MEDICAL BIOCHEMISTRY
advertisement

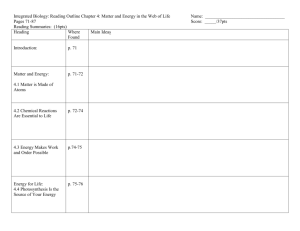
Enzymes The key element in clinical diagnosis Enzymes are biological catalysts responsible for supporting almost all of the chemical reactions that maintain animal homeostasis. Because of their role in maintaining life processes, the assay and pharmacological regulation of enzymes have become key elements in clinical diagnosis and therapeutics. The macromolecular components of almost all enzymes are composed of protein, except for a class of RNA modifying catalysts known as ribozymes. Ribozymes are molecules of ribonucleic acid that catalyze reactions on the phosphodiester bond of other RNAs. Enzymes are found in all tissues and fluids of the body. Almost every significant life process is dependent on enzyme activity. Intracellular enzymes catalyze the reactions of metabolic pathways. Plasma membrane enzymes regulate catalysis within cells in response to extracellular signals. Circulatory system enzymes are responsible for regulating the clotting of blood. Enzyme Classifications Traditionally, enzymes were simply assigned names by the investigator who discovered the enzyme. As knowledge expanded, systems of enzyme classification became more comprehensive and complex. Currently enzymes are grouped into six functional classes by the International Union of Biochemists (I.U.B.). The enzyme's name is comprised of the names of: The substrate(s), The product(s) and The enzyme's functional class. In the enzyme acetyl choline esterase for example, It catalyzes the breakdown of the neurotransmitter acetylcholine at several types of synapses as well as at the neuromuscular junction — the specialized synapse that triggers the contraction of skeletal muscle. One molecule of acetylcholinesterase breaks down 25,000 molecules of acetylcholine each second. This speed makes possible the rapid "resetting" of the synapse for transmission of another nerve impulse. The substrate of this enzyme is acetyl choline. The products are acetate and choline base. The enzyme functional clase is esterase because it is hydrolyze the ester bond in the acetyl choline. In everyday usage, most enzymes are still called by their common name. Number 1. Classification Oxidoreductases Biochemical Properties Act on many chemical groupings to add or remove hydrogen atoms. Transfer functional groups between donor and acceptor molecules. Kinases 2. Transferases are specialized transferases that regulate metabolism by transferring phosphate from ATP to other molecules. 3. Hydrolases Add water across a bond, hydrolyzing it. Add H2O, NH3 or CO2 across double 4. Lyases bonds, or remove these elements to produce double bonds. Carry out many kinds of isomerization: L 5. Isomerases to D isomerizations, mutase reactions (shifts of chemical groups) and others. Catalyze reactions in which two chemical 6. Ligases groups are joined (or ligated) with the use of energy from ATP. Enzymes are also classified on the basis of their composition: 1. Simple enzymes: They are composed wholly of protein. 2. Complex enzymes: They are composed of protein plus non-protein component (a relatively small organic molecule). Complex enzymes are also known as HOLOENZYMES. In this terminology the protein component is known as the APOENZYME. Non-protein component is known as the COENZYME or PROSTHETIC GROUP. When the binding between the apoenzyme and non-protein components is non-covalent, the small organic molecule is called coenzyme. When the binding between the apoenzyme and nonprotein components is covalent, the small organic molecule is called Prosthetic group. Many prosthetic groups and coenzymes are water-soluble derivatives of vitamins. It should be noted that the main clinical symptoms of dietary vitamin insufficiency generally arise from the malfunction of enzymes , which lack sufficient cofactors derived from vitamins to maintain homeostasis. The non-protein component of an enzyme may be as simple as a metal ion or as complex as a small non-protein organic molecule. Enzymes that require a metal in their composition are known as METALLOENZYMES if they bind and retain their metal atom(s) under all conditions with very high affinity. While those which have a lower affinity for metal ion, but still require the metal ion for activity, are known as METAL-ACTIVATED ENZYMES. Role of Coenzymes The functional role of coenzymes is to act as transporters of chemical groups from one reactant to another. The chemical groups carried can be as simple as the hydride ion (H+ + 2e-) carried by NAD or the mole of hydrogen carried by FAD; or they can be even more complex than the amine (-NH2) carried by pyridoxal phosphate. Since coenzymes are chemically changed as a consequence of enzyme action, it is often useful to consider coenzymes to be a special class of substrates, or second substrates, which are common to many different holoenzymes. In all cases, the coenzymes donate the carried chemical grouping to an acceptor molecule and are thus regenerated to their original form. This regeneration of coenzyme and holoenzyme fulfills the definition of an enzyme as a chemical catalyst, since (unlike the usual substrates, which are used up during the course of a reaction) coenzymes are generally regenerated. Enzyme Relative to Substrate Type Although enzymes are highly specific for the kind of reaction they catalyze, the same is not always true of substrates they attack. For example, Succinic dehydrogenase (SDH) always catalyzes an oxidation reduction reaction and its substrate is succinic acid. Alcohol dehydrogenase (ADH) also catalyzes oxidation-reduction reactions but attacks a number of different alcohols, ranging from methanol to butanol. Generally, enzymes having broad substrate specificity are most active against one particular substrate. In the case of alcohol dehydrogenase, ethanol is the preferred substrate. Enzymes also are generally specific for a particular steric configuration (optical isomer) of a substrate. Enzymes that attack D-sugars will not attack the corresponding Lisomer. Enzymes that act on L-amino acids will not employ the corresponding D-optical isomer as a substrate. The enzymes known as racemases provide a striking exception to these generalities; in fact, the role of racemases is to convert Disomers to L-isomers and vice versa. Thus racemases attack both D and L forms of their substrate. As enzymes have a more or less broad range of substrate specificity, it follows that a given substrate may be acted on by a number of different enzymes, each of which uses the same substrate(s) and produces the same product(s). The individual members of a set of enzymes sharing such characteristics are known as ISOZYMES. The best studied set of isozymes is the lactate dehydrogenase (LDH) system. LDH is a tetrameric enzyme composed of all possible arrangements of two different protein subunits. These subunits combine in various combinations leading to 5 distinct isozymes. ENZYME-SUBSTRATE INTERACTIONS The favored model of enzyme substrate interaction is known as the induced fit model. This model proposes that the initial interaction between enzyme and substrate is relatively weak, but that these weak interactions rapidly induce conformational changes in the enzyme that strengthen binding and bring CATALYTIC SITES close to substrate bonds to be altered. Enzymes as Biological Catalysts In cells and organisms most reactions are catalyzed by enzymes, which are regenerated during the course of a reaction. These biological catalysts are physiologically important because they speed up the rates of reactions that would otherwise be too slow to support life. Enzymes increase reaction rates sometimes by as much as one million fold, but more typically by about one thousand fold. Catalysts speed up the forward and reverse reactions proportionately so that, although the magnitude of the rate constants of the forward and reverse reactions is are increased, the ratio of the rate constants remains the same in the presence or absence of enzyme. A + B C+ D At equilibrium, there is no further apparent change and the rate of the forward reaction becomes equal to that of the backward one, hence, v1 = v2 and k1 [A] [B] = k2 [C] [D] [C] [D] ---------- = k1 / k2 = k [A] [B] Since the equilibrium constant is equal to a ratio of rate constants, it is apparent that enzymes and other catalysts have no effect on the equilibrium constant of the reactions they catalyze. Enzymes increase reaction rates by decreasing the amount of energy required to form a complex of reactants that is competent to produce reaction products. This complex is known as the activated state or transition state complex for the reaction. Michaelis-Menton Kinetics In typical enzyme-catalyzed reactions, reactant and product concentrations are usually hundreds or thousands of times greater than the enzyme concentration. Consequently, each enzyme molecule catalyzes the conversion to product of many reactant molecules. In biochemical reactions, reactants are commonly known as substrates. The catalytic event that converts substrate to product involves the formation of a transition state, and it occurs most easily at a specific binding site on the enzyme. This site, called the catalytic site of the enzyme, has been evolutionarily structured to provide specific, high-affinity binding of substrate(s) and to provide an environment that favors the catalytic events. The complex that forms when substrate(s) and enzyme combined, is called the enzyme substrate (ES) complex. Reaction products arise when the ES complex breaks down releasing free enzyme. Between the binding of substrate to enzyme, and the reappearance of free enzyme and product, a series of complex events must take place. At a minimum an ES complex must be formed; this complex must pass to the transition state (ES*); and the transition state complex must advance to an enzyme product complex (EP). The latter is finally competent to dissociate to product and free enzyme. The series of events can be shown thus: E+S <--> EScomplex<--> ES*complex<--> EPcomplex<--> E + P The kinetics of simple reactions like that above were first characterized by biochemists Michaelis and Menten. The concepts underlying their analysis of enzyme kinetics continue to provide the cornerstone for understanding metabolism today, and for the development and clinical use of drugs aimed at selectively altering rate constants and interfering with the progress of disease states. The Michaelis-Menten equation is a quantitative description of the relationship among the rate of an enzyme- catalyzed reaction [v1], the concentration of substrate [S] and two constants, Vmax and Km (which are set by the particular equation). The