SPINAL CORD INJURY
advertisement

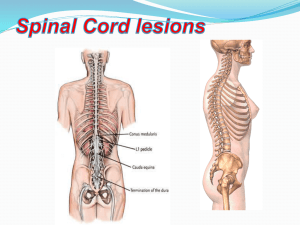
SPINAL CORD INJURY Spinal Cord Injury is damage to the spinal cord that results in a loss of function such as mobility or feeling. Frequent causes of damage are trauma and disease Clinical syndromes Central cord syndrome: hyperextension(common) Anterior spinal artery syndrome: flexion Loss of motor function, pain and temperature are lost Brown sequard syndrome: gun shot or stab wound causing injury to half of spinal cord More impairment in upper limb than lower limb Ipsilateral motor and position sense and contralateral pain is lost. Posterior cord syndrome: injury to posterior spinal artery all sensation of posterior column is lost. (rare) Spinal Cord Paralysis Levels C1-C3 All daily functions must be totally assisted Breathing is dependant on a ventilator Motorised wheelchair controlled by sip and puff or chin movements is required C4 Same as C1-C3 except breathing can be done without a ventilator C5 Good head, neck, shoulder movements, as well as elbow flexion Electric wheelchair, or manual for short distances C6 Wrist extension movements are good Assistance needed for dressing, and transitions from bed to chair and car may also need assistance C7-C8 All hand movements Ability to dress, eat, drive, do transfers, and do upper body washes Spinal Cord Paralysis Levels T1-T4 (paraplegia) Normal communication skills Help may only be needed for heavy household work or loading wheelchair into car T5-T9 Manual wheelchair for everyday living Independent for personal care T10-L1 Partial paralysis of lower body L2-S5 Some knee, hip and foot movements with possible slow difficult walking with assistance or aids Only heavy home maintenance and hard cleaning will need assistance Medical management Pharmacological management: methyleprednisolone Surgical stabilization: Phrenic nerve pacing electric stimulation of phrenic nerve – above C3 lesion Gardener wells tongs – 5 ponds (cervical) Hard collar (Philadelphia collar) or SOMI (sterno-occipital mandibular immobilizer) 6-8 weeks for bony fusion Halo is used when surgery is not needed Cervical stabilsation Philadelphia collar Halo Thoracolumbar stabilisation Jewett brace EXAMINATION History: demographic data , level of activity. Systemic review: vitals. Aerobic capacity and endurance: autonomic response to position change. Anthropometric measurements. Adaptive devices. Skin examination. Motor examination. Joint mobility. Flexibility of essential muscles. Pain Posture Reflex integrity. Functional independence measure. Respiratory system. INTERVENTION Prevention and management of joint contractures Tenodesis grasp Hamstring Shoulder rotators Prevention and management of respiratory complications Inspiratory muscle training Gentle pressure diaphragm and ,intercostals Glossopharyngeal breathing Secretion clearance Quad coughing Early mobilization Orthostatic hypotension Abdominal binders. Upright position as soon the fracture is stable Bladder management Reflex bladder - low pressure voiding Nonreflex bladder- intermittent catheterization Home management Bed mobility Pressure relief Wheel chair transfer