Intravenous fluids

Prescribing Intravenous Fluids and
Infusions
Intravenous Fluids
Fluid charts
Intravenous infusions
Introduction
You will need to be competent in all areas pertaining to the prescription of intravenous fluids and infusions. This module will direct your learning but it is up to you to put the knowledge and skills into practice. The skills included in this module should be attempted in a skills centre before being practiced in the clinical setting.
Aims and Objectives
This module is designed to direct your learning around the knowledge and skills associated with intravenous fluids and infusions
By the end of this module students should be aware of
• The different intravenous fluids available
• The main differences between their composition, side effects and clinical application
• How to prescribe fluids on a fluid chart
• The steps required in setting up an intravenous infusion
• How to calculate the rate of a drip
• How to calculate the rates and dosage of infusions
Challenge to Knowledge and Practice
Before starting this module
(a) What do you understand by the terms crystalloid and colloid
(b) List some examples of each
(c) Give some examples of circumstances where you would prescribe a crystalloid.
Colloids and Crystalloids
Intravenous fluids may be divided into
• Crystalloid solutions
- clear fluids made up of water and electrolyte solutions; Will cross a semi-permeable membrane e.g Normal, hypo and hypertonic saline solutions; Dextrose solutions; Ringer’s lactate and
Hartmann’s solution.
• Colloid solutions
– Gelatinous solutions containing particles suspended in solution. These particles will not form a sediment under the influence of gravity and are largely unable to cross a semi-permeable membrane. e.g. Albumin, Dextrans, Hydroxyethyl starch [HES];
Haemaccel and Gelofusine
Saline Solutions
(1) 0.9% Normal Saline – Think of it as ‘Salt and water’
•
Principal fluid used for intravascular resuscitation and replacement of salt loss e.g diarrhoea and vomiting
•
Contains: Na+ 154 mmol/l, K+ - Nil, Cl - 154 mmol/l; But K+ is often added
•
IsoOsmolar compared to normal plasma
•
Distribution: Stays almost entirely in the Extracellular space
Of 1 litre – 750ml Extra cellular fluid; 250ml intravascular fluid
•
So for 100ml blood loss – need to give 400ml N.saline [only 25% remains intravascular]
(2) 0.45% Normal saline = ‘Half’ Normal Saline = HYPOtonic saline
•
Reserved for severe hyperosmolar states E.g. severe dehydration
•
Leads to HYPOnatraemia if plasma sodium is normal
•
May cause rapid reduction in serum sodium if used in excess or infused too rapidly. This may lead to cerebral oedema and rarely, central pontine demyelinosis ; Use with caution!
(3) 1.8, 3.0, 7.0, 7.5 and 10% Saline = HYPERtonic saline
•
Reserved for plasma expansion with colloids
•
In practice rarely used in general wards; Reserved for high dependency, specialist areas
•
Distributed almost entirely in the ECF and intravascular space. This leads to an osmotic gradient between the ECF and ICF, causing passage of fluid into the EC space. This fluid distributes itself evenly across the ECF and intravascualr space, in turn leading to intravascular repletion.
•
Large volumes will cause HYPERnatraemia and IC dehydration.
Dextrose solutions
•
•
•
•
•
•
•
(1) 5% Dextrose (often written D5W) – Think of it as ‘Sugar and Water’
Primarily used to maintain water balance in patients who are not able to take anything by mouth; Commonly used post-operatively in conjuction with salt retaining fluids ie saline; Often prescribed as 2L D5W: 1L N.Saline [‘Physiological replacement’ of water and Na+ losses]
Provides some calories [ approximately 10% of daily requirements]
Regarded as ‘electrolyte free’ – contains NO Sodium, Potassium, Chloride or
Calcium
Distribution: <10% Intravascular; > 66% intracellular
When infused is rapidly redistributed into the intracellular space; Less than 10% stays in the intravascular space therefore it is of limited use in fluid resuscitation.
For every 100ml blood loss – need 1000ml dextrose replacement [10% retained in intravascular space
Common cause of iatrogenic hyponatraemia in surgical patient
•
•
•
(2) Dextrose saline – Think of it as ‘a bit of salt and sugar’
Similar indications to 5% dextrose; Provides Na+ 30mmol/l and Cl sprinkling of salt and sugar!
Primarily used to replace water losses post-operatively
30mmol/l Ie a
Limited indications outside of post-operative replacement – ‘Neither really saline or dextrose’; Advantage – doesn’t commonly cause water or salt overload
.
Colloid solutions
• The colloid solutions contain particles which do not readily cross semi-permeable membranes such as the capillary membrane
• Thus the volume infused stays (initially) almost entirely within the intravascular space
• Stay intravascular for a prolonged period compared to crystalloids
• However they leak out of the intravascular space when the capillary permeability significantly changes e.g. Severe trauma or sepsis
• Until recently they were regarded as the gold standard for intravascular resuscitation.
• Because of their gelatinous properties they cause platelet dysfunction and interfere with fibrinolysis and coagulation factors (factor VIII) – thus they can cause significant coagulopathy in large volumes.
Colloid or Crystalloid Resuscitation what should you do?
Recommendations:
• Colloid should NOT be used as the sole fluid replacement in resuscitation; Volumes infused should be limited because of side effects and lack of evidence for their continued use in the acutely ill.
• In severely ill patients – principally use crystalloid and blood products; Colloid may be used in limited volume to reduce volume of fluids required or until blood products are available
• In elective surgical patients – replace fluid loss with
‘physiological Hartmann’s and Ringer’s solutions; Blood products and colloid may be needed to replace intravascular volume acutely.
The Fluid chart
The Fluid Chart
• You need to fill in all the areas of the chart, just like a drug chart.
• Useful to record the patient’s weight if known; Guestimate and record it if not.
• You will note there is a drop rate advised at the bottom of the chart shown in the previous slide
Using one of the blank charts supplied - Please write up 3 x 1litre of normal saline with 20 mmol/l of KCl in each litre – to run at 1litre/ 8 hourly; Patient is Mr Ali Khan Number
326587, DOB 13/09/81, weight 81Kg.
Consultant Ms Cuttem; Ward B3
Your fluid chart should look something like this. (I have written it out twice as I was unconvinced of my first attempt)
So now you’re experts and all aglow,
Have a go, at the examples below
(Dr Zeus and the IV calculations)
Using the fluid charts provided please prescribe intravenous fluids for the following patients for the next 24 hours. You may wish to ask a friendly
PRHO or SHO for advice with regard the correct fluid regimes.
(a) A 29 year old man who is nil by mouth awaiting an OGD for a small upper
GI bleed. He is haemo dynamically stable and well.
(b) A 74 year old woman who is 24 hours post laparotomy. The drains contain
180mls of blood stained fluid. She is NBM; BP 105 /70, Pulse 96 bpm.
(c) A 17 year old man admitted with suspected salmonella gastroenteritis. He is passing frequent fluid like stools and vomiting hourly. Urea 9.6mmol/l; BP
110/70, Pulse 100 bpm
(d) A 34 year old Type 1 Diabetic man who is admitted with DKA secondary to urinary sepsis; BP = 90/60, Pulse 120 bpm; Urea 38.9mmol/l Creatinine
231µmol/l.
(e) A 91 year old man who is admitted with severe dehydration, left sided hemiparesis and carpet burns. He is confused but it is estimated he has been on the floor of his bedroom for 72 hours. BP = 100/70, Pulse 120 bpm,
Urea 42.6mmol/l , Creatinine 311 µmol/l, CK 12,098 iu/l
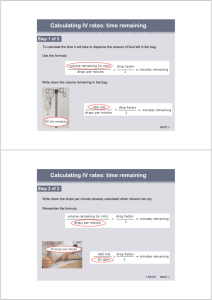
To calculate drip rates / transfusion rates
To calculate the drip rate (drops / minute)
Drip Rate gtt = Volume to be infused (ml) x Drop Factor (gtt/ml) min Time (minutes)
1 unit of blood is approximately 400ml in volume
E.g. A unit of blood is prescribed to run over 4 hours; The giving set has a drop factor of 20 gtt /ml. What is the drip rate (drops /min)?
(See next slide for answer and calculation)
Example one – Calculate the Transfusion rate
E.g. A unit of blood is prescribed to run over 4 hours; The giving set has a drop factor of 20 gtt /ml. What is the drip rate (drops /min) ?
Drip rate = 400 ml x 20 gtt ; Drip Rate is drops / minute
4 hour 1ml
Thus Drip Rate = 400ml x 20 gtt x 1 hour
4 hour 1 ml 60 minutes
By multidimensional analysis units are correct (drops / minute)
Drip Rate = 100 / 3 = 33 drops / minute
• Drop rate is rounded up or down to the nearest drop
• In the clinical setting to be able to count drops / minute it is sensible to have a number divisable by 4 - Thus you would set this drip at 32 drops per minute
Converting drip rate (gtt /min) to ml /hour
In high dependency areas caring for critically ill patients it may be necessary to know the infusion rate in ml/hour – this is important in setting infusion pumps (usually set in ml/hour) and when calculating fluid balance.
E.g. What is the transfusion rate in ml /hour of a blood transfusion being run at 40 drops / minute through a giving set with drop factor of
20 gtt / ml?
E.g. What is the transfusion rate in ml /hour of a blood transfusion being run at 40 drops / minute through a giving set with drop factor of 20 gtt / ml?
If there are 40 drops in one minute then in 1 hour
40 drops = X drops thus X = 40 x 60 = 2400 drops / hour
1 minute 60 minutes
If the giving set has drop factor of 20 drops/ 1 ml
20 drops = 2400 drops thus Xml = 2400 = 120 ml / hour
1 ml X ml 20
Therefore one could set an infusion pump to deliver this volume or it can be factored into the fluid input /hour.
Please work your way through the following problems.
(1) You are asked to run an intravenous infusion of 1litre of D5W over 6 hours.
What drop rate will you set the infusion at if the giving set has a drop factor of 10 gtt/ml?
(2) You are asked to set up a 1litre normal saline infusion to run over 10 hours.
The giving set has a drop factor of 20 gtt / ml. what rate will you set the drip at in drops/minute?
(1) A 91 yo woman is receiving intravenous fluids for dehydration. The SHO asks you to make sure her drip is running at the correct rate as he is concerned she may rapidly go into heart failure if it is infused too quickly.
There are 350ml remaining of a 1000ml bag which has been running for 6 hours. It is prescribed to run through in 12 hours. The drop rate is 10 drops
/minute and the giving set has a drop factor of 20gtt/ml. How long will the present drip take to run through? What adjustments (if any) will you need to make to ensure the drip runs through in 12 hours as prescribed?
You are asked to run an intravenous infusion of 1litre of
D5W over 6 hours. What drop rate will you set the infusion at if the giving set has a drop factor of 10 gtt/ml?
Drops = 1000ml x 1 hour x 10 gtt
Minute 6 hours 60 mins 1ml
= 1000 = 27.8 drops / min
36
Since we always round up or down to the nearest drop – the actual rate will be 28 drops / minute
You are asked to set up a 1litre normal saline infusion to run over 10 hours. The giving set has a drop factor of 20 gtt / ml. what rate will you set the drip at in drops/minute?
Drops = 1000ml x 1 hour x 20 gtt minute 10 hr 60 min 1 ml
= 100 = 33 drops / minute
3
A 91 year old woman is receiving intravenous fluids for dehydration. The SHO asks you to make sure her drip is running at the correct rate as he is concerned she may rapidly go into heart failure if it is infused too quickly. There are 350ml remaining of a 1000ml bag which has been running for 6 hours. It is prescribed to run through in 12 hours. The drop rate is 25 drops /minute and the giving set has a drop factor of 20gtt/ml. How long will the present drip take to run through? What adjustments (if any) will you need to make to ensure the drip runs through in 12 hours as prescribed?
Present Rate
650 ml = 1000ml Thus X = 6000 = 9.2 hours
6 hours X hours 650
To Run in 12 hours
X drops = 350ml x 1 hr x 20 drops pm minute 6 hr 60 min 1ml
= 350 = 19 drops / minute
18
Thus you will have to change the rate of the drip to run at 19 drops / minute ie reduce the rate by 6 drops/ minute
Try these for size …
(1) A 750ml infusion of 5% dextrose is infusing at 65gtt / min. The drop factor of the giving set is 60 gtt/ml. How long will the infusion take?
(2) A litre of normal saline is meant to be running over 8 hours. The drip is set at 83gtt/min,the giving set has a drop factor of 20gtt/ml.
(3) A litre of 5% dextrose is running at 80 gtt/min. The drop factor is 60 gtt/ml. What will the pump be set at in ml/Hr.
A 750ml infusion of 5% dextrose is infusing at 65gtt/min. The drop factor of the giving set is 60 gtt/ml. How long will the infusion take?
65 gtt = 750ml x 60 gtt x 1 hr min X hr ml 60min
X = 750 x 60 x 1
65 x 60
X = 11.5 hours
A litre of normal saline is meant to be running over 8 hours. The drip is set at 83gtt/min,the giving set has a drop factor of 20gtt/ml.
83 drops = 1000ml x 20 gtt x 1 hr min X hr ml 60min
X hr = 20,000 = 20,000 = 4 hours
83 x 60 4980
Thus you need to halve the drops /min to 42 drops / minute
A litre of 5% dextrose is running at 80 gtt/min. The drop factor is
60 gtt/ml. What will the pump be set at in ml/Hr.
If 80 drops = X drops minute 60minutes
X = 60 x 80 = 4800 drops / Hr
If 60 drops = 4800 drops
1ml Xml
Xml = 4800 = 80mls / Hr
60
Try these for size …..
(1) A heparin infusion is prescribed to run at 5000 units / Hr. The infusion is made up of
25,000 units in 500ml 5% dextrose. What rate in ml/hr will you set the pump?
(2) An aminophylline infusion is running at 30ml/hr. There is 0.5g / 500ml. It should be running @ 12mg / hour. What is the infusion rate and what will you do to ensure it runs at the correct rate?
(3) 2g of Kilabug is mixed up in 500ml of 5% dextrose. It is set to run at 5mg / min.
What rate in ml/hr will you set the infusion pump?
(4) A patient is on a GTN infusion for pulmonary oedema. The infusion is made up of
50mg in 250ml 5% dextrose. It is presently running at 20ml/hr. How many mcg / minute is the patient receiving?
(5) A patient is started on an inotrope infusion for cardiogenic shock. The infusion is
750mg in 250ml N. saline. It is running at 5 ml/hr. The patient becomes increasingly hypotensive and his urine output is dropping off. The infusion rate is changed to
12ml/hr. The patient is 70Kg. What dose in mcg / Kg/ min is the patient receiving?
(6) A second patient who weighs 100Kg is on an inotrope infusion running at
10mcg/kg/min. You receive a pharmacy prepared bag with 1g in 500ml. A what rate
(ml/hr) will you set the pump
A heparin infusion is prescribed to run at 5000 units / Hr. The infusion is made up of 25,000 units in 500ml 5% dextrose. What rate in ml/hr will you set the pump?
Rate (ml) = 5000 units x 500ml
Hr 1 hour 25,000 units
= 100 ml / Hr
An aminophylline infusion is running at 30ml/hr. There is 0.5g /
500ml. It should be running @ 12mg / hour. What is the infusion rate and what will you do to ensure it runs at the correct rate?
30 ml = Xmg x 500ml x 1g
1 hour Hour 0.5g
1000mg
X = 30 mg / hr
The drip should be running at 12 mg/hr
Thus need to reduce the rate to 12 ml/hr
(30mg: 12mg = 30ml:12ml)
2g of Kilabug is mixed up in 500ml of 5% dextrose. It is set to run at 5mg / min. What rate in ml/hr will you set the infusion pump?
Rate Xml = 5mg x 60 min x 500ml x 1g
Hr min 1 hr 2g 1000mg
Rate = 75ml /Hr
A patient is on a GTN infusion for pulmonary oedema. The infusion is made up of 50mg in 250ml 5% dextrose. It is presently running at 20ml/hr. How many mcg / minute is the patient receiving?
20 ml = X mcg x 250 ml x 60 min x 1mg
Hr min 50mg 1 hr 1000 mcg
= 66.7 mcg / min
A patient is started on an inotrope infusion for cardiogenic shock. The infusion is 750mg in 250ml N. saline. It is running at 5 ml/hr. The patient becomes increasingly hypotensive and his urine output is dropping off. The infusion rate is increased to 12ml/hr. The patient is 70Kg. What dose in mcg /
Kg/ min is the patient now receiving?
12ml = X mcg x 250ml x 70Kg x 60 min x 1mg
Hr min.Kg 750mg 1hr 1000 mcg
X = 8.6 mcg / Kg / min
A second patient who weighs 100Kg is on an inotrope infusion running at 10mcg/kg/min. You receive a pharmacy prepared bag with 1g in 500ml. At what rate (ml/hr) will you set the pump?
Rate ml = 10 mcg x 500 ml x 100Kg x 60 min x 1g x 1mg
Hr Kg.min 1g 1 hr 1000mg 1000mcg
= 30 ml / hr
Mr Jones ‘in extremis’
Mr Jones is a 60 year old man with known IHD. He is brought to A&E ‘in extemis’ (makes a change from an ambulance) after suddenly becoming short of breath whilst watching television. He is clinically and radiologically in severe pulmonary oedema.
He is electively ventilated and sent to ITU. He is started on
Frusemide 50mg/ml – running at 5mg/hr
Dobutamine 500mg in 250ml running at 8mcg / Kg.min
GTN 100mg in 500ml running at 20 mcg / Kg.min
He weighs 80 Kg. After one hour he is haemodynamically stable and his urine output is satisfactory.
(1)What rate is the GTN infusion running at in ml /hr?
(2)What rate is the dobutamine infusion running at in ml /hr?
Overnight he goes into fast AF and is started on an Amiodarone infusion. After the loading dose, he is started on 5mcg/kg/min. The infusion is 500mg in 50ml.
(3) What rate in ml/hr is the pump set out?
Mr Jones still unwell …
Overnight he goes into fast AF and is started on an Amiodarone infusion. After the loading dose, he is started on 5mcg/kg/min. The infusion is 500mg in 50ml.
(3) What rate in ml/hr is the infusion pump set out?
Despite the infusion he remains in fast AF and the SpR asks you to increase the infusion to 5ml/hr. However the ITU nurse tells you that the maximum dose of amiodarone is 12 mcg/kg.min.
(4) What is the maximum rate of the infusion?
Two days later he develops severe gram negative sepsis. He is started on a gentamicin infusion. The dose recommended by the microbiologist is 3mg/Kg.
The dose is made up in 50 ml D5W and is meant to run over 45 minutes.
(5) What rate (ml/hr) will you set the infusion rate?
You will need to show the workings for each calculation.
The answers are shown overleaf.
Mr Jones case - Answers
(1) 6 ml/hr
(2) 19.2ml/hr
(3) 2.4 ml / hr
(4) 5.8 ml/hr
(5) 66.7 ml/hr
Learning outcomes
At the end of this module you should now:-
Be aware of
• The difference between crystalloids and colloids
• The clinical indications for the different fluids
• The steps required in setting up an intravenous infusion
Be able to
• Prescribe fluids on a fluid chart
• Calculate the rate of a drip
• Calculate the rates and dosage of infusions
Recommended websites
www.wine1.sb.fsu.edu/chm1045/notes/Intro/Dimanal/Dimanal.htm
l www.-isu.indstate.edu/nurs/mary/mathprac.htm
l www.classes.kumc.edu/son/nurs420/CalculatingDrugDosages.html
www.cs.jcu.edu.au/~michael/web/Sections6.html