floopy infant
advertisement

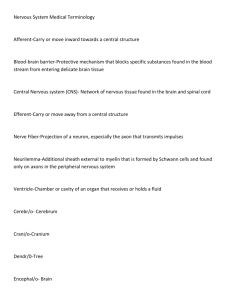
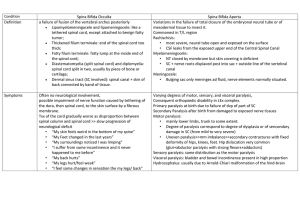
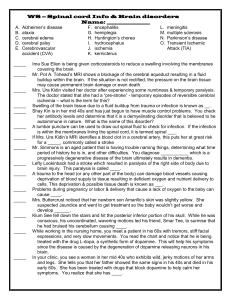
Floppy Infant Brain Spinal cord Hypotonia Clinical features: • In early infancy, there is decreased muscular activities both spontaneous and in response to postural reflex testing and to passive motion. • In young infants , hypotonia manifested as ‘Frog posture”. • In older infants, there is delay in motor milestones. • Ventral suspension: In this position floppy infant droops over the hand like an inverted U shape. • Head lag when pulled up from supine to sitting position. Clinical features • Weak cry • Abdominal breathing. • No or depressed tendon reflexes. • Fasciculation's of the tongue. • Normal mentality in infantile progressive muscular atrophy • Mental retardation in congenital muscular dystrophy. Lower Motor Neuron Etiology: A- Paralytic causes: Lesion of the lower motor neuron. 1- Infantile progressive muscular atrophy (IPSMA): Decreased movement in-utero – Gradual weakness – Delay in gross motor milestones- Weak cry – Absent deep tendon reflexes – Fasciculation's of tongueNormal personal and social behaviors. 2- Infantile botulism: Poor feeding, constipation, failure to thrive, facial weakness, ptosis- ocular palsy, inability to suck or swallow, apnea (Source: soil dust, honey). Etiology 3-Myasthenia gravis (Neonatal transient and congenital persistent): Poor sucklingchocking- respiratory distress- weak crymother may have myasthenia. 4- Myotonic dystrophy: AD, Polyhydramnios, failure of suckling, facial diplegia, arthrogryposis, thin ribs, developmental delay. Myathenia gravis Etiology: continue 5- Congenital muscular dystrophy : Early onset facial weakness, joint contractures, mental retardation, seizures. 6- Rare types of myopathy (Nemaline and Central core): Proximal weakness( shoulders, hips),but the finger movement is preserved, intelligence, fine motor, language and social milestones are normal. 7- Spinal cord lesion: Upper thoracic spinal cord injury after breech extraction. 8- Glycogenosis: Type II glycogen storage = pompe disease, type V= McArdle disease). B- Non-Paralytic causes: 1- CNS disorders: Atonic diplegia, choeoathetosis , ataxic and atonic cerebral palsy. 2- Syndromes with hypotonia: 1-Tisomy 21. 2- Prader willi syndrome (deletion of 15q11 gene) 3- Marfan syndrome. 4- Turner syndrome. 3- Degenerative disorders: -Tay-Sack’s disease. - Metachromatic leukodystrophy. Non- paralytic causes Continue 4- Systemic diseases: -Malnutrition. -Celiac disease, and Cystic.Fibrosis. - Chronic illness . - Metabolic diseases: Hypercalcemia. - Endocrinopathy: Hypothyroidism. 5- Benign congenital hypotonia: mild to moderate hypotonia with weakness. Celiac Disease Hypothyroidism Differential diagnosis of flaccid paralysis (LMNL): • 1-Guillain Barre syndrome (postinfectious polyneuritis): It is the most common cause of acute paralysis in children/Although infants can be affected, most cases are seen in children above the age of 3 years. History of preceding viral infection, one or two weeks before the onset of ascending symmetrical paralysis, is usually obtained. • 2-Poliomyelitis: It is going to be eradicated in many countries of the world. The spinal lesion lead to Asymmetrical flaccid paralysis. Differential diagnosis of flaccid paralysis (LMNL): • 3-Post diphtheritic paralysis: This form of toxic polyneuritis is uncommon nowadays because of the routine vaccination. History of preceding sore throat and swollen neck (pharyngeal diphtheria) or stridor (laryngeal diphtheria), 1 - 2 week before the onset of paralysis can be obtained. • 4-Transverse myelitis: It is the second most common cause of acute symmetric paralysis. -It is a segmental dysfunction of the spinal cord without an evidence of spinal cord compression. The cause is probably either a direct viral infection or an autoimmune disease. Transverse Myelitis Differential diagnosis of flaccid paralysis (LMNL): continue • 5- Botulism: It is a toxic neuromuscular blockade caused by clostridium botulinum (anaerobic gram positive bacteria). Three forms are present : (1) Infant botulism occurs in infants. Germination of spores in gastrointestinal tract follows exposure to soil, house dust. honey or corn syrup ; (2) Food-induced botulism occurs with ingestion of improperly home-preserved foods containing the toxins. (3) Wound botulism occurs due to wound contamination with the clostridium botulinum organisms. Differential diagnosis of flaccid paralysis (LMNL): continue • 6- Acute spinal cord compression: Trauma to the back, spinal epidural abscess and vascular anomalies of the cord may produce acute paralysis. - Occasionally, spinal cord tumors may also present with acute paralysis. - Myelography is essential to demonstrate the obstruction. CT scan of the spine or MRI are more sensitive. • 7- Hypotonia with movement disorders: - In acute cerebellar ataxia, hypotonia is usually present, but the truncal ataxia with unsteady gait is the most characteristic feature. - In rheumatic chorea, hypotonia is present and may be marked simulating acute paralysis but abnormal involuntary choreic movements is the dominating finding. GB Syndrome Spinal cord syndrome poliomyelitis Eitiology Delayed hypersesitivity. antibody mediated Trasverse myelitis,spinal cord abscess,TB Poliovirus type I,II,III History GI or URTI, 5 to 14days preceding symptoms Rapid progression Unimmunized, of symptoms URTI or GI infection Symptoms Symmetric weakness in LL gradually ascending with parasthesias. normal bowel & bladder function Back pain. Sensory loss below the level of lesion, sphincter problems Fever,. meningism, muscle tenderness, asymmetric weakness Signs Symmetric flaccid weakness, sensations intact, gradually ascending Symmetric areflexia,sensory loss below the level of lesion., pain, bowel and bladder dysfunction Assymmetric flaccid weakness, sensations intact, muscle wasting CSF findings Normal cell count with raised protiens 2nd week of illness Pleocytosis with raised protiens Pleocytosis with raised protiens EMG/NCS Signs of denervation, Normal initially NCS shows delayed conduction NCS normal, EMG denervation later Course and prognosis Recovery in majority Depends on within 12 months eitiology Permanent disability in 1% cases Diagnosis: Differentiate hypotonia with hyporeflexia from hypotonia with hyperreflexia. -Brisk reflexes point to cerebral dysfunction. -Creatine kinase level and EMG are normal in neurological lesions. -Prolonged nerve conduction in polyneuropathy. -Muscle biopsy to diagnose the type of myopathy. Management: -Treat the cause. -Physiotherapy. -Genetic counseling.