droplets Virulence factors: These include A) Cell associated factors B) Extracellular factors A) CELL ASSOCIATED FACTORS: a) Cell associated polymers b) Cell surface proteins a) CELL ASSOCIATED POLYMERS 1. Cell wall polysaccharide 2. Teichoic acid 3. Capsular polysaccharide b) CELL SURFACE PROTEINS: 1. Protein A 2. Clumping factor (bound coagulase) Structure of Staphylococcal cell wall B) EXTRACELLULAR FACTORS a) Enzymes b) Toxins a) Enzymes: 1. Free coagulase 2. Catalase 3. Lipase 4. Hyaluronidase 5. DNAase 6. Thermonuclease 7. Staphylokinase (Fibrinolysin) 8. Phosphatase b) Toxins: 1. Cytolytic toxins i) Haemolysins Alpha haemolysin Beta haemolysin Gamma haemolysin Delta haemolysin ii) Leucocidin (Panton-Valentine toxin) 2. Enterotoxin 3. Toxic shock syndrome toxin (TSST) 4. Exfoliative (epidermolytic toxin) . Disease: Diseases produced by Staphylococcus aureus is studied under 2 groups: A) Infections B) Intoxications A) INFECTIONS: Mechanism of pathogenesis: Cocci gain access to damaged skin, mucosal or tissue site Colonize by adhering to cells or extracellular matrix Evade the host defense mechanisms and multiply Cause tissue damage Common Staphylococcal infections are: 1) Skin and soft tissue: Folliculitis, furuncle (boil), carbuncle, styes, abscess, wound infections, impetigo, paronychia and less often cellulitis. Folliculitis Folliculitis Furuncle (boil) Carbuncle Styes Abscess Impetigo Wound infection Paronychia Cellulitis 2) Musculoskeletal: Osteomyelitis, arthritis, bursitis, pyomyositis. osteomyelitis 3) Respiratory: Tonsillitis, pharyngitis, sinusitis, otitis, bronchopneumonia, lung abscess, empyema, rarely pneumonia. 4) Central nervous system: Abscess, meningitis, intracranial thrombophlebitis. 5) Endovascular: Bacteremia, septicemia, pyemia, endocarditis. Endocarditis 6) Urinary: Urinary tract infection. B) INTOXICATIOINS: The disease is caused by the bacterial exotoxins, which are produced either in the infected host or preformed in vitro. There are 3 typesFood poisoning Toxic shock syndrome Staphylococcal scalded skin syndrome .1 .2 .3 1) Food poisoning: Enterotoxin is responsible for manifestations of staphylococcal food poisoning. Eight types of enterotoxin are currently known, named A, B, C1-3, D, E, and H. It usually occurs when preformed toxin is ingested with contaminated food. The toxin acts directly on the autonomic nervous system to cause the illness, rather than gut mucosa. Cytolytic (cytotoxins; cytolysins) Alpha toxin - hemolysin Beta toxin Hemolytic activity Delta toxin Sphingomyelinase Gamma toxin Reacts with RBCs Cytopathic for: RBCsش Macrophages Lymphocytes Neutrophils Platelets Enterotoxic activity Leukocidin Virulence Factors: Exotoxins Enterotoxin Exfoliative toxin (epidermolytic toxin) Pyrogenic exotoxins Pass skin – first line of defense Benign infection Phagocytosis Antibody Inflammatory response Chronic infections Delayed hypersensitivity 1. Staphylococcus aureus 2. Coagulase positive Staphylococci Coagulase negative Staphylococci Staphylococcus epidermidis Staphylococcus saprophyticus Major human pathogen Habitat - part of normal flora in some humans and animals Source of organism - can be infected human host, carrier, fomite or environment Many neonates, children, adults intermittently colonised by S. aureus Usual sites - skin, nasopharynx, perineum Breach in mucosal barriers - can enter underlying tissue Characteristic abscesses Disease due to toxin production Due to direct effect of organism Local lesions of skin Deep abscesses Systemic infections Toxin mediated Food poisoning toxic shock syndrome Scalded skin syndrome Boils Styes Furuncles(infection of hair follicle) Carbancles (infection of several hair follicles) Wound infections(progressive appearance of swelling and pain in a surgical wound after about 2 days from the surgery) Impetigo(skin lesion with blisters that break and become covered with crusting exudate) Can be single or multiple Breast abscess can occur in 1-3% of nursing mothers in puerperiem Can produce mild to severe disease Other sites - kidney, brain from septic foci in blood 1. With obvious focus Osteomyelitis, septic arthritis 2. 3. No obvious focus heart (infective endocarditis) Brain(brain abscesses) Ass. With predisposing factors multiple abscesses, septicaemia(IV drug users) Staphylococcal pneumonia (Post viral) 1. Staphylococcal food poisoning Due to production of entero toxins heat stable entero toxin acts on gut produces severe vomiting following a very short incubation period Resolves on its own within about 24 hours High fever, diarrhoea, shock and erythematous skin rash which desquamate Mediated via ‘toxic shock syndrome toxin’ 10% mortality rate Described in two groups of patients ass. With young women using tampones during menstruation Described in young children and men Disease of young children Mediated through minor Staphylococcal infection by ‘epidermolytic toxin’ producing strains Mild erythema and blistering of skin followed by shedding of sheets of epidermis Children are otherwise healthy and most eventually recover 1. Gram stain and culture of pus 2. In all systemic infections Blood culture 3. In all pus forming lesions In infections of other tissues Culture of relevant tissue or exudate Skin commensal heart valves, Causes urinary tract infection in cathetarised patients Skin commensal Imp. Cause of UTI in sexually active young women Usually sensitive to wide range of antibiotics