symbols used in the Michaelis-Menton equation refer to the reaction rate [v1], maximum reaction rate (Vmax), substrate concentration [S] and the Michaelis-Menton constant (Km). The Michaelis-Menten equation can be used to demonstrate that at the substrate concentration that produces exactly half of the maximum reaction rate, i.e., 1/2 Vmax , the substrate concentration is numerically equal to Km. This fact provides a simple yet powerful bioanalytical tool that has been used to characterize both normal and altered enzymes, such as those that produce the symptoms of genetic diseases. Rearranging the Michaelis-Menton equation leads to: From this equation it should be apparent that when the substrate concentration is half that required to support the maximum rate of reaction, the observed rate, v1, will, be equal to Vmax divided by 2; in other words, v1 = [Vmax/2]. At this substrate concentration Vmax/v1 will be exactly equal to 2, with the result that: Km =[S])2-1) = [S] The latter is an algebraic statement of the fact that, for enzymes of the Michaelis-Menten type, when the observed reaction rate is half of the maximum possible reaction rate, the substrate concentration (S) is numerically equal to the Michaelis-Menten constant (Km) . In this derivation, the units of Km are those used to specify the concentration of S, usually Molarity. Plotting of substrate concentration versus reaction velocity in Michaelis-Menten equation: Plot of substrate concentration versus reaction velocity The key features of the plot are marked by points A, B and C. At high substrate concentrations the rate represented by point C the rate of the reaction is almost equal to Vmax, and the difference in rate at nearby concentrations of substrate is almost negligible. If the Michaelis-Menten plot is extrapolated to infinitely high substrate concentrations, the extrapolated rate is equal to Vmax. When the reaction rate becomes independent of substrate concentration, or nearly so, the rate is said to be zero order. The very small differences in reaction velocity at substrate concentrations around point C (near Vmax) reflect the fact that at these concentrations almost all of the enzyme molecules are bound to substrate and the rate is virtually independent of substrate, hence zero order. At lower substrate concentrations, such as at points A and B, the lower reaction velocities indicate that at any moment only a portion of the enzyme molecules are bound to the substrate. In fact, at the substrate concentration denoted by point B, exactly half the enzyme molecules are in an EScomplex at any instant and the rate is exactly one half of Vmax. At substrate concentrations near point A the rate appears to be directly proportional to substrate concentration, and the reaction rate is said to be first order. Inhibition of Enzyme Catalyzed Reactions To avoid dealing with curvilinear plots of enzyme catalyzed reactions, biochemists Lineweaver and Burk introduced an analysis of enzyme kinetics based on the following rearrangement of the Michaelis-Menten equation: Take the inverse: 1/v1 = Km /Vmax[S] + 1/Vmax Plots of 1/v1 versus 1/[S] yield straight lines having a slope of Km/Vmax and an intercept on the ordinate at 1/Vmax. A Lineweaver-Burk Plot Lineweaver-Burk transformation of the Michaelis-Menton equation is useful in the analysis of enzyme inhibition. Since most clinical drug therapy is based on inhibiting the activity of enzymes, analysis of enzyme reactions using the tools described above has been fundamental to the modern design of pharmaceuticals. Well- known examples of such therapy include: The use of methotrexate in cancer chemotherapy to semiselectively inhibits DNA synthesis of malignant cells. The use of aspirin to inhibits the synthesis of prostaglandins which are at least partly responsible for the aches and pains of arthritis. The use of sulfa drugs to inhibit the folic acid synthesis that is essential for the metabolism and growth of diseasecausing bacteria. Enzyme inhibitors fall into two broad classes: 1. Inhibitors causing irreversible inactivation of enzymes. 2. Inhibitors whose inhibitory effects can be reversed. Irreversible Inhibitors: They cause an inactivating, covalent modification of enzyme structure. Cyanide is a classic example of an irreversible enzyme inhibitor by covalently binding mitochondrial cytochrome oxidase, it inhibits all the reactions associated with electron transport. The kinetic effect of irreversible inhibitors is to decrease the concentration of active enzyme, thus decreasing the maximum possible concentration of EScomplex . Since the limiting enzyme reaction rate is often k2[ES], it is clear that under these circumstances the reduction of enzyme concentration will lead to decreased reaction rates. Note that when enzymes in cells are only partially inhibited by irreversible inhibitors, the remaining unmodified enzyme molecules are not distinguishable from those in untreated cells; in particular, they have the same turnover number and the same Km. Turnover number, related to Vmax, is defined as the maximum number of moles of substrate that can be converted to product per mole of catalytic site per second. Irreversible inhibitors are usually considered to be poisons and are generally unsuitable for therapeutic purposes. Reversible inhibitors: They can be divided into three categories: 1. Competitive inhibitors. 2. Noncompetitive inhibitors. 3. Uncompetitive inhibitors. Inhibitor Type Binding Site on Enzyme Kinetic effect Competitive Inhibitor Specifically at the catalytic site. It competes with substrate for binding. Inhibition is reversible by substrate. Vmax is unchanged. Km is increased. Noncompetitive Inhibitor Binds E or ES complex other than at the catalytic site. Substrate binding unaltered, but ESI complex cannot form products. Inhibition cannot be reversed by substrate. Km appears unaltered. Vmax is decreased proportionately to inhibitor conc. Uncompetitive Inhibitor Binds only to ES complexes at locations other than the catalytic site. Substrate binding modifies enzyme structure, making inhibitor- binding site available. Inhibition cannot be reversed by substrate. Apparent Vmax decreased. Km is decreased. When the reversible inhibitor concentration drops, enzyme activity is regenerated. Usually these inhibitors bind to enzymes by noncovalent forces and the inhibitor maintains a reversible equilibrium with the enzyme. The equilibrium constant for the dissociation of enzyme inhibitor complexes is known as KI: KI = [E] [I] / [EI complex] The importance of KI is that in all enzyme reactions where substrate, inhibitor and enzyme interact, the normal Km and or Vmax for substrate enzyme interaction appear to be altered. These changes are a consequence of the influence of KI on the overall rate equation for the reaction. The effects of KI are best observed in Lineweaver-Burk plots. Probably the best known reversible inhibitors are competitive inhibitors, which always bind at the catalytic or active site of the enzyme. Most drugs that alter enzyme activity are of this type. Competitive inhibitors are especially attractive as clinical modulators of enzyme activity because they offer two routes for the reversal of enzyme inhibition, while other reversible inhibitors offer only one. First, as with all kinds of reversible inhibitors, a decreasing concentration of the inhibitor reverses the equilibrium regenerating active free enzyme. Second, since substrate and competitive inhibitors both bind at the same site they compete with one another for binding Raising the concentration of substrate (S), while holding the concentration of inhibitor constant, provides the second route for reversal of competitive inhibition. The greater the proportion of substrate, the greater the proportion of enzyme present in competent ES complexes. As noted earlier, high concentrations of substrate can displace virtually all competitive inhibitor bound to active sites. Thus, it is apparent that Vmax should be unchanged by competitive inhibitors. Lineweaver-Burk Plots of Inhibited Enzymes Enzymes in the Diagnosis of Pathology The measurement of the serum levels of numerous enzymes has been shown to be of diagnostic significance. This is because the presence of these enzymes in the serum indicates that tissue or cellular damage has occurred resulting in the release of intracellular components into the blood. Hence, when a physician indicates that he/she is going to assay for liver enzymes, the purpose is to ascertain the potential for liver cell damage. Commonly assayed enzymes are the amino transferases: Alanine transaminase, ALT (sometimes still referred to as serum glutamate-pyruvate aminotransferase, SGPT). Aspartate aminotransferase, AST (also referred to as serum glutamate-oxaloacetate aminotransferase, SGOT). Lactate dehydrogenase, LDH. Creatine kinase, CK (also called creatine phosphokinase, CPK). Gamma-glutamyl transpeptidase, GGT. The typical liver enzymes measured are AST and ALT. ALT is particularly diagnostic of liver involvement as this enzyme is found predominantly in hepatocytes. When assaying for both ALT and AST the ratio of the level of these two enzymes can also be diagnostic. Normally in liver disease or damage that is not of viral origin the ratio of ALT/AST is less than 1. However, with viral hepatitis the ALT/AST ratio will be greater than 1. Measurement of AST is useful not only for liver involvement but also for heart disease or damage. The level of AST elevation in the serum is directly proportional to the number of cells involved as well as on the time following injury that the AST assay was performed. The measurement of LDH is especially diagnostic for myocardial infarction because this enzyme exist in 5 closely related, but slightly different forms (isozymes). METABOLISM METABOLISM is the set of chemical reactions that occur in living organisms in order to maintain life. These processes allow organisms to grow and reproduce, maintain their structures, and respond to their environments. Metabolism is usually divided into two categories. CATABOLISM breaks down large molecules, for example to harvest energy in cellular respiration. ANABOLISM , on the other hand, uses energy to construct components of cells such as proteins and nucleic acids. The chemical reactions of metabolism are organized into metabolic pathways, in which one chemical is transformed into another by a sequence of enzymes. Most of the structures that make up animals, plants and microbes are made from three basic classes of molecule: 1. amino acids 2. carbohydrates 3. lipids As these molecules are vital for life, metabolism focuses on making these molecules, in the construction of cells and tissues, or breaking them down and using them as a source of energy, in the digestion and use of food. Many important biochemicals can be joined together to make polymers such as DNA and proteins. These macromolecules are essential parts of all living organisms. CATABOLISM Catabolism is the set of metabolic processes that break down large molecules. These include breaking down and oxidizing food molecules. The purpose of the catabolic reactions is to provide the energy and components needed by anabolic reactions. The exact nature of these catabolic reactions differ from organism to organism. The most common set of catabolic reactions in animals can be separated into three main stages: 1. Large organic molecules (proteins, carbohydrates or lipids) are digested into their smaller components outside cells. 2. These smaller molecules are taken up by cells and converted to smaller molecules, usually acetyl coenzyme A, which releases some energy. 3. The acetyl group of CoA is oxidized to H2O and CO2 in the citric acid cycle and electron transport chain, releasing the energy that is stored by reducing the coenzyme NAD+ (nicotinamide adenine dinucleotide) into NADH. Digestion Macromolecules such as starch, cellulose or proteins cannot be rapidly taken up by cells and need to be broken into their smaller units before they can be used in cell metabolism. Several common classes of enzymes digest these polymers. These digestive enzymes include proteases that digest proteins into amino acids, as well as glycoside hydrolazes that digest polysaccharides into monosaccharides. Lipases digest lipids into fatty acids and glycerol. Animals secrete these enzymes from specialized cells in their guts. The amino acids or sugars released by these extracellular enzymes are then pumped into cells by specific active transport proteins. Energy from organic compounds Carbohydrate catabolism is the breakdown of carbohydrates into smaller units. Carbohydrates are usually taken into cells once they have been digested into monosaccharides. Once inside, the major route of breakdown is glycolysis, where sugars such as glucose and fructose are converted into pyruvate and some ATP is generated. Pyruvate is an intermediate in several metabolic pathways, but the majority is converted to acetyl-CoA and fed into the citric acid cycle. Although some more ATP is generated in the citric acid cycle, the most important product is NADH, which is made from NAD+ as the acetyl-CoA is oxidized. An alternative route for glucose breakdown is the pentose phosphate pathway, which reduces the coenzyme NADPH and produces pentose sugars such as ribose, the sugar component of nucleic acids. Fats are catabolized by hydrolysis to free fatty acids and glycerol. The glycerol enters glycolysis and the fatty acids are broken down by beta oxidation to release acetyl-CoA, which then is fed into the citric acid cycle. Fatty acids release more energy upon oxidation than carbohydrates because carbohydrates contain more oxygen in their structures. Amino acids are either used to synthesize proteins and other biomolecules, or oxidized to urea and carbon dioxide as a source of energy. The oxidation pathway starts with the removal of the amino group by a transaminase. The amino group is fed into the urea cycle, leaving a deaminated carbon skeleton in the form of a keto acid. Several of these keto acids are intermediates in the citric acid cycle, for example the deamination of glutamate forms α-ketoglutarate. The glucogenic amino acids can also be converted into glucose, through gluconeogenesis. ANABOLISM Anabolism is the set of constructive metabolic processes where the energy released by catabolism is used to synthesize complex molecules. In general, the complex molecules that make up cellular structures are constructed step-by-step from small and simple precursors. Anabolism involves three basic stages: 1. The production of precursors such as amino acids, monosaccharides, isoprenoids and nucleotides. 2. Their activation into reactive forms using energy from ATP. 3. The assembly of these precursors into complex molecules such as proteins, polysaccharides, lipids and nucleic acids. Carbohydrates Metabolism In carbohydrate anabolism, simple organic acids can be converted into monosaccharides such as glucose and then used to assemble polysaccharides such as starch. The generation of glucose from compounds like pyruvate, lactate, glycerol, glycerate 3-phosphate and amino acids is called gluconeogenesis. Gluconeogenesis converts pyruvate to glucose-6-phosphate through a series of intermediates, many of which are shared with glycolysis. However, this pathway is not simply glycolysis run in reverse, as several steps are catalyzed by non-glycolytic enzymes. Polysaccharides and glycans are made by the sequential addition of monosaccharides by glycosyltransferase from a reactive sugarphosphate donor such as uridine diphosphate glucose (UDPglucose) to an acceptor hydroxyl group on the growing polysaccharide. Glycolysis Digestion of Dietary Carbohydrates Dietary carbohydrate from which humans gain energy enter the body in complex forms, such as disaccharides and the polymers starch (amylose and amylopectin) and glycogen. The polymer cellulose is also consumed but not digested. The first step in the metabolism of digestible carbohydrate is the conversion of the higher polymers