Present 9
advertisement

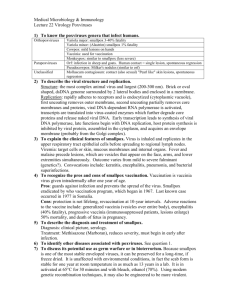
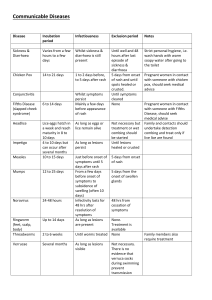
Rash Illness Paige Jordan RN, BSN Region II Epidemiologist Objectives Describe the public health action required to respond to a suspected case of smallpox Describe the epidemiology, mode of transmission and presenting symptoms of papulovesicular rashes Describe the differential diagnosis of papulovasicular rashes and other diseases of public health significance Describe how to use the Diagnostic Algorithm for evaluation of rash illness Describe the laboratory diagnosis of papulovasicular rashes Public Health Significance Smallpox eradicated in 1970’s. Heightened concern that the variola virus might be used as an agent of bioterrorism. Ruling out rash illnesses facilitates the diagnosis/confirmation of smallpox Many rash illnesses of public health significance require ruling out other differential diagnosis A good understanding of rash illnesses allows for early identification, diagnosis, treatment, control and prevention of disease. Public Health Action Identify personnel to respond to a suspected case of smallpox. Personnel must have: Documented immunity to smallpox Unvaccinated personnel : - Fit tested N 95 mask - No contraindication to smallpox vaccination Documented immunity to measles, rubella and varicella Completed training in smallpox investigation & response Public Health Action Educate providers to immediately isolate undiagnosed hospital patients with acute, generalized vesicular or pustular rash illness, to include: Airborne precautions Contact precautions Notification of the ICP Public Health Action Educate providers to recognize major and minor smallpox diagnostic criteria , as follows Major Criteria Febrile prodrome: occurring 1-4 days before rash onset: fever >101°F and at least one of the following: prostration, headache, backache, chills, vomiting or severe abdominal pain. Classic smallpox lesions: deep-seated, firm/hard, round, well-circumscribed vesicles or pustules; may be umbilicated or confluent. Lesions in the same stage of development: on any one part of the body (e.g., the face, or arm) all the lesions are in the same stage of development (i.e. all are vesicles, or all are pustules). Public Health Action Minor Criteria Centrifugal distribution: greatest concentration of lesions on face and distal extremities First lesions on the oral mucosa/palate, face, forearms Patient appears toxic or moribund Slow evolution: lesions evolve from macules to papules pustules over days (each stage lasts 1-2 days) Lesions on the palms and soles (majority of cases) Public Health Action Educate hospitals to report immediately cases of : Acute febrile pustular or vesicular rash illness immediately Educate hospitals to report hospitalized cases of varicella immediately Public Health Action Triage reports of pustular/ vesicular rash illness according to CDC criteria, as follows: High risk Moderate risk Febrile prodrome AND Classic smallpox lesions AND Lesions in same stage of development Febrile prodrome AND 1 major OR >=4 minor criteria Low risk No/mild febrile prodrome Febrile prodrome and < 4 minor criteria Rash Illness Algorithm Goal Evaluation of cases Classification of cases into risk categories according to major & minor criteria Assumptions / Limitations - Will miss the first case of smallpox until day 4-5 (by excluding maculo-papular rashes) - Will miss an atypical case of smallpox (hemorrhagic, flat/velvety or highly modified) if it is the first case. Patient with Acute, Generalized Vesicular or Pustular Rash Illness Institute Airborne & Contact Precautions Alert Infection Control on Admission Low Risk for Smallpox Moderate Risk of Smallpox High Risk for Smallpox (see criteria below) (see criteria below) (see criteria below) ID and/or Derm Consultation VZV +/- Other Lab Testing as indicated ID and/or Derm Consultation Alert Infx Control & Local and State Health Depts History and Exam Highly Suggestive of Varicella Diagnosis Uncertain Varicella Testing Optional Test for VZV and Other Conditions as Indicated Non-Smallpox Diagnosis Confirmed Report Results to Infx Control Evaluating Patients for Smallpox No Diagnosis Made Ensure Adequacy of Specimen ID or Derm Consultant Re-Evaluates Patient Smallpox Response Team Collects Specimens and Advises on Management Cannot R/O Smallpox Contact Local/State Health Dept Testing at CDC NOT Smallpox Further Testing SMALLPOX Public Health Action High Risk of Smallpox Report Immediately Contact IDEP emergently to arrange smallpox testing through CDC Consider infectious disease and/or dermatology consultation Consider testing for chickenpox, if appropriate Clinical and epidemiological data may be collected using the vesicular rash illness form If a specific disease is diagnosed, use the investigation form for that disease. Consider active surveillance for vesicular/pustular rash illness in hospitals and emergency rooms. Public Health Action Moderate Risk of Smallpox Urgent Evaluation Consider dermatology and/or infectious disease consultation Consider testing for chickenpox (DFA) Clinical and epidemiological data may be collected using the vesicular rash illness form If a specific disease is diagnosed, use the investigation form for that disease Recommend additional testing, if indicated Public Health Action Low Risk of Smallpox Manage as Clinically Indicated Consider testing for chickenpox (DFA), if appropriate. Contact IDEP to arrange Clinical and epidemiological data may be collected using the vesicular rash illness form If a specific disease is diagnosed, use the investigation form for that disease Public Health Action Assure collection of appropriate clinical samples for testing Smallpox Chickenpox Measles Herpes simples Monkeypox Rickettsialpox On confirmation of a specific diagnosis, refer to disease specific protocol for public health action. Investigating Tool IDEP’s case investigation worksheet for investigation of febrile vesicular or pustular rash illnesses SMALLPOX Single confirmed case is an international public health emergency Etiology Variola Virus (Orthopoxvirus) Infects only Humans May remain viable in crusts for years at room temperature Rapidly inactivated by UV light, chemical disinfectants Epidemiology All ages and genders affected Incubation 12 days (range 10-14 days) Spread Person-to-person transmission: Droplets > Contact with contaminated clothing and bedding > Aerosol Infectious Period: From the time the rash appears - particularly in the first week of illness - until the scabs fall off. Smallpox Signs & Symptoms Signs & symptoms Fever, malaise, headache, abdominal pain, delirium Rash, pustules, toxemia, secondary bacterial infections, death 5-6 days after rash Survivors usually have deeply scarred face. Clinical Features Three stages of disease Incubation Asymptomatic Prodromal Nonspecific febrile illness, flu-like (may be misdiagnosed or ignored) Eruptive Characteristic rash Clinical Features Incubation Stage (From time of infection to onset of symptoms) Average 12 days (range 10-14 days) Problem for epidemiological investigation and control (e.g., quarantine) of carriers & exposed No symptoms Considered non-infectious during this stage Clinical Features Prodromal Stage Occurs 1-4 days before rash onset End of stage marked by mucosal (mouth) lesions Mucosal lesions indicate onset of infectiousness Common symptoms Abrupt onset of fever > = 101 F Weakness, headache, backache Occasional symptoms Nausea, vomiting, abdominal pain, delirium Clinical Features Eruptive Stage (Rash) “Centrifugal” (in order of appearance & severity) Initially oral mucosa Occurs 1-4 days before rash onset Face, head Forearms, hands, palms Legs, soles, (sometimes less so on trunk) Clinical Features Rash Description Enanthem (mucous membrane lesions) Appears approx. 24 hours before skin rash Minute red spots on the tongue and oral/pharyngeal mucosa Lesions enlarge and ulcerate quickly May result in complaint of sore throat Virus titers in saliva are highest during first week of exanthem Clinical Features Rash Description Exanthem (skin rash) Appears 2-4 days after onset of fever First appears as macules, usually on the face Lesions appear on proximal extremities, spread to distal extremities and trunk. Clinical Features Rash Description Classic Smallpox Lesions Vesicles often have a central depression (“umbilication”) Pustules raised, round, firm to touch, deeply embedded in the skin Lesions in same stage of development Most dense on face and distal extremities (centrifugal distribution) Lesions on palms and soles (>=50% cases) Smallpox Clinical Course Smallpox Rash Evolution Stage Days after Rash onset Macules Papules Vesicles Pustules Crusts All crusts separated 0-1 2-3 3-5 6-12 13-20 21-28 Understanding the terms (Illustration by Electronic Illustrators Group.) http://www.hendrickhealth.org/healthy/001267.htm Rash Evolution World Health Organization (WHO) SMALLPOX - RASH PROGRESSION Day 1 Day 2 Day 3 Few raised spots (papules) More papules appear Rash more distinct fluid accum. to form vesicles World Health Organization (WHO) SMALLPOX - RASH PROGRESSION Day 4 Day 5 Day 7 Vesicles more distinct Fluid in vesicles Rash characteristic becomes of cloudy to form smallpox no mistake pustules in diagnosis World Health Organization (WHO) SMALLPOX - RASH PROGRESSION Day 8 & 9 Day 10-14 Day 20 Pustules increase in size Firm and deeply embedded Pustules dry up to form dark scabs Scabs have come off revealing depigmented areas World Health Organization (WHO) Smallpox Rash - Distribution Smallpox Rash - Distribution World Health Organization (WHO) Smallpox Rash - Distribution World Health Organization (WHO) Smallpox Rash - Distribution World Health Organization (WHO) Smallpox Clinical Types Ordinary smallpox: 90% of cases Case-fatality average 30% Occurs in non-immunized persons Modified smallpox Milder, rarely fatal Occurs in 25% of previously immunized persons and 2% of non-immunized persons Fewer, smaller,more superficial lesions that evolve more rapidly Smallpox Clinical Types Hemorrhagic smallpox: <3% of cases Immunocompromised persons and pregnant women at risk Shortened incubation period, severe prodrome Dusky erythema followed by petechiae & hemorrhages into skin and mucous membranes Almost uniformly fatal within 7 days Hemorrhagic Smallpox Smallpox Clinical Types Malignant or flat-type smallpox: 7% of cases Slowly evolving lesions that coalesce without forming pustules Associated with cell-mediated immune deficiency Usually fatal Smallpox – No Rash (Variola sine eruptione) Occurs in previously vaccinated persons or infants with maternal antibodies Asymptomatic or mild illness Transmission from these cases has not been documented Malignant Smallpox Thomas, D. Smallpox Laboratory Testing Specimens Fluid from vesicles, pustules, or scabs Autopsy specimens from major organs including skin, spleen, lymph node, liver, lung, kidney, and heart Tonsillar tissue Blood Laboratory Criteria for Diagnosis of Smallpox Isolation of smallpox virus from a clinical specimen (level D lab only) PCR identification of Variola DNA in a clinical specimen, or Negative stain Electron Microscopy identification of Variola virus in a clinical specimen (level D lab or approved level C lab) Smallpox Surveillance Clinical Case Definition An illness with acute onset of fever > 101o F followed by a rash characterized by firm, deep-seated vesicles or pustules in the same stage of development without other apparent cause Laboratory criteria for confirmation Isolation of smallpox virus from a clinical specimen, OR Identification of variola in a clinical specimen by PCR or electron microscopy * Initial confirmation of outbreak requires testing in level D lab (I.e CDC) Smallpox Surveillance Case classification Confirmed: laboratory confirmed Probable: meets clinical case definition & has an epi link to another confirmed or probable case Suspected: Meets clinical case definition but is not laboratoryconfirmed and does not have an epi link OR Atypical presentation not lab confirmed but has an epi link to a confirmed or probable case Common Conditions With Vesicular or Pustular Rashes Varicella (primary infection with VZV) Disseminated herpes zoster Impetigo Drug eruptions and contact dermatitis Erythema multiforme minor Erythema multiforme incl. Stevens Johnson syndrome Enteroviruses incl. Hand, Foot and Mouth disease Disseminated herpes simplex Scabies and insect bites Molluscum contagiosum CHICKENPOX (VARICELLA) Varicella Is the disease most likely to be confused with smallpox Chickenpox Epidemiology Incubation: 14-16 days (range 10-21 days) Spread: Person to person by direct contact with patients with : Varicella or Zoster lesions Airborne spread from respiratory secretions Infectious Period: two days before the onset of the rash, until all of the lesions are crusted over Chickenpox Epidemiology Etiology: Varicella Zoster Virus VZV Reservoir: Humans are the only source of infection Seasonality: Seasonal transmission of disease highest during winter and early spring Chickenpox Clinical Features Fever and malaise usually mild in children and more severe in adults A pruritic skin rash most prominent on chest, back, shoulders, scalp, or other areas Lesions on the mouth, vagina, rectum, eye, or other mucous membranes changes to fluid-filled blisters Crusting, after the blister breaks Crusts become progressively darker with time Scabs fall off in about 9 to 13 days Itching-- may be severe Chickenpox Clinical Features Prodrome: 0-1 day of fever, anorexia, headache Rash: Begins on face and scalp Spreading inferiorly to trunk and extremities Palms and soles usually spared Scabs form as early as day 3 or 4 of rash; fall off by day 14 Enanthem: Vesicles and shallow erosions most commonly on the hard palate, but also on nasal mucosa, conjunctiva, pharynx, larynx, GI tract, urinary tract, vagina Exanthem: Macules, papules, vesicles, crusts in various stages of evolution Chickenpox Clinical Features Chickenpox on the palate. Glistening, water-drop characteristic of the chickenpox vesicle on the palate. . Chickenpox Clinical Features Chickenpox vesicle behind the ear. Classic "dew drop on a rose petal" appearance. Chickenpox Clinical Features © 2001, Johns Hopkins University School of Medicine Chickenpox Rash Classic Chickenpox Rash Superficial lesions Not well circumscribed Confluence and umblication uncommon Lesions at all stages of development Chickenpox Rash Evolution Stages Macules Papules Vesicles Crusts Rapid evolution of macules to papules, vesicles, crusts All stages simultaneously present Lesions superficial, distribution centripetal Scabs fall off in 9-13 days Differentiating Features Chickenpox Vs Smallpox Distinguishing Smallpox from Chickenpox Epi Features that Differ Smallpox (variola) Most of the population expected to be susceptible Chickenpox (varicella) Most cases occur in children Expected case fatality rate 2-3/100,000 Secondary attack rate of 80% among susceptible household contacts Expected case fatality rate averages 30% Secondary attack rate ~60% in unvaccinated family contacts Distinguishing Smallpox from Chickenpox Clinical Features that Differ SMALLPOX FEVER 2-4 DAYS BEFORE RASH RASH SAME STAGE Appearance Development SLOW CHICKENPOX AT TIME OF RASH DIFFERENT STAGES RAPID Distribution MORE ON ARMS & LEGS MORE ON BODY On palms & USUALLY PRESENT soles USUALLY ABSENT > 10% VERY UNCOMMON DEATH Distinguishing Smallpox from Chickenpox Clinical Features that Differ Classic Smallpox lesion Classic Chickenpox lesion “Dew drops on a rose petal” Rash Distribution Rash Distribution Smallpox Chickenpox Content Provider: CDC/Dr. John Noble, Jr. Rash Distribution Chickenpox - More pocks on the trunk Very Few on arms and hands - Pocks different stages of development Smallpox More pocks on face arms and thighs - Pocks same stage of development Rash Distribution Chickenpox No or few lesions on the hands Smallpox Pocks usually present on the palms of the hands Rash Distribution Smallpox Many lesions on the soles Chickenpox Few of no lesions Rash Distribution Rash Distribution Smallpox Chickenpox Rash Distribution Smallpox Chickenpox Rash Distribution Smallpox Rash same stage of development Chickenpox Several stages of rash (papules, vesicles & pustules) Rash Distribution Smallpox Scabs not yet formed Chickenpox Most lesions scabbed Rash Distribution Smallpox Scabs beginning to form Chickenpox Most scabs fallen off Chickenpox Diagnosis Rapid diagnostic testing for varicella zoster virus (DFA, IFA, PCR) Laboratory Specimens for Diagnosis Swab sample from the base of a skin lesion preferably fresh fluid vesicle HERPES ZOSTER (Shingles) A painful involvement of cutaneous nerves resulting from a reactivation of a dormant varicella zoster virus Herpes Zoster Epidemiology Etiology DNA virus belonging to herpes group. Same virus that transmits the chicken pox. Reactivation of varicella infection Incubation: There may be latent period of decades before the virus is reactivated and start spreading along cutaneous nerves. Spread: There is no convincing evidence that shingles can be contracted from another individual. The virus remains dormant in dorsal root or cranial nerve ganglion after the patient recovers from chicken pox. Herpes Zoster Epidemiology No airborne droplet spread from cases of shingles. Direct contact with the blister fluid can cause chickenpox in a non immune person. Immunosuppressed individuals - at more risk. More common in the elderly. The trigeminal nerve is most commonly involved cranial nerve. Overall the thoracic is the most commonly affected. Herpes Zoster Clinical Features Prodrome: Neuritic pain or paresthesia for 2-3 weeks Physical examination reveals an eruption, which is limited to one side of the body and corresponds to a dermatome. What is a Dermatome? American Accreditation HealthCare Commission (www.urac.org). Herpes Zoster Rash Rash Painful papulovesicular rash Stages of Rash Red macule Papule Vesicle surrounded by erythema. The individual vesicles may become confluent and evolve over the next 2-3 weeks to become pustular, haemorrhagic and finally scabbed. Crust formation: days to 2-3 weeks; post-herpetic neuralgia:months to years www.niaid.nih.gov/shingles Herpes Zoster Vesicle Herpes zoster on the arm. - Characteristic grouping of vesicles Herpes Zoster Shingles affecting the left side of the chest of an adult male. - The dermatomes involved are T6 and T7. Herpes Zoster HERPES ZOSTER ON THE FACE Dermatomal distribution of the papules, vesicles, and pustules. •Groups of vesicles arranged along the distribution of a cranial or spinal nerve •Cutaneous and visceral dissemination from the original dermatome develops in some individuals, particularly immunocompromised patients •Associated with localized or referred pain Distinguishing Smallpox from Herpes Zoster Clinical Features that Differ HERPES ZOSTER SMALLPOX Lesions are unilaterally distributed along a dermatome Lesions are widely distributed Lesions at any given time are in different stages of development (vesicles, pustules, and crusts are in evidence at one time) Lesions at any given time are all at the same stage of development Associated with severe constitutional symptoms Herpes Zoster Laboratory Diagnosis Rapid diagnostic tests for Herpes Zoster Virus Direct Fluorescent Antibody (DFA) - Very sensitive and specific - Critically dependent on careful collection of material from a lesion Specimen: Vesicle scraping Polymerase chain reaction Specimen: body fluid or tissue What is Herpes? Herpes is a common viral infection. It causes oral herpes (cold sores or fever blisters), and genital herpes (genital sores). There are two herpes simplex viruses: •Herpes Simplex Type 1 (HSV-1) •Herpes Simplex Type 2 (HSV-2) These viruses look identical under the microscope, and either type can infect the mouth or genitals. Most commonly, however, HSV-1 occurs above the waist, and HSV-2 below. GENITAL HERPES Genital herpes is a contagious viral infection affecting primarily the genitals of men and women. It is characterized by recurrent clusters of vesicles and lesions at the genital areas. It is caused by the Herpes Simplex-2 virus (HSV-2), one of several strains of the Herpes Simplex Virus responsible for chickenpox, shingles, mononucleosis, and oral herpes (fever blisters or cold sores, HSV-1). While generally not dangerous, it is a nuisance and can be emotionally traumatic, as there is no cure. It has reached epidemic proportions in the U.S.; 500,000 are diagnosed each year. One in five American adults has herpes, but only one third of those inflicted are aware that they have the virus. Many people don’t relate their symptoms to herpes, since they have either very mild or no symptoms at all. Over 50 million cases are currently estimated to exist in either the active or dormant stage. Eczema herpeticum (ulcers are of similar shape and size) “The key physical sign of eczema herpeticum is blisters, pustules, or erosions of a rather uniform size and appearance” Frequency of Adverse Events Following Primary Smallpox Vaccination with New York Board of Health Strain Vaccinia, by Age and Type of Adverse Event Expected Number of Adverse Events Per Million Vaccines Age at Vaccination <1 1-4 5-19 20+ 5 0.5 0-5 5 (?) Post-vaccinial encephalitis 6 2 3 4 Progressive vaccinia 1 0.5 1 10 + (?) Eczema vaccinatum 14 44 35 30 Generalized rashes 400 9,600 140 250 Accidental implantation 507 577 371 606 Type of Adverse Event Death (all causes) Eczema vaccinatum Eczema vaccinatum is a serious complication that occurs when people with eczema or atopic dermatitis get vaccinated. The lesion spreads to skin that is currently affected or has recently been affected by eczema. This complication can occur even if the eczema or atopic dermatitis is not active at the time, and requires immediate medical attention. Prior to 1960, eczema vaccinatum occurred in 10 to 39 people per 1 million people vaccinated. Vaccine Immune Globulin (VIG) is felt to be a useful treatment for eczema vaccinatum. Eczema vaccinatum Eczema vaccinatum is characterized by widespread vaccinial lesions over the body of patients with eczema or a history of eczema. These patients are clinically similar to burn patients, losing fluid, serous exudate, and electrolytes through their skin. Fatalities often occurred in patients who were not themselves vaccinated, but were close household contacts of recently vaccinated siblings etc. Many patients with eczema have perfectly normal vaccination responses; there are no data to show what proportion of eczema patients develop serious disease, but it is probably considerably less than half. While patients with other widespread skin disease can get superinfection of their rashes, they do not develop the extensive involvement found with occasional eczema patients, and essentially never die. Vigorous therapy with VIG and good supportive care reduced the fatality rate from about 10% in the pre-VIG era, to only about 1%. Eczema vaccinatum •In the past, it was estimated to occur in 10-39 per million primary vaccinees.* Rates in the United States today may be higher because there may be more persons Eczema vaccinatum is a localized or systemic spread of vaccinia virus. •at risk from 1) immune suppression from cancer, cancer therapy, organ transplantation, and other illnesses, such as HIV/AIDS, and 2) eczema or atopic dermatitis. Rates may be lower for persons previously vaccinated •Transfer of vaccinia virus can occur from autoinoculation or from contact with a vaccinee whose lesion is in the florid stages. •Individuals with eczema or atopic dermatitis are at increased risk. Eczema vaccinatum can occur regardless of whether the eczema/atopic dermatitis is active at the time of vaccination •Virus implanted in disrupted skin (may be at multiple sites) spreads from cell to cell producing extensive lesions dependent on extent of abnormal skin. •Treatment should include hospitalization and urgent treatment with VIG. Mortality has been prevented in patients treated promptly and adequately. •Severe cases and fatalities have been observed after contact of recently vaccinated persons with persons who have active eczema/atopic dermatitis or a history of eczema/atopic dermatitis. Eczema vaccinatum. Eczema vaccinatum. Eczema vaccinatum in contact to recently vaccinated child. Recovered without sequelae or permanent ocular damage. Eczema vaccinatum in an unvaccinated contact to a vaccinated sibling. [from Fenner F., Henderson DA, et al. Smallpox and its Eradication. WHO. 1988]. Generalized vaccinia •Generalized vaccinia consists of vesicles or pustules appearing on normal skin distant from the vaccination site. •In the past, it was estimated to occur in 242 per million primary vaccinees. •It is believed to result from a vaccinia viremia with skin manifestations. •Most rashes labeled as generalized vaccinia produce only minor illness with little residual damage. •The rash is generally self-limited and usually requires only supportive therapy. However, patients with underlying immunosuppressed illnesses may have a toxic course and require Vaccinia Immune Globulin (VIG). Generalized vaccinia in an apparently normal child. Recovered without sequelae. Accidental implantations or Autoinocculation This child touched his inoculation site and inoculated his lower lid with vaccinia virus . More common, but of less concern are accidental implantations, erythematous or urticarial rashes, and “generalized vaccinia.” Accidental implantation occurs when a patient scratches his/her vaccination site, and then scratches an eye, the anus or genitals, or another skin disorder such as poison ivy. This creates a coprimary lesion distant from the intended vaccination site. When vaccinia infects the eye, care must be taken to examine for keratitis. About 6% of patients with vaccinia in the eye develop vaccinial keratitis; VIG is contraindicated in such patients, because they may get antigen-antibody precipitates in the cornea causing scarring. Inadvertent Inoculation •Successful vaccination produces a lesion at the vaccination site. Beginning about four days after vaccination, the florid site contains high titers of vaccinia virus. This surface is easily transferred to the hands and to fomites, especially since itching is a common part of the local reaction. •Accidental implantation occurs due to transfer of vaccinia virus from the primary site to other parts of the body, or to other individuals. •This is the most frequent complication of smallpox vaccination (529 per million primary vaccinees), accounting for approximately half of all complications of primary vaccination and revaccination. •Lesions of inadvertent inoculation can occur anywhere on the body, but the most common sites are the face, eyelid, nose, mouth, genitalia, and rectum. Lesions in eczematous skin, in disrupted skin and in the eye pose special hazards, as the infection can be extensive in skin lesions and a threat to eyesight in the eye. •Most lesions heal without specific treatment Vaccinia keratitis •Vaccinia keratitis results in lesions of the cornea due to accidental implantation of vaccinia virus, and is potentially threatening to eyesight. •Symptoms appear ten days after transfer of vaccinia virus. •Left untreated, considerable corneal scarring may result as lesion heals resulting in significant impairment of vision. •Topical antiviral agents are the treatment of choice; therapy should be determined in immediate consultation with an experienced ophthalmologist. Progressive vaccinia •Progressive vaccinia, also known as vaccinia necrosum, is a severe, potentially fatal illness characterized by progressive necrosis in the area of vaccination, often with metastatic lesions (e.g., lesions at places other than the vaccination site). •In the past, it was estimated that progressive vaccinia occurred in approximately 1 to 2 per million primary vaccinations, and was almost always fatal before the introduction of VIG and antiviral agents. •Rare in the past, it may be a greater threat today, given the larger proportion of susceptible persons in the population and the greater number with immunocompromise. Nearly all instances have been in people with defined cell-mediated immune defect (T-cell deficiency). •Prompt hospitalization and aggressive use of VIG are required. •Massive doses of VIG are necessary to control viremia. Up to 10 ml per kg of intramuscular VIG has been used. •There is no proven antiviral therapy. Preliminary studies with cidofovir show some antiviral effect in vitro; studies in animals are pending. •Immediate consultation with the CDC is recommended to determine if any experimental antiviral drugs are available. Electronic sources of dermatological information Dermatology Online Journal tray.dermatology.uiowa.edu/home.html Internet Dermatology Society RxDerm-L Tumours of the skin, University of California at Davis Dermatology online atlas Dermatology atlas www.telemedicine.org listpro@ucdavis.edu (email) matrix.ucdavis.edu/tumors/tradition/tumors .html www.derma.med.unierlangen.de/index_e.htm www.meddean.luc.edu/lumen/medEd/medici ne/dermatology/melton/atlas.htm Skin cancer and benign tumor image atlas www.meddean.luc.edu/lumen/medEd/medici ne/dermatology/content.htm Dermatology image bank www.tmc.edu.tw/medimage/derma_bank/def ault_eng.htm www.telemedicine.org/contact.htm www.dermnet.org.nz/dna2a.html erl.pathology.iupui.edu/cases/dermcases/der mcases.cfm www.skindex. Contact dermatitis DermNet (atlas and information) Virtual Dermatology (case directory) Skindex-case directory (news, reviews, treatment trends, meeting reports, CME, case reports, disease descriptions, atlas, Q&A site)