NEUROLOGICAL SYMPTOMS:
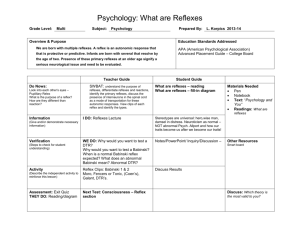
advertisement

NEUROLOGICAL SYMPTOMS: A good neurological history can be very revealing. Important aspects are time of onset, frequency of event, time course of symptoms (e.g. does it gradually or suddenly get worse) The prime symptom topics are shown, not all are fully discussed, but you can amplify these yourselves!) HEADACHE: o Can be Primary or Secondary: o MIGRAINE HEADACHE: Often preceded by aura, and associated with weakness, numbness, and paraesthesias. o TENSION HEADACHE: Usually is frontal or occipital. Tends to be recurrent. o CLUSTER HEADACHE: In males, occurring at night, 2-3 hours after falling asleep. Symptoms are intense unilateral orbital pain (over one eye), with lacrimation, rhinorrhoea, flushing. Usually lasts about 1 hour. o CAUSES of SECONDARY HEADACHE: o Meningismus: Stiff neck. If it occurs with the "worst headache of my life," then you should be suspicious of subarachnoid haemorrhage. Projectile Vomiting: Headache with projectile vomiting, occurring in morning, usually means increased intracranial pressure. Transient loss of Consciousness: Headache accompanied by transient loss of consciousness should raise question of stroke. SYNCOPE and LOSS of CONSCIOUSNESS: SEIZURES: o Types of Seizures: o Complex Partial Seizures: Patients commonly have feelings of fear or déja vu associated with complex partial seizures. Grand Mal Seizures: Tonic-clonic, often with loss of autonomic control. Petit Mal Seizures: Lasting for a short period of time -- only a few seconds. o CAUSES of SEIZURE: o Adolescents (12-20): Idiopathic (Epilepsy), Trauma, Drug and alcohol withdrawal Young Adults (20-35): Trauma, alcoholism, brain tumour Older adults (35+): brain tumour, CVA, metabolic disorders, electrolyte imbalances (hyponatraemia, hypoglycaemia, uraemia). CHANGES in VISION: o Homonymous hemianopia occurs with certain strokes o Bitemporal hemianopia occurs with pituitary tumour o Amaurosis Fugax: Transient, painless loss of vision in one eye, due to ischaemic changes in retina. Usually due to carotid artery stenosis or some form of retinal artery occlusion. o Other symptoms, such as weakness, paraesthesias, often accompany the Amaurosis Fugax. o Retrobulbar Neuritis: Occurs in Multiple Sclerosis and may cause transient loss of vision in one eye. CHANGES in HEARING: o Tinnitus o Deafness CHANGES in SPEECH: o o Dysphonia: Difficulty speaking due to impaired phonation ability. Dysarthria: Difficulty in articulating words. Can occur with weakness of tongue and oropharynx in stroke, Parkinson’s. o Aphasia: Inability to produce (motor aphasia) or understand (receptive aphasia) meaningful speech. PARALYSIS or WEAKNESS: o Paralysis complete loss of function o Paresis is intermittent or incomplete weakness. o CAUSES of Paresis: o Transient ischaemic attacks (TIAs): Recurrent Transient weaknesses in an upper extremity, accompanied by numbness and paraesthesia. Myasthenia Gravis (fatigable weakness) Hypokalaemia can result in periodic paralysis. Peripheral neuropathies Polymyositis or dermatomyositis. NUMBNESS and PARAESTHESIA: o May be hemisensory loss in stroke or sensory inattention o Hypocalcaemia, hypomagnesaemia o Hyperventilation syndrome o Paraneoplastic syndrome. o Medications: isoniazid, metronidazole. o Vitamin B12 deficiency CHANGES in MOOD and SLEEP PATTERN: ALCOHOL and DRUG USE, SEXUAL HISTORY: o Sexual history: In the neurological exam, may inquire about it to evaluate risk of HIV encephalopathy. o Alcohol abuse manifests a lot of neurological symptoms (Wernicke’s encephalopathy, beriberi, peripheral neuropathies). NEUROLOGICAL EXAMINATION: ASSESSMENT of PERIPHERAL FUNCTION ASSESSMENT of MOTOR FUNCTION: Sometimes pluses and minuses can be used for even finer grading. This is important in stroke and peripheral nerve or root lesions. o 0: No contraction; paralysis o 1: Trace of contraction. o 2: Moves if gravity is eliminated. o 3: Moves against gravity. o 4: Moves against gravity and against some resistance. o 5: Normal strength. Motor Abnormalities: o Hysteria: To test whether weakness in the leg is from hysteria or is organic, put a hand on both limbs and have the patient lift one limb against the hand's resistance. o If the cause of motor weakness is organic, then examiner should feel the other leg move the opposite direction in compensation. If it is hysteria, then the other leg remains still. o Fasciculations: Twitchings in resting muscles. May be normal if they are occasional or precipitated by cold. They may be a sign of Amyotrophic Lateral Sclerosis (ALS) if they are accompanied by weakness. o Tics: Normal movements of muscle groups (such as winking or grinning) occurring involuntarily, as in Tourette's Syndrome. o Tetany: Involuntary muscle spasms. o Causes: Tetanus, hypocalcaemia, hypomagnesaemia, hyperventilation syndrome. Chvostek's Sign: Tap over facial nerve anterior to ear, and look for contraction of the facial muscles, especially shutting of eyes. Trousseau's Phenomenon: Inflate a blood-pressure cuff to systolic pressure and maintain for 1-2 minutes. Induction of carpal-pedal spasm indicates latent tetany. o Tremors: Oscillating movements caused by involuntary contractions of muscle groups. SENSORY EVALUATION o Peripheral Neuropathies tend to occur in hand-and-glove distribution -- at the distal ends of the extremities. o PAIN: Upon pinprick, patient may experience hypalgesia (reduced pain), hyperalgesia, or analgesia (no pain). o LIGHT TOUCH: o Hypaesthesia = Impaired light touch sensation. Also related to light-touch are hyperaesthesia, paraesthesia, and anaesthesia (no light touch). o Sensory Extinction or Sensory Inattention: In parietal lobe lesions, if you put a pinprick on both sides of the body of a patient simultaneously, the patient will not perceive the prick on the affected side of the lesion. If the pins are placed sequentially, then the patient still retains normal sensation on both sides. STEREOGNOSIS: Being able to identify objects with your eyes closed. CEREBELLAR FUNCTION: o Dysergia: Improper co-ordinated function of a muscle group. o Dysmetria: Inability to properly gauge the distance between two points. Tested with finger-to-nose movements. o Dysdiadochokinesia: Inability to do rapid alternating movements. o Scanning Speech: Prolonged separation of syllables, often seen with cerebellar dysfunction. o GAIT Disturbances: o Cerebellar Lesions: Central cerebellar lesion shows unsteady gait, but conventional cerebellar signs may be normal. Posterior Columns Lesions: Loss of proprioception results in unsteady gait when eyes are closed, but relatively normal gait when eyes are open. Festinating Gait: Parkinsonian gait, shuffling walk. o Romberg's Test: Patient can't maintain balance with legs tight together, with eyes closed. o Titubation: Body tremor when standing or walking, sign of cerebellar disease. REFLEXES: Deep Tendon Reflexes: o Upper Extremity: o Biceps Reflex: Elbow flexion. Triceps Reflex: Forearm extension. Brachioradialis Reflex: Tap distal radius ------> flexion and partial supination of the forearm. o Lower Extremity: o Patellar Reflex: Contraction of Quadriceps (strongest muscles in body) and extension of leg. Suprapatellar Reflex: Above the knee; same response. Achilles Reflex: Causes plantar-flexion of foot. Reflex grading: o 0: Complete absence o 1: Diminished o 2: Normal Reflex o 3: Hyperactive reflex o 4: Clonus present (remember to test for this). Superficial Reflexes: o Upper Abdominal: Ipsilateral contraction of abdominal muscles on the stroked side. o Lower Abdominal: Ipsilateral contraction of abdominal muscles on the stroked side. o Cremasteric: Stroke inner thigh ------> elevation of testes. Brainstem Reflexes: o Corneal Reflex o Pupillary Light Reflex o Gag Reflex Abnormal Reflexes: o Babinski Sign: Stroke bottom of the foot ------> fanning (eversion) of big toe. o Chaddock's Reflex: When the external malleolar skin area is irritated, extension of the great toe occurs in cases of organic disease of the corticospinal reflex paths. o Oppenheim's Sign: Scratch inner side of leg ------> extension of toes. Sign of cerebral irritation. o Gordon's Sign: Squeeze the calf muscles and note the response of the great toe. Fanning or extension is considered abnormal. o Hoffman's Sign: Flexion of the terminal phalanx of the thumb and of the second and third phalanges of one or more of the fingers when the volar surface of the terminal phalanx of the fingers is flicked. o It is significant for pyramidal tract disease when it is unilateral. If it is bilateral than the meaning is uncertain. Absence of Superficial Reflexes: Unilateral suppression of superficial reflexes often results from upper motor lesions subsequent to a CVA. Primitive Reflexes: Presence of primitive reflexes is often a sign of frontal lobe lesions. o Suck Reflex: Gently tap or rub the upper lift ------> elicit a reflexive sucking or puckering response. o Grasp Reflex: Stroke the patient's palm, causing him to grasp your fingers. A positive test occurs when the patient does not let go of your fingers. o Palmomental Sign: Rub the thenar eminence ------> elicit reflexive contraction of the muscles of the chin. CRANIAL NERVE EVALUATION: CN I: OLFACTORY o TEST: Have patient identify objects by smell. o ABNORMAL: o Head trauma with fracture of cribriform plate Neoplasm in anterior fossa: meningioma CN II: OPTIC o TEST: Visual acuity, fundoscopic exam o ABNORMAL: Lots of causes of blindness CN III: OCULOMOTOR o TEST: o Have patient move eyes through all fields of vision. Intact 3 rd nerve means that eyes can move medially, superiorly, and inferiorly. Pupillary Reflex: Check for pupillary response to light in same eye and contralateral eye. Ptosis: Ptosis may occur due to 3rd nerve palsy. o ABNORMAL: o Unilateral CN-III Palsy: Subarachnoid haemorrhage resulting from aneurysm, diabetes, atherosclerosis. Horner's Syndrome: Usually occurs from bronchogenic carcinoma (Pancoast Tumour) impinging on the Superior Cervical Ganglion. CN IV: TROCHLEAR o TEST: o ABNORMAL: CN V: TRIGEMINAL o TEST: o Sensory: Check corneal reflex. Test facial sensation with eyes closed. Motor: Have patient clench teeth and palpate masseter muscle. o ABNORMAL: o Lost Corneal Reflex: Tumour of the cerebellopontine angle. Tic Douloureux: Irritative lesions of the CN V sensory roots. Spasm of muscles of mastication: tetanus, adverse reaction to Phenothiazines. CN VI: ABDUCENS o TEST: Look laterally. o ABNORMAL: o Diabetes, atherosclerosis, increased ICP, neoplasm. CN VII: FACIAL o TEST: Have patient smile, blink, frown, wrinkle forehead. o ABNORMAL: Bell's Palsy o Central Lesion of VII: The supratrochlear muscles are spared, as they receive bilateral innervation from both facial nerves. Below the eyes, the contralateral side will be paralysed. Peripheral Lesion of VII: There is an entire facial hemiplegia, with the paralysis occurring on the contralateral side. CN VIII: VESTIBULOCOCHLEAR o TEST: Standard hearing and vestibular tests. o ABNORMAL: A variety of disorders CN IX: GLOSSOPHARYNGEAL o TEST: Have patient open mouth and say "Aaahhh." o ABNORMAL: See Vagus N. below. CN X: VAGUS o TEST: Have patient open mouth and say "Aaahhh." o ABNORMAL: o Aortic Aneurysm, Bronchogenic Carcinoma may damage the recurrent laryngeal nerve. Uvula will deviate toward the damaged side. CN XI: SPINAL ACCESSORY o TEST: Have patient shrug shoulders. o ABNORMAL: Polymyositis CN XII: HYPOGLOSSAL o TEST: Have patient stick out tongue. o ABNORMAL: MENTAL STATUS EXAM: STATE of CONSCIOUSNESS: The Glasgow Coma Scale ORIENTATION ABILITY to COOPERATE MOOD THOUGHT PROCESS MEMORY for RECENT and REMOTE EVENTS ABILITY to HANDLE CONCEPTS and PROVERBS PRACTICAL SKILLS SPEECH PROBLEMS and RECOGNITION of APHASIA Abbreviated Mental Test Score and MSQ - tests for memory PATIENTS with ABNORMAL NEUROLOGICAL STATUS: APPROACH to the STROKE PATIENT: APPROACH to the COMATOSE PATIENT: APPROACH to the DELIRIOUS PATIENT: APPROACH to the PATIENT with PERIPHERAL NEUROPATHY: APPROACH to the PATIENT with SIGNS of MENINGEAL IRRITATION: Glasgow Coma Scale Overview: The Glasgow coma scale is used to assess patients in coma. The initial score correlates with the severity of brain injury and prognosis. Glasgow coma scale = = (score for eye opening) + (score for best verbal response) + (score for best motor response) Eye Opening Score spontaneously 4 to verbal stimuli 3 to pain 2 never 1 Best Verbal Response Score oriented and converses 5 disoriented and converses 4 inappropriate words 3 incomprehensible sounds 2 no response 1 Best Motor Response Score obeys commands 6 localises pain 5 flexion withdrawal 4 abnormal flexion (decorticate rigidity) 3 extension (decerebrate rigidity) 2 no response 1 Interpretation: • maximum score is 15 which has the best prognosis • minimum score is 3 which has the worst prognosis • scores of 8 or above have a good chance for recovery o • scores of 3-5 are potentially fatal, especially if accompanied by fixed pupils or absent oculovestibular responses • young children may be nonverbal, requiring a modification of the coma scale for evaluation. Abbreviated Mental Test Overview: The Abbreviated Mental Test can be used to quickly test the cognitive function in elderly patients. This is also referred to as the Hodkinson's Mental Test Score. Item age Score 1 time to the nearest hour 1 year 1 name of place 1 recognition of 2 persons 1 birthday (date and month) 1 date of World War I 1 name of your country's Ruler, President or Prime Minister 1 able to count from 20 to 1 backwards 1 address - 42 West Street 1 Interpretation • minimum score: 0 • maximum score: 10 • a higher score indicates greater cognitive function • a score of 6 is used as the cut-off to separate normal elderly persons from those who are confused or demented with a correct assignment of 81.5% References: Jitapunkul S, Pillay I, Ebrahim S. The Abbreviated Mental Test: Its use and validity. Age Aging. 1991; 20: 332-336. Kalra L, Crome P. The role of prognostic scores in targeting stroke rehabilitation in elderly patients. J Am Geriatr Soc. 1993; 41: 396-400. Qureshi KN, Hodkinson HM. Evaluation of a ten-question mental test in the institutionalised elderly. Age Ageing. 1974; 3: 152-157. Vardon VM, Blessed G. Confusion ratings and abbreviated mental test performance: A comparison. Age Ageing. 1986; 15: 139-144. Mental Status Questionnaire Overview: The Mental Status Questionnaire can also be used to quickly test the cognitive function in elderly patients. This has similar roots to the Abbreviated Mental Test Score, but was developed in Scotland. Item Score Today's DATE 1 Today's MONTH 1 Today's YEAR 1 This TOWN 1 Present SITUATION 1 AGE 1 MONTH of BIRTH 1 YEAR of BIRTH 1 PRIME MINISTER 1 PREVIOUS PRIME MINISTER 1 Interpretation • minimum score: 0 • maximum score: 10 • a higher score indicates greater cognitive function • a score of 7 is used as the cut-off to separate normal elderly persons from those who are confused or References: