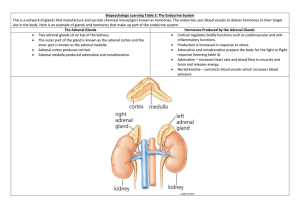
Adrenal cortex
advertisement

Zona Glomerulosa • Zona Fasiculata • Zona Reticularis • Steroid Hormones • Glucocorticoids • Mineralcorticoids • Sex Steroids – – – – – – – – – CHO, lipid & fat metabolism Increases blood glucose levels & gluconeogenesis Increases protein breakdown Inhibits protein synthesis Elecrolyte & fluid balance Increases sodium & water retention Regulated by renin & andiotensin Low synthesis in adrenals compared to gonads Virilising hormones may be secreted 4 Conditions Affecting Adrenal Cortex Adrenocortical Hyperfunction • Cushing’s syndrome • Hyperaldosterone • – Increased glucocorticoid levels – Excessive water retention Ht – Excess androgens (testosterone) in peripheral tissue Adrenogenital syndromes • • Dehydroepiandrosterone Androstentendione Adrenocortical Insufficiency • • Acute Adrenocortical Insufficiency Chronic Adrenocortical Insuffeciency (Addison’s) 5 Acute Adrenocortical Insufficiency Aetiology & pathogenesis • Sepsis Waterhouse-Friderichsen syndrome • Sudden withdrawal of long term corticosteroid treatment – – – – • Neisseria meningitidis (classic) Pseudonomas; pneumococci; H. influenzae (others) Unclear pathogenesis endotoxin induced vascular injury (massive haemorrhage) with associated DIC Inability of atrophic adrenals to produce glucocorticoids Stress with underlying chronic adrenal insufficiency – Acute adrenal crises on limited physiological reserves 6 Massive adrenal haemorrhage, resulting in primary acute adrenal insufficiency Metastatic breast carcinoma affecting the adrenal gland and causing primary chronic adrenal insufficiency Chronic Adrenocortical Insufficiency “Addison’s Disease” Aetiology & pathogenesis • • Primary Addison’s disease Secondary causes – – Tuberculosis caseous necrosis of adrenal cortex Autoimmune adrenalitis – – – – – – AIDS Metastatic disease Systemic amyloidosis Fungal infections Haemochromatosis Sarcoidosis • Ass with e.g. pernicious anaemia; thyroiditis; IDDM 8 9 Morphology • Primary autoimmune adrenitis – Irregularly shrunken glands • TB; fungi; sarcoidosis – Granulomas in adrenals • Metastatic Ca – Adrenals enlarged – achitecture obscured • Secondary hypoadrenalism – Adrenals small & flattened – Atrophy of corticol cells 10 Clinical Features • Insidious onset • Primary adrenal disease • • • • • • – – Progressive weakness & fragiability Non-specific complaints (anorexia; N/V; WL) – Hyperpigmentation (increased ACTH) – Infections; trauma; sugery intractable vomiting; abdominl pain; hypotension; vascular collaspe death Hyperkalaemia & hyponatraemia Hypotension (volume depletion) & dehydration Hypoglycaemia Sexual dysfunction Adrenal crises Diagnosis – Low plasma cortisol 11 Laboratory findings. 1. A low serum Na level and a high serum P level together 2. with a characteristic clinical picture suggest the possibility of Addison’s disease. Adrenal insufficiency can be specifically diagnosed by: • • 3. low levels of plasma glucocorticoids and mineralocorticoids, or urinary 17 – hydroxycorticosteroid (17 – OHCS) or 17 – ketogenic steroid (17 – KGS); demonstrating failure to increase plasma cortisol levels, or urinary 17 – OHCS or 17 – KGS excretion, upon administration of ACTH (in patients with primary adrenal insufficiency, those with secondary adrenocortical insufficiency will have a significant increase in plasma cortisol or 24 - h urinary corticosteroid levels.) To distinguish between primary and secondary adrenal insufficiency, me have to find the level of plasma ACTH: primary shows increased, and secondary shows decreased level. Features of Addison’s d. This is a caseating granuloma of tuberculosis in the adrenal gland. Tuberculosis used to be the most common cause of chronic adrenal insufficiency. Now, idiopathic (presumably autoimmune) Addison's disease is much more 14 often the cause for chronic adrenal insufficiency. The pair of adrenals in the center are normal. Those at the top come from a patient with adrenal atrophy (with either Addison's disease or long-term corticosteroid therapy). The adrenals at the bottom represent bilateral cortical hyperplasia. This could be due to a pituitary adenoma secreting ACTH (Cushing's disease), or 16 Cushing's syndrome from ectopic ACTH production, or idiopathic adrenal hyperplasia. Case Discussion A 26-year old man is admitted to the Intensive Care Unit 3 days vomiting – hourly Drowsy BP 60/30 Deeply pigmented Na+ 125 mmol/l (N 135-145) K+ 5.4 mmol/l (N 3.5-5.0) Questions Diagnosis Pathogenesis What hormone is deficient Diagnostic test Treatment Complications Addison’s disease Pathogenesis Destruction of adrenal glands Autoimmune Tuberculosis Tumour/infiltration Infective (meningococcus) Hormone deficiency Cortisol Aldosterone Diagnostic test Synacthen test Treatment Cortisol replacement Hydrocortisone/Cortisone Aldosterone replacement Fludrocortisone Complications Adrenal crisis – intercurrent illness Synacthen test Pituitary •Baseline cortisol may be normal in Addison’s disease •Synacthen test: uses synthetic ACTH analogue •Normal response: rise in cortisol Synacthen (=synACTHen) Adrenal gland Cortisol