to simpler, soluble forms that can be transported across the intestinal wall and delivered to the tissues. Oxidation of glucose is known as glycolysis. Glucose is oxidized to either lactate or pyruvate. Under aerobic conditions, the dominant product in most tissues is pyruvate and the pathway is known as aerobic glycolysis. When oxygen is depleted, as for instance during prolonged vigorous exercise, the dominant glycolytic product in many tissues is lactate and the process is known as anaerobic glycolysis. The Energy Derived from Glucose Oxidation Glucose + 2 ADP + 2 NAD+ + 2 Pi 2 Pyruvate + 2 ATP + 2 NADH + 2 H+ The NADH mitochondrial generated ATP during synthesis glycolysis via is oxidative used to fuel phosphorylation, producing either two or three equivalents of ATP. The net yield from the oxidation of 1 mole of glucose to 2 moles of pyruvate is, therefore, either 6 or 8 moles of ATP. Complete oxidation of the 2 moles of pyruvate, through the Citric Acid Cycle (TCA cycle) yields an additional 30 moles of ATP; the total yield, therefore being either 36 or 38 moles of ATP from the complete oxidation of 1 mole of glucose to CO2 and H2O. The citric acid cycle is part of a metabolic pathway involved in the chemical conversion of carbohydrates, fats and proteins into carbon dioxide and water to generate a form of usable energy. The Individual Reactions of Glycolysis The pathway of glycolysis can be seen as consisting of 2 separate phases. The first is the chemical priming phase requiring energy in the form of ATP. The second is considered the energy-yielding phase. In the first phase, 2 equivalents of ATP are used to convert glucose to fructose 1,6bisphosphate (F1,6BP). In the second phase, fructose 1,6-bisphosphate (F1,6BP) is degraded to pyruvate, with the production of 4 equivalents of ATP and 2 equivalents of NADH. Pathway of Glycolysis from glucose to pyruvate (Lactate). Embden-Mayerhof- دورة امدن مايرهوف Enzymes involved in Glycolysis: 1. Hexokinase & Glucokinase: The ATP-dependent phosphorylation of glucose to form glucose 6phosphate (G6P) is the first reaction of glycolysis, and is catalyzed by tissue-specific isoenzymes known as hexokinases. The phosphorylation accomplishes two goals: First, the hexokinase reaction converts nonionic glucose into an anion that is trapped in the cell, since cells lack transport systems for phosphorylated sugars. Second, the otherwise biologically inert glucose becomes activated into a labile form capable of being further metabolized. Four mammalian isozymes of hexokinase are known (Types I IV), with the Type IV isozyme often referred to as glucokinase. Glucokinase is the form of the enzyme found in hepatocytes. Non-hepatic tissues, which contain hexokinase rapidly and efficiently trap blood glucose within their cells by converting it to glucose-6-phosphate. One major function of the liver is to deliver glucose to the blood and this is ensured by having a glucose phosphorylating enzyme glucokinase. This feature of hepatic glucokinase allows the liver to buffer blood glucose. After meals, when postprandial blood glucose levels are high, liver glucokinase is significantly active, which causes the liver preferentially to trap and to store circulating glucose. When blood glucose falls to very low levels, tissues such as liver and kidney, which contain glucokinases but are not highly dependent on glucose, do not continue to use the meager glucose supplies that remain available. At the same time, tissues such as the brain, which are critically dependent on glucose, continue to scavenge blood glucose. Under various conditions of glucose deficiency, such as long periods between meals, the liver is stimulated to supply the blood with glucose through the pathway of gluconeogenesis. The levels of glucose produced during gluconeogenesis are insufficient to activate glucokinase, allowing the glucose to pass out of hepatocytes and into the blood. 2. Aldolase: Aldolase catalyses the hydrolysis of F1,6BP into two 3-carbon products: dihydroxyacetone glyceraldehyde 3-phosphate phosphate (G3P). The (DHAP) aldolase and reaction proceeds readily in the reverse direction, being utilized for both glycolysis and gluconeogenesis. 3. Triose Phosphate Isomerase: The two products of the aldolase reaction equilibrate readily in a reaction catalyzed by triose phosphate isomerase. Succeeding reactions of glycolysis utilize G3P as a substrate; thus, the aldolase reaction is pulled in the glycolytic direction by mass action principals. 4. Glyceraldehyde-3-Phosphate Dehydrogenase: The second phase of glucose catabolism features the energyyielding glycolytic reactions that produce ATP and NADH. In the first of these reactions, glyceraldehyde-3-P dehydrogenase (G3PDH) catalyzes the NAD+-dependent oxidation of G3P to 1,3bisphosphoglycerate (1,3BPG) and NADH. The G3PDH reaction is reversible, and the same enzyme catalyzes the reverse reaction during gluconeogenesis. 5. Phosphoglycerate Kinase: The high-energy phosphate of 1,3-BPG is used to form ATP and 3phosphoglycerate (3PG) by the enzyme phosphoglycerate kinase. Note that this is the only reaction of glycolysis or gluconeogenesis that involves ATP and yet is reversible under normal cell conditions. Associated with the phosphoglycerate kinase pathway is an important reaction of erythrocytes, the formation of 2,3bisphosphoglycerate, 2,3BPG (see Figure below) by the enzyme bisphosphoglycerate mutase. 2,3BPG is an important regulator of hemoglobin's affinity for oxygen. Note that 2,3- bisphosphoglycerate phosphatase degrades 2,3BPG to 3- phosphoglycerate, a normal intermediate of glycolysis. The 2,3BPG shunt thus operates with the expenditure of 1 equivalent of ATP per triose passed through the shunt. The process is not reversible under physiological conditions. 6. Phosphoglycerate Mutase and Enolase: The remaining reactions of glycolysis are aimed at converting the relatively low energy phosphoacyl-ester of 3PG to a high-energy form and harvesting the phosphate as ATP. The 3PG is first converted to 2PG by phosphoglycerate mutase and the 2PG conversion to phosphoenoylpyruvate (PEP) is catalyzed by enolase 7. Pyruvate Kinase: The final reaction of aerobic glycolysis is catalyzed by the highly regulated enzyme pyruvate kinase (PK). In this strongly exergonic reaction, the high-energy phosphate of PEP is conserved as ATP. The loss of phosphate by PEP leads to the production of pyruvate in an unstable enol form, which spontaneously tautomerizes to the more stable, keto form of pyruvate. This reaction contributes a large proportion of the free energy of hydrolysis of PEP. Anaerobic Glycolysis Under aerobic conditions, pyruvate in most cells is further metabolized via the TCA cycle. Under anaerobic conditions and in erythrocytes under aerobic conditions, pyruvate is converted to lactate by the enzyme lactate dehydrogenase (LDH), and the lactate is transported out of the cell into the circulation. The conversion of pyruvate to lactate, under anaerobic conditions, provides the cell with a mechanism for the oxidation of NADH (produced during the G3PDH reaction) to NAD+; which occurs during the LDH catalyzed reaction. Aerobic glycolysis generates substantially more ATP per mole of glucose oxidized than does anaerobic glycolysis. The utility of anaerobic glycolysis, to a muscle cell when it needs large amounts of energy, stems from the fact that the rate of ATP production from glycolysis is approximately 100X faster than from oxidative phosphorylation. Pyruvate Metabolism Pyruvate is the branch point molecule of glycolysis. The ultimate fate of pyruvate depends on the oxidation state of the cell. In the reaction catalyzed by G3PDH a molecule of NAD+ is reduced to NADH. In order to maintain the re-dox state of the cell, this NADH must be re-oxidized to NAD+. During aerobic glycolysis this occurs in the mitochondrial electron transport chain generating ATP. Thus, during aerobic glycolysis ATP is generated from oxidation of glucose directly at the PGK and PK reactions as well as indirectly by re-oxidation of NADH in the oxidative phosphorylation pathway. Additional NADH molecules are generated during the complete aerobic oxidation of pyruvate in the TCA cycle. Pyruvate enters the TCA cycle in the form of acetyl-CoA which is the product of the pyruvate dehydrogenase reaction. The fate of pyruvate during anaerobic glycolysis is reduction to lactate. LACTATE METABOLISM During anaerobic glycolysis, the large quantity of NADH produced is oxidized by reducing pyruvate to lactate. This reaction is carried out by lactate dehydrogenase, (LDH). The lactate produced during anaerobic glycolysis diffuses from the tissues and is transproted to highly aerobic tissues such as cardiac muscle and liver. The lactate is then oxidized to pyruvate in these cells by LDH and the pyruvate is further oxidized in the TCA cycle. If the energy level in these cells is high the carbons of pyruvate will be diverted back to glucose via the gluconeogenesis pathway. FRUCTOSE METABOLISM Diets containing large amounts of sucrose can utilize the fructose as a major source of energy. The pathway to utilization of fructose differs in muscle and liver. In the muscle, which contains only hexokinase can phosphorylate fructose to F6P which is a direct glycolytic intermediate. In the liver, which contains mostly glucokinase (specific for glucose as its substrate) requires the function of additional enzymes (aldolases) to utilize fructose in glycolysis. Clinical Significances of Fructose Metabolism FRUCTOSURIA is metabolic disorder caused by the lack of fructokinase. HEREDITARY FRUCTOSE INTOLERANCE is a potentially lethal disorder resulting from a lack of aldolase B. The disorder is characterized by severe hypoglycemia and vomiting following fructose intake. Prolonged intake of fructose by infants with this defect leads to vomiting, poor feeding, jaundice يرقاان وو عارور باالعاازازا, hepatomegaly, hemorrhage and eventually hepatic failure and death. Patients remain symptom free on a diet devoid of fructose and sucrose. GALACTOSE METABOLISM Galactose, which is metabolized from the milk sugar, lactose enters glycolysis by its conversion to glucose-1-phosphate (G1P). This occurs through a series of steps summarized in the following figure: Clinical Significances of Galactose Metabolism GALACTOSEMIA is a major symptom of the loss of the two enzymes, galactokinase and galactose-1-phosphate uridyl transferase. Vomiting and diarrhea occur following ingestion of milk, hence individuals are termed lactose intolerant. Clinical findings elevated blood galactose, hyper galactosemia, urinary galactitol excretion and hyper amino acid uria. Unless controlled by exclusion of galactose from the diet, these galactosemias can go on to produce blindness and fatal liver damage. GLYCOGEN METABOLISM The body obtains glucose from either one of the following: 1. Directly from the diet 2. From amino acids and lactate via gluconeogenesis. Glucose obtained from these two primary sources either remains soluble in the body fluids or is stored in a polymeric form, glycogen. Glycogen is considered the principal storage form of glucose and is found mainly in liver and muscle. With up to 10% of its weight as glycogen, the liver has the highest specific content of any body tissue. Muscle has a much lower amount of glycogen per unit mass of tissue, but since the total mass of muscle is so much greater than that of liver, total glycogen stored in muscle is about twice that of liver. Stores of glycogen in the liver are considered the main buffer of blood glucose levels. GLYCOGENOLYSIS Degradation of stored glycogen, termed glycogenolysis, occurs through the action of glycogen phosphorylase. The glucose-1-phosphate produced by the action of phosphorylase is converted to glucose-6-phosphate by phosphor gluco mutase. The enzyme phosphate is transferred to C-6 of glucose-1phosphate generating glucose-1,6-phosphate as an intermediate. The conversion of glucose-6-phosphate to glucose, which occurs in the liver, kidney and intestine, by the action of glucose-6phosphatase does not occur in skeletal muscle as these cells lack this enzyme. Therefore, any glucose released from glycogen stores of muscle will be oxidized in the glycolytic pathway. In the liver the action of glucose-6-phosphatase allows glycogenolysis to generate free glucose for maintaining blood glucose levels. Gluconeogenesis Gluconeogenesis is the biosynthesis of new glucose, (i.e. not glucose from glycogen). The production of glucose from other metabolites is necessary for use as a fuel source by the brain, testes, erythrocytes and kidney medulla since glucose is the sole energy source for these organs. During starvation, however, the brain can derive energy from ketone bodies which are converted to acetyl-CoA. Substrates for Gluconeogenesis Lactate: Lactate is a predominate source of carbon atoms for glucose synthesis by gluconeogenesis. During anaerobic glycolysis in skeletal muscle, pyruvate is reduced to lactate by lactate dehydrogenase (LDH). LDH Pyruvate Lactate This reaction serves two critical functions during anaerobic glycolysis: 1. LDH reaction requires NADH and yields NAD+ which is then available for use by the glyceraldehyde-3-phosphate dehydrogenase reaction of glycolysis. 2. The lactate produced by the LDH reaction is released to the blood stream and transported to the liver where it is converted to glucose. The glucose is then returned to the blood for use by muscle as an energy source and to replenish glycogen stores. This cycle is termed the Cori cycle. Pyruvate: Pyruvate, generated in muscle and other peripheral tissues, can be transaminated to alanine which is returned to the liver for gluconeogenesis. The transamination reaction requires an α-amino acid as donor of the amino group, generating an α-keto acid in the process. This pathway is termed the glucose-alanine cycle. The glucose-alanine cycle is, therefore, an indirect mechanism for muscle to eliminate nitrogen while replenishing يازودits energy supply. However, the major function of the glucose-alanine cycle is to allow non-hepatic tissues to deliver the amino portion of catabolized amino acids to the liver for excretion as urea. Within the liver the alanine is converted back to pyruvate and used as a gluconeogenic substrate (if that is the hepatic requirement) or oxidized in the TCA cycle. The amino nitrogen is converted to urea in the urea cycle and excreted by the kidneys. Citric Acid Cycle The citric acid cycle — also known as the tricarboxylic acid cycle (TCA cycle), the Krebs cycle, is a series of enzyme-catalysed chemical reactions of central importance in all living cells that use oxygen as part of cellular respiration. In eukaryotes, the citric acid cycle occurs in the matrix of the mitochondrion. In aerobic organisms, the citric acid cycle is part of a metabolic pathway involved in the chemical conversion of carbohydrates, fats and proteins into carbon dioxide and water to generate a form of usable energy. Other relevant reactions in the pathway include those in glycolysis and pyruvate oxidation before the citric acid cycle, and oxidative phosphorylation after it. In addition, it provides precursors for many compounds including some amino acids and is therefore functional even in cells performing fermentation. The TCA cycle showing enzymes, substrates and products. The GTP generated during the succinate thiokinase (succinyl-CoA synthetase) reaction is equivalent to a mole of ATP by virtue of the presence of nucleoside diphosphokinase. The 3 moles of NADH and 1 mole of FADH2 generated during each round of the cycle feed into the oxidative phosphorylation pathway. Each mole of NADH leads to 3 moles of ATP and each mole of FADH2 leads to 2 moles of ATP. Therefore, for each mole of pyruvate which enters the TCA cycle, 12 moles of ATP can be generated. IDH = isocitrate dehydrogenase. α-KGDH = α-ketoglutarate dehydrogenase. MDH = malate dehydrogenase. Place mouse over cycle intermediate names to see their structures. CITRIC ACID CYCLE (TCA CYCLE) Krebs دورة