EMBRYOLOGY LECTURE. HUMN110. GAMETOGENESIS
advertisement

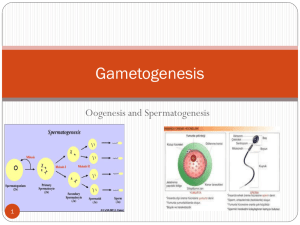
DEVELOPMENT 1 Dr. Farhat Aamir At the end of session, student should able to • Define and classify gametogenesis. • Identify and discuss the stages of gametogenesis. • Discuss morphological changes during maturation of gametes. • Identify clinical application i.e., formation of abnormal gametes. Gametogenesis • Gametes: derives from primordial germ cells. • Formed in epiblast during second week. • During fourth week, germ cells migrate towards developing gonads. • Germ cell undergo meiosis to reduce chromosome number. Gametogenesis • Definition: the process of forming gametes • Two types • Oogenesis in females Start dividing to form oogonia Divides to form primary oocyte • Spermatogenesis in males Oogenesis • Oogenesis is the process of formation of mature oocyte (or ovum). • Oogonia increase in number by rapid division. • By fifth month of prenatal life, it reach up to 7 million Oogenesis • By seven month, majority of oogonia degenerates. • The surviving primary oocyte enters in prophase of meiosis I • Primordial follicle: are primary oocyte surrounded by layer of flat epithelial cells Oogenesis • Primordial follicle remain arrested in prophase and do not finish their first meiotic division before puberty is reached. • Controlled by oocyte maturation inhibitor secreted by follicular cells. • At birth number of primary oocyte are 600,000800,000. • 500 oocyte reach up to puberty. Oogenesis • Primary follicle: conversion of squamous granulosa cells to cuboidal cells More than one layer Zona pellucida: layer of glycoprotein surrounding oocyte. Oogenesis • Antral/vesicular follicle: Theca externa Outer layer Fibrous capsule Theca interna Inner layer Secretory cells Appearance of fluid filled spaces All these spaces join together to form antral cavity Mature vesicular/Graffian follicle • Corona radiata: Granulosa cells surrounding oocyte • Cumulus oophorus • 25mm or more in diameter • Well developed theca externa and interna Oogenesis • A surge in LH hormone induce preovulatory growth • Meiosis I is completed Formation of two daughter cells Secondary oocyte and polar body Cell arrested in metaphase of meiosis 2 It will complete at the time of fertilization Spermatogenesis • It starts at puberty • Events in which spermatogonia are transformed into spermatozoa. • During puberty, PGC give rise to spermatogonial stem cells • Further, they form type A spermatogonia • Sertoli cells are supporting cells Spermatogenesis • Spermatocytes and spermatid remain inside sertoli cells • Sertoli cells supports, protect and help in releasing mature spermatozoa • FSH and LH help in spermatogeneis Spermiogenesis • Defined as series of changes resulting in the transformation of spermatids into spermatozoa 1. Formation of acrosome 2. Condensation of nucleus 3. Formation of neck, middle piece and tail 4. Shedding of cytoplasm by sertoli cells • Time span of 74 days Clinical correlations • Teratoma are tumors having bone, hair, muscle, tooth and epithelia • PGC may choose irregular path can give rise to teratoma Clinical correlations • Abnormal germ cells • Primordial follicle with two oocyte • Some times, primary oocyte contain two or three nucleus • These binucleated or trinucleated oocyte dies before maturity Clinical correlations • 10 % of spermatozoa usually have defects. • Head and tail may be abnormal. • Sometimes, gaint and dwarf. • It lacks normal mobility and do not fertilize with oocyte References • Langman’s: A text book of medical embryology.