factors affecting pulmonary ventillation
advertisement

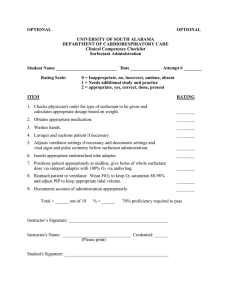
Lecture 8 Factors affecting Pulmonary Ventilation By: Dr. Khaled Ibrahim • By the end of this session, the student should be able to: o Outline the various factors affecting airway resistance and correlate it to changes in pulmonary ventilation. o Describe the metabolism of surfactant, discuss its significance and relate its deficiency to clinical conditions. o Define compliance of the lung and chest wall, illustrate and discuss the compliance curve and describe the effect of surfactant on it. o Discuss work of breathing and relate it to clinical conditions. Guyton and Hall- Textbook of Medical Physiology 12th edition, Page 467-468. Factors that affect pulmonary ventilation (airflow to the lung) 1. Resistance of the respiratory passage. 2. Pressure relationship in the thoracic cavity. 3. Surfactant. 4. Lung and chest compliance. 1) Resistance of the air passage : The resistance to air flow is inversely proportional to the diameter of the respiratory passage. i.e., ↑diameter (bronchodilatation) ----> ↓resistance & vice versa. The diameter of respiratory passage is affected by : i. Bronchomotor tone. ii. Bronchial mucosa. i. Bronchial muscle tone : Definition: It is the continuous partial contraction of smooth muscle fibers in the wall of bronchi & bronchioles. Significance: 1- to maintain the airways continuously patent. 2- to resist rupture of the airways during cough. Factors affecting: a- Autonomic nervous system : Sympathetic stimulation β2 adrenergic stimulators ------> Parasympathetic stimulation bronchodilatation. - Acting on M3 receptors ----> bronchoconstriction. (isoprenaline) α1 adrenergic stimulator ------> bronchoconstriction. The autonomic nervous activity shows "circadian rhythm" or "diurnal variation" in which the sympathetic activity reaches its maximum in the afternoon period while the parasympathetic activity is maximum in the late evening & early morning. b- Reflex bronchoconstriction: In response to stimulation of receptors in the trachea and large bronchi by irritants such as: cigarette smoke, inhaled dust, cold air, and noxious gases. c- Inflammatory mediators: May cause bronchodilatation as: PGs. May cause bronchoconstriction as: - Histamine - Serotonin - Platelets activating factor (PAF): This substance secreted from mast cells of the lung ----> bronchoconstriction , pulmonary V.C., bronchial oedema and mucus hypersecretion. ii. Bronchial mucosa : The presence of secretion OR ↑thickness of the mucosa causes an increase in air way resistance. Surfactant Definition: a substance which ↓the surface tension. Chemical structure: complex mixture of: phospholipids (dipalmitoyl lecithin), protein (apoproteins) and Ca2+. Synthesized & Released from alveolar type II cells from fatty acids that are extracted from the blood or formed in the lung. It is stored in organelles known as lamellar bodies. Release of surfactant occurs due to direct mechanical distortion of type II alveolar cells & it is directly proportional to tidal volume. Rapidly Degraded by phospholipases in the alveoli. Factors affecting synthesis of surfactant: 1- Thyroid hormone: ↑size & number of lamellar bodies in alveolar type II cells. 2- Cortisol hormone: accelerate surfactant formation. Function of surfactant: Respiratory function: ↓ the surface tension of the fluid lining the alveoli Through: 1- forms a monomolecular layer at the interface between the fluid lining and the air in the alveoli preventing the development of water-air interface. 2- scatters among the fluid molecules ----> ↓the attraction between them. Thus: 1- helps expansion of the lung & prevents its collapse. 2- maintain the alveoli dry. (maintain the fluid balance). Protective functions: 1. activate alveolar macrophages. 2. has a bacteriolytic effect: making the bacteria susceptible to alveolar macrophages. 3. helps the ciliary movement in the upper respiratory tract (mucociliary escalator) 4. The phospholipids of surfactant prevent excess immune response of T- lymphocytes. Surfactant decreases in the following conditions: 1. Respiratory distress syndrome: A fetal condition which may affect premature babies born before 8th month (the usual age for start of surfactant formation). Manifestations: Lack of surfactant -----> high surface tension of the fluid lining the alveoli causing: 1- collapse of lung alveoli. 2- Leakage of the plasma fluid into the alveoli ----> pulmonary edema. So, the condition is also called hyaline membrane disease. It is more sever in hypothyroid babies. Treated by placing the infant on a mechanical ventilator till the normal synthesis of surfactant starts. 2. Elective cesarean section: When it is life saving to the mother, the lecithin / sphingomyelin ratio should be measured. If it is less than 1.0: the mother is better injected with Cortisol which can help rapid maturation of surfactant. 3. Smoking: ↓surfactant due to destruction of type II alveolar cells. 4. Cardiac surgery: alveolar epithelium fail to secrete surfactant due to interruption of pulmonary circulation. Compliance Definition: The extent to which the lung expand for each unit increase in transpulmonary pressure. Transpulmonary pressure: is the difference between the intrapulmonary and Intrapleural pressures. pressure – intrapulmonary pressure). (Intrapleural Normal values: The normal compliance of the lungs in the average adult human is approximate 200 mL/cm of water pressure. While, The combined compliance of the lung and the thoracic wall is 130 ml/cm water pressure. Compliance curve: Definition: It is a curve relating lung volume changes to change in transpulmonary pressure, during inspiration and expiration. The pressure recorded is intra pleural pressure & represents the transpulmonary pressure, because the intra pulmonary pressure at the end of inspiration and expiration is zero. Compliance is slightly greater when measured during deflation than during inflation due to recoil tendency of the lung. Factors affecting compliance : Factors in the lung : * Elastic force of the lung tissue: ↓elasticity of the lung as in fibrosis ----> ↓compliance * Surface tension of the fluid lining the alveoli: ↑this tension as in cases of ↓surfactant -----> ↓compliance. Factors in the chest wall: - Contains some elastic components as: muscles, tendons and connective tissues of the chest. While the other components are non-elastic. ↓compliance of the chest wall occurs in the following conditions: - Deformities of spine as: kyphosis & scoliosis. - Arthritis of vertebra. - Skeletal muscle disease e.g. myasthenia gravis & poliomylities. - Obesity. 2) Pressure relationship in the thoracic cavity: These pressures include: i. Intrapulmonary pressure. ii. Intrapleural pressure. Intrapulmonary pressure Intrapleural pressure (I.P.P) Work of Breathing During quite normal respiration, work is done mainly during inspiration due to respiratory muscle contractions whereas expiration is entirely a passive process caused by elastic recoil of the lung and chest wall. Work of inspiration can be divided into: 1. Compliance work: 2. Tissue resistance work: 3. Airway resistance work : Definition: It is the work required to expand It is the work required to It is the work required to overcome overcome the resistance of non the lungs against its elastic force. elastic tissue of the lungs and airway resistance during the thoracic cage. movement of air into the lung. Increased by: - Decreased elasticity (fibrosis). - Diseases affecting thoracic cage Obstructive lung disease as: e.g. kyphosclosiosis. - obstruction of air way. - Lung congestion (Heart failure). - Muscle disease. - emphysema. - chronic bronchitis. - asthma which is characterized by increased expiratory work