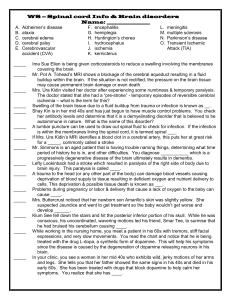
Adult and Geriatric Health Nursing-2/Theory Unit Two Nursing Care for Patients with
advertisement

Adult and Geriatric Health Nursing-2/Theory Unit Two Nursing Care for Patients with Neurological Problems Introduction: Central Nervous System: • The central nervous system consists of the brain and spinal cord. • The brain plays a central role in the control of most bodily functions, including awareness, movements, sensations, thoughts, speech, and memory. • Some reflex movements can occur via spinal cord pathways without the participation of brain structures. Introduction: Central Nervous System: • The spinal cord is connected to a section of the brain called the brainstem and runs through the spinal canal. • Cranial nerves exit the brainstem. • Nerve roots exit the spinal cord to both sides of the body. • The spinal cord carries signals (messages) back and forth between the brain and the peripheral nerves. • Cerebrospinal fluid surrounds the brain and the spinal cord and also circulates within the cavities (called ventricles) of the central nervous system. • The meninges surround the brain and the spinal cord. Introduction: Central Nervous System: • Te cerebrospinal fluid circulates between 2 meningeal layers called the pia matter and the arachnoid (or pia-arachnoid membranes). The outer, thicker layer serves the role of a protective shield and is called the dura matter. • The basic unit of the central nervous system is the neuron (nerve cell). • Billions of neurons allow the different parts of the body to communicate with each other via the brain and the spinal cord. • A fatty material called myelin coats nerve cells to insulate them and to allow nerves to communicate quickly. Introduction: • The Brain: – The Cerebrum: • The cerebrum is the largest part of the brain and controls voluntary a ctions, speech, senses, thought, and memory. Introduction: • The Brain: – The Thalamus: • Integrates and relays sensory information to the cortex of the parietal, temporal, and occipital lobes. • Other roles of the thalamus include motor and memory control. • Located in the lower central part of the brain (that is, upper part of the brainstem) and is located medially to the basal ganglia. • The brain hemispheres lie on the thalamus. Introduction: • The Brain: – The Hypothalamus: • Located below the thalamus. • Regulates automatic functions such as appetite, thirst, and body temperature. It also secretes hormones that stimulate or suppress the release of hormones (for example, growth hormones) in the pituitary gland. Introduction: • The Brain: – The Pituitary Gland: • Located at the base of the brain. • The pituitary gland produces hormones that control many functions of other endocrine glands. • It regulates the production of many hormones that have a role in growth, metabolism, sexual response, fluid and mineral balance, and the stress response. – The Ventricles: • Cerebrospinal fluid-filled cavities in the interior of the cerebral hemispheres. Introduction: • The Brain: – The Base of the Brain: • The base of the brain contains the cerebellum and the brainstem. • The cerebellum has been known to control equilibrium and coordination and contributes to the generation of muscle tone. • The brainstem connects the brain with the spinal cord. It includes the midbrain, the pons, and the medulla oblongata. • The midbrain is located below the hypothalamus. Some cranial nerves that are also responsible for eye muscle control exit the midbrain. Introduction: • The Brain: – The Base of the Brain: • The pons serves as a bridge between the midbrain and the medulla oblongata. The pons also contains the nuclei and fibers of nerves that serve eye muscle control, facial muscle strength, and other functions. • The medulla oblongata is the lowest part of the brainstem and is interconnected with the cervical spinal cord. The medulla oblongata also helps control involuntary actions, including vital processes, such as heart rate, blood pressure, and respiration, and it carries the corticospinal (that is, motor function) tract toward the spinal cord. Introduction: • The Spinal Cord: – The spinal cord is an extension of the brain and is surrounded by the vertebral bodies that form the spinal column. – The central structures of the spinal cord are made up of gray matter (nerve cell bodies), and the external or surrounding tissues are made up of white matter. – Within the spinal cord are 30 segments that belong to 4 sections (cervical, thoracic, lumbar, sacral), based on their location: Introduction: • The Spinal Cord: – Eight cervical segments: These transmit signals from or to areas of the head, neck, shoulders, arms, and hands. – Twelve thoracic segments: These transmit signals from or to part of the arms and the anterior and posterior chest and abdominal ar eas. – Five lumbar segments: These transmit signals from or to the legs and feet and some pelvic organs. – Five sacral segments: These transmit signals from or to the lower back and buttocks, pelvic organs and genital areas, and some areas in the legs and feet. Introduction: • Peripheral Nervous System: – Nerve fibers that exit the brainstem and spinal cord become part of the peripheral nervous system. – Cranial nerves exit the brainstem and function as peripheral nervous system mediators of many functions, including eye movements, facial strength and sensation, hearing, and taste Cerebral Vascular Attacks (CVA): -Stroke • Cerebro vascular accident (CVA), or stroke, is a sudden loss of brain function accompanied by neurological deficit. • Causes is ischemia (oxygen deprivation) resulting from a thrombus, embolus, severe vasospasm, or cerebral hemorrhage→ neurological deficits (temporary or permanent) of sensation, movement, thought, memory, or speech. Cerebral Vascular Attacks (CVA): -Stroke • Transient Ischemic Attack (TIA): – A TIA is a temporary or transient (Few seconds to 24 hours) episode of neurological dysfunction caused by temporary impairment of blood flow to the brain. – Transient ischemic attacks (TIAs) frequently precede a CVA. Cerebral Vascular Attacks (CVA): -Stroke • Risk factors for stroke: – – – – – – Hypertension. Diabetes mellitus. Atherosclerosis. Aneurysm. Cardiac disease. High blood cholesterol. – – – – – – Obesity. Sedentiary lifestyle.. Smoking. Stress. Drug abuse (cocaiene). Use of oral contraceptive. Cerebral Vascular Attacks (CVA): -Stroke • Diagnostic test: – Mainly is brain CT scan. • Signs and Symptoms: – Hemiplegia: paralysis of one side of the body on the side opposite of the brain lesion. – Hemiparesis: weakness of one side of the body. – Dysarthria: impairment of speech due to muscle dysfunction. – Dysphagia: impairment of swallowing muscles. – Emotional liability: loss of emotional control, depression, and decreased tolerance to stressors. – Inability to control behavior and inability to process multiple pieces of information. Cerebral Vascular Attacks (CVA): -Stroke • Signs and Symptoms: – Visual deficits of double vision and decreased visual acuity. – Decreased sensation to touch, pressure, pain, heat, and cold. – Confusion and disorientation. – Memory impairment, poor judgment, short attention span, difficulty organizing thoughts, and inability to reason or calculate. – Bowel and bladder dysfunction. – Aphasia: inability to produce speech. Cerebral Vascular Attacks (CVA): -Stroke • Management: – Medical: • Aims of medical treatment: – Airway maintenance and supportive therapy during the first 24 to 48 hours. – Maintaining adequate cerebral perfusion. – Preventing cerebral edema. – Reducing neurological deficit. – Surgical: • Surgical removal of the thrombus (thrombolectomy) or embolus (embolectomy) may be necessary to relieve pressure on the brain Cerebral Vascular Attacks (CVA): -Stroke • Management: – Pharmacological: • Stroke caused by thrombi: – Anticoagulants (aspirin, heparin, or coumadin) are used to prevent further clot formation. – Thrombolytic agents (Activase, streptokinase) to dissolve thrombi. • Stroke caused by bleeding: – Dexamethasone (Decadron) may be used to reduce intracranial pressure. – Anticonvulsants may be used if convulsions are present. Cerebral Vascular Attacks (CVA): -Stroke • Management: – Diet: • Intravenous fluids or tube feedings or soft food according to the risk of choking. – Activity: • Elevate bed to increase cerebral perfusion and Bed rest according to the physician description. – Other Therapies: • Rehabilitation, physical, and speech therapy. Cerebral Vascular Attacks (CVA): -Stroke • Nursing care: – Administer medication. – Continuous respiratory and neurological assessment. – Provide air way care (suctioning) and administer oxygen as needed. – Assess the swallowing ability of the client and provide appropriate food (mainly require nasogastric tube feeding). – Help client in diagnostic test procedures and provide care during test and in transportation if needed. – Assess V/S frequently and provide appropriate care if needed Cerebral Vascular Attacks (CVA): -Stroke • Nursing care: – Perform or help client in self- care activity. – Change position every 2 hours at least. – Assess client's and family's needs for discharge teaching, knowledge level about necessary home care. – Develop a multidisciplinary plan for client and family teaching. – Teach small segments of information at a time and reinforce teaching, then, have client and family return demonstrate or verbalize knowledge. – Areas of teaching are medication administration (dosages, actions, and side effects to report to the physician), mobility needs; self-care needs; safety factors; communication; swallowing; elimination; and skin care. Space Occupying Lesions of the Brain (Brain tumors): • Brain tumors are space-occupying intracranial lesions (benign or malignant) that increase in volume of brain tissue. • The Etiology is unknown. • Clinical manifestations: – – – – – – Alterations in consciousness. Decreased mental functioning. Headaches. Seizures. Vomiting (sometimes sudden and projectile). Other S&S are relative to the functions of areas involved. Space Occupying Lesions of the Brain (Brain tumors): • Diagnostic evaluation: – – – – CT scan. MRI. Electroencephalogram (EEG). Needle biopsies of the tumor may be performed to identify the type of tumor. • Management: – Medical: • Radiotherapy. • Chemotherapy. – Surgical: • Surgical intervention (usual or laser). • Some CSF may be removed (shunt) to relieve increased pressure Space Occupying Lesions of the Brain (Brain tumors): • Management: – Pharmacological: • Pharmacological interventions are based on presenting symptoms: – – – – – Dexamethasone (Decadron) to decrease cerebral edema. Phenytoin (Dilantin) is given to prevent seizure activity. Antacids and H2 blockers to prevent gastric irritation. Analgesics, NSAIDs, or codeine are used for headaches. Stool softeners to prevent straining. Space Occupying Lesions of the Brain (Brain tumors): • Nursing intervention: – Assess fatigue, pain, headache, weakness, and ability to perform daily activities. – Sensory alterations such as hearing, visual, or olfactory changes should be assessed. – Psychosocial assessment and support: changes in personality or judgment. – Assess of functional ability, mobility, and mental status, including motor strength, gait, and level of consciousness. – Administer medication. – Provide support to prevent complication such as side rails. – Allow client to verbalize feeling of anxiety and discuss coping patterns previously used. Space Occupying Lesions of the Brain (Brain tumors): • Nursing intervention: – Provide emotional support by listening and guiding client to explore feelings. – Teach client and family about diagnostic tests, treatments, and; expected outcomes. – Involve client in planning daily schedule that includes frequent rest periods. – Assess client's ability to perform ADL, need for assistance to conserve energy. – Cluster care activities to provide frequent rest periods that agree with peak effectiveness of analgesics. – Assess client's weight every other day. – Provide frequent small feedings of high-calorie and high-protein foods. Intracranial Pressure (ICP): • Intracranial pressure is the maintenance of normal volume of major component in the skull: brain, cerebrospinal fluid, and blood. • Intracranial pressure affected by: – – – – Arterial and venous circulation. Abdominal and thoracic cavity pressure. Increase in body temperature. Posture (i.e., flexion of neck, head lower than body). Intracranial Pressure (ICP): • Intracranial pressure measured by: – Lumber puncture (LP) by measuring the cerebrospinal fluid (CSF) pressure as it drains through a manometer. – Inserting a catheter into one of the ventricles of the brain. – Inserting a screw or bolt into the subarachnoid. Intracranial Pressure (ICP): – Normal CSF pressure :bed elevated 30 degrees is: • 80 to 180 cm of water (by LP manometer) . • 0 to 15 mm of mercury (by catheter pressure transducer). Increased Intracranial Pressure (IICP): • IICP is fundamental to the care of patients with neurological problems because uncontrolled and untreated IICP →irreversible neurological pathology and cardiopulmonary arrest. • Causes of IICP: – – – – – Cerebral tumor. Hematoma. Abscess. Malabsorption of CSF. Edema of the brain (cerebral edema): hepatic or renal encephalopathy and lead toxicity. Increased Intracranial Pressure (IICP): • Signs and symptoms: – Early signs and symptoms: • LOC: irritability, agitation, mild confusion, personality changes, and lower Glasgow Coma Scale (GCS) score. • Pupils: drooping of eyelid (ptosis), delayed reaction, unilateral change in pupil size. • Vision: blurred; diplopia; decreased visual acuity. • Motor: weakness especially on one side. • Sensory: decreased response to touch. Increased Intracranial Pressure (IICP): • Signs and symptoms: – Early signs and symptoms: • Headache: early morning headache; possible vomiting with or without nausea. • Speech: slow or slurred. • Memory: may be impaired. • Appearance of cranial incision: postoperative bulging or edema. • Vital signs: no change. • Cranial nerves: II (early papilledema), III (ptosis, abnormal pupillary responses) may be seen. • Seizure activity: may or may not occur. Increased Intracranial Pressure (IICP): • Signs and symptoms: – Late signs and symptoms: • LOC: requires more stimuli for response; low GCS score (coma). • Pupils: unilateral enlarging pupil, progressing to fixed and dilated; papilledema; progressing to bilateral fixed and dilated. • Motor: dense weakness. • Sensory: impaired. • Headache: worsening, with projectile vomiting. • Speech: may only groan to stimulus. Increased Intracranial Pressure (IICP): • Signs and symptoms: – Late signs and symptoms: • Respiratory: irregular rate and arrest if IICP not relieved. • Vital signs: rising systolic BP with widening pulse pressure, , fall in BP, temperature changes if IICP not relieved. • Cardiac: arrhythmias and cardiac arrest if IICP not relieved. • Cranial nerves: II (papilledema, decreased visual acuity), III, IV, VI (pupillary and eye movement dysfunction). • Abnormal reflexes: Babinski sign (planter reflex). Increased Intracranial Pressure (IICP): • Complication: – Respiratory and cardiac arrest. – Herniation of the brain: the protrusion of a portion of the brain through an opening or a defect in the skull. – Seizures. • Treatment: – Treatment focuses on: • Rapid detection. • Support of body systems (e.g., respiratory and cardiovascular): Control of fluid intake, fever, blood pressure and respiratory rate. Increased Intracranial Pressure (IICP): • Treatment: – Treatment focuses on: • Decrease ICP: – – – – Osmotic diuretics (e.g., mannitol). Loop diuretics (e.g., lasix). Corticosteroids (e.g., dexamethasone). Hyperventilation: believed to be an increase in the expiration of CO2 that causes blood vessels of the brain to be constricted. – Drainage of CSF. – Surgery (craniotomy) to remove any cause: lesion, hematoma, and abscess. Increased Intracranial Pressure (IICP): • Nursing Care: – – – – Assess neurological status frequently. Observe for S&S of IICP and notify physician. Assess V/S. Assess respiratory system frequently and provide respiratory care. – Elevate the head of the bed (at least 30 degree ) and avoid prone position and hip flexion. – Monitor intake and output. – Avoid other actions that may increase ICP such as giving suppositories and enemas. Increased Intracranial Pressure (IICP): • Nursing Care: – – – – – – – – – Care of the drainage system if applied. Help in diagnostic and treatment intervention. Take precautions for complication development. Keep quiet environment and administer analgesia as prescribed to control headache. Apply cold compresses and administer antipyretics medications. If there is a wound: prevent wound infection and give antitetanus. Provide good eye care and if patient is unconscious cover the eye and irrigate eye with N/S or artificial tears/2 hours. Initiate CPR and call CPR team if client is arrested. Provide self-care intervention. Herpes Zoster: • Herpes Zoster is inflammation of the nerve route ganglia caused by viral infection named varicellaZoster. • Clinical manifestation: – Clusters of small vesicles over the course of a peripheral sensory nerve. – Lesions in the chest or over the trigeminal nerve. – Crusts. – Sever pain and itching around the nerve, fever, and malaise. Herpes Zoster: • Management: – Acyclovir (zovirax). – Analgesia. – Antipruritic medication to decrease itching: calamine lotion. – Antibiotic. – Corticosteroids. • Complication: – Vision loss. – Diaphragm paralysis. – Muscle atrophy. Herpes Zoster: • Nursing care: – Administer medication as ordered. – Provide hygiene and be sure to not to transmitted the infection to other site of the body. – Monitor client for complication. – Frequently assess the skin condition especially involved area. – Provide adequate bed rest. – If there is an ulcer in the mouth, teach client to use analgesia, soft toothbrush, and eat soft food. – Reassure client that disease will subside. Spinal Cord Injuries: • Spinal cord injury (SCI) occurs from trauma to the spinal cord or from compression of the spinal cord due to injury to the supporting structures. • Causes of injury are motor vehicle accidents, violence, falls, and sport accidents. Spinal Cord Injuries: • Classification of injury: – Complete: • Complete disruption of the spinal cord functions(no impulses are carried below the level of injury) which depends on the level of injury including: – Motor (voluntary) movement. – Sensation. – Reflexes. – Incomplete: • Some of the spinal cord tracts are affected while others are able to carry impulses normally. Spinal Cord Injuries: • Clinical manifestation: – Spinal shock: • Cessation of motor, sensory, autonomic dysreflexia (an emergency situation resulting in a hypertensive crisis and possibly stroke or seizure activity), and reflex impulses (Areflexia: the absence of reflexes). • Affect the diaphragm and the respiratory function (accessory respiratory muscles). – Paraplegia (paralysis of lower extremities). Spinal Cord Injuries: • Clinical manifestation: – Quadriplegia (dysfunction or paralysis of both arms and legs). – Bowel and bladder paralysis with sexual dysfunction. – Neurogenic shock, a hypotensive situation resulting from the loss of sympathetic control of vital functions from the brain. This happens in clients with injury above the T6 vertebra. – Other symptoms: orthostatic hypotension, bradycardia, decreased cardiac output, loss of ability to sweat, and subnormal temperature. Spinal Cord Injuries: • Management: – Medical: • Medical management of the client with spinal cord injury begins prior to reaching the hospital. • Prevent further damage to the spinal cord by immobilizing the head, neck, and vertebral column with devices such as rigid cervical collars and splinting backboards. Spinal Cord Injuries: • Management: – Medical: • Traction may be used to maintain alignment of the spinal column. – Spinal cord traction: » Body casts and jackets are used to immobilize thoracic and lumbar fractures. » Provide ventilatory support as necessary. – Surgical: • Surgical interventions are performed for (according to the nature of the injury): – Decompression (Laminectomy: decompress the Spinal cord with placement of Harrington rods to stabilize the vertebral column). – Realignment (surgical manipulation of the vertebral column). Spinal Cord Injuries: • Management: – Pharmacological: • Steroid (SoluMedrol) (Decadron): therapy with dexamethasone – Is administered to prevent and reduce edema in the injured spinal cord → improve blood flow. • Osmotic diuretic (Mannitol): – May be administered to decrease and prevent cord edema. • Hypotensive drugs: – Hydralazine hydrochloride (Apresoline) or nifedipine is used to reduce blood pressure in cases of autonomic dysreflexia. – Activity: • Immobilization of the spinal column is necessary. Spinal Cord Injuries: • Management: – Rehabilitation (interdisciplinary approach): • Begins immediately, with a focus on preventing disabilities and maximizing and strengthening remaining functional ability. • Neurological function can be regained for up to 1 year. • Nursing care: – Prevent further damage to the spinal cord by immobilizing the head, neck, and vertebral column with devices such as rigid cervical collars and splinting backboards. – All trauma clients are treated as potential spinal cord injuries. – Assessment of airway, breathing, circulation, and disability (neurological assessment). Spinal Cord Injuries: • Nursing care: – Respiratory function is continuously assessed, and ventilatory support is provided as necessary (Mechanical ventilation may be required). – Assess vital signs especially blood pressure must be assessed immediately and monitored every few minutes until within normal limits and body temperature. – Subjective assessment involves eliciting input from the client regarding sensation, pain, and history of the accident. – Assess for skin condition, bowel and bladder function. – Discus with the client and his family about the injury (coping), the resulting disability, and the major lifestyle changes that have occurred should all be noted. Spinal Cord Injuries: • Nursing care: – Psychosocial assessment is very important to the well-being of the client. – Maintain care as immobile client. – Assess client for a distended bladder and empty the bladder if distended. – Observe for bradycardia, vasodilatation, flushing, and diaphoresis above the level of spinal cord injury. If these symptoms occur: • • • • Immediately notify the physician. Administer medications as ordered to decrease blood pressure. Raise head of bed and lower legs to reduce blood pressure. Remove the noxious stimuli, which may include constrictive clothing, shoes, splints, or linens. Multiple Sclerosis: • Multiple sclerosis (MS) is a chronic, progressive, degenerative disease wherein scattered nerve cells of the brain and spinal cord are demyelinated. • This myelinated sheath is involved in the conduction of impulses. • The disease interferes with the conduction of impulses A. normal nerve fiber and myelin sheath; B. MS destruction of myelin sheath Multiple Sclerosis: • The cause of MS is unclear but it is suggested that it is immune-mediated process with a viral activation. • Diagnosis is generally based on: – History and on elimination of other possible diagnoses. – MRI and CT scan can be used to identify lesions of sclerotic tissue as the disease progresses. – Cerebrospinal fluid reveals increased white blood cells, protein, and immunoglobulin (IgG). Multiple Sclerosis: • Symptoms: – Sensory: • Sensory symptoms may include visual disturbances, numbness, paresthesia, pain, and decreased sense of temperature. – Motor: • Motor symptoms may include decreased muscle strength, spasticity, paralysis, or bowel and bladder incontinence or retention. – Other disturbances: • • • • Ataxia (loss of balance or coordination). Nystagmus (constant, involuntary eye movements in any direction). Speech disturbances, tremors, and vertigo (dizziness). Sexual dysfunction and mood changes ranging from depression to euphoria (extreme happiness). Multiple Sclerosis: • Management: – There is no cure or specific treatment for MS. – Treatment goals are to limit exacerbations (relapsing), prevent complications, and maintain functional level. – Pharmacological: • The treatment of choice for relapsing-remitting MS is interferon beta for 2 or 3 months. • Steroids therapy: adrenocorticotropic hormone (ACTH) or prednisone is used to decrease periods of exacerbation. • The immunosuppressive agents (Imuran or cyclosporine) are administered to decrease immune response. Multiple Sclerosis: • Management: – Diet: • A well-balanced diet complete with roughage is necessary to promote bowel elimination. Plenty of fluids are also necessary. – Activity: • Physical therapy: to prevent contractures, maintain muscle strength, or prevent loss of function from spasticity, or for gait training. • Occupational therapy: to maintain or attain self-care. • Nursing management: – Assessment of signs and symptoms. – Assess motor status every 4 to 24 hours. – Passive/active ROM exercises should be done several times / day. – Encourage daily skills. Multiple Sclerosis: • Nursing management: – Turn bedridden clients every 2 hours. – Ambulate client four times daily with use of assistive devices as necessary. – Assess for bladder retention or incontinence. – Catheterize as necessary for retention or post-void residual. – Allow client to verbalize feelings. – Collaborate with other health care providers, such as mental health counselors and physicians. – Teach client about the disease process. – Educate client about decrease temperature sensation (advise him to be careful when cooking or otherwise around the kitchen stove and use bath thermometer to test bath water so as to prevent burning). Gillian-Barre Syndrome: • An acute inflammatory process primarily involving the motor neurons (Sensory neurons may also be affected) of the peripheral nervous system (spinal and cranial). • The demyelination process begins in distal nerves and ascends symmetrically. • Cause is not known, but most cases are preceded by a nonspecific infection. • Autoimmune or viral basis for this syndrome. Gillian-Barre Syndrome: • Clinical manifestations: – Motor weakness: motor weakness begins in the legs and progresses up the body. – Respiratory failure. – Facial muscle deficits. – Difficulty in swallowing. – Absence reflexes. – Sensory involvement causes paresthesia and pain in the hands and feet. The pain progresses up the body. Gillian-Barre Syndrome: • Stages of Guillain-Barre syndrome: – Acute onset, lasting 1 to 3 weeks. – The plateau period, lasting several days to 2 weeks. – Recovery phase, which involves remyelination and may last up to 2 years. Gillian-Barre Syndrome: • Management: – Medical: • The goal of medical management is prevention and treatment of complications such as immobility, infection, and respiratory failure. • Plasmapheresis (Plasma exchanges) removes the antibodies affecting the myelin sheath. • Occupational therapy activities teach the client to maintain optional self-care within the limitation of the disease process. – Pharmacological: • Steroids (ACTH and prednisone) and immunosuppressive agents (Imuran) are prescribed to slow the demyelination process. Antibiotics may be used. Gillian-Barre Syndrome: • Nursing care: – Assess the status of motor and sensory functions which are monitored continuously in the acute phase of the illness especially respiratory status. – Assess the Status of autonomic functions by assessment of blood pressure, cardiac rhythm, urinary elimination, and bowel sounds. – Ranges of motion and muscle strength are maintained through physical therapy every 2 to 4 hours. Gillian-Barre Syndrome: • Nursing care: – Position client to facilitate maximal expansion of the chest wall for optimal breathing. – Monitor vital signs (blood pressure, pulse, respiration, and temperature) every 2 to 4 hours. – Administer medication as prescribed. – Provide daily care needs that client is unable to perform. Bell's palsy: • Bell's palsy is a condition in which the motor component of the 7th cranial nerve and characterized by loss of the ability to move the muscles on one side of the face. • Signs and symptoms: – Pain in the face or behind the ear for 1-2 days before the paralysis started. – Inability to close the eye in the affected side. – Dropping of the mouth. – Loss of taste sense in 2/3 of the tongue. – Herpes lesion may appear in the ear. Bell's palsy: • Treatment: outpatient – – – – Analgesia. Anti-viral drugs: zovirax Corticosteroids: decrease inflammation. Muscle tone returns in few weeks and movement restored in months. • Nursing intervention: – – – – Gentle facial massage. Apply moist heat. Reassurance and psychological support. Apply medication. Trigeminal neuralgia: • Trigeminal neuralgia (nerve pain) is a condition of cranial nerve and characterized by period of sudden onset of pain and facial muscle contractions (lasting from seconds to minutes). • The period may last several weeks to months. • The pain follows one of the three branches of the Trigeminal nerve: – A. Ophthalmic branches. – B. Maxillary branches. – C. Mandibular branches. Trigeminal neuralgia: • The etiology of trigeminal neuralgia is not known, but the possible causes: – Injury. – Dental caries and dental work. – Anatomic position of the nerves. Trigeminal neuralgia: • Management: – Surgical: • Percutaneous electrocoagulation with radio frequency to relieve pain. This procedure affects the pain-sensory fibers. – Pharmacological: • Phenytoin (Dilantin) and carbamazepine (Tegretol) are used to shorten the length of pain. • Nerve blocks using alcohol and phenol injections into the nerve provide temporary relief for 8 to 16 months. Trigeminal neuralgia: • Nursing Management: – Goals of nursing interventions are: • Relief of pain. • Prevention of self-care deficits. • Promotion of social interaction. • Prevention of injury (eye injury). Trigeminal neuralgia: • Nursing interventions: – Provide good oral hygiene (trigeminal neuralgia cause severe pain that cleaning, talking, and eating are avoided). – Help the client in identifying both the trigger points that stimulate the pain and ways to avoid those areas without neglecting daily needs. – Instruct client not to touch his eye and to observe for redness of the eye and conjunctiva. – Encourage routine visits to the dentist for oral examination. Trigeminal neuralgia: • Nursing interventions: – Administer medication. – Educate client and family member about the disease and encourage social relationships. – Instruct client to have dental work done during a period of remission (decrease pain). – Inform the dentist about his condition. – Maintain good dental hygiene, especially during remission. Unconsciousness: • Definition: – A condition in which the patient is unresponsive to and unaware of environmental stimuli. • Coma: – Clinical state of unconsciousness in which the patient is unaware of self or the environment for prolonged periods. • Unconsciousness itself is not a disease or a diagnoses but rather a manifestation of a large number of pathophysiological processes, including trauma, metabolic disturbances, mass lesions, and infections. Unconsciousness: • Causes Of Unconsciousness: – Psychiatric disorders: • Depression, catatonia and schizophrenia. – Supertentorial Mass: • Epidural hematoma, cerebral infarction, brain tumor, brain abscess. – Subtentorial Lesions: • Brainstem infarction, brainstem hemorrhage, cerebellar hemorrhage. Unconsciousness: Potential complications: • Respiratory failure. • Pneumonia. • Pressure ulcers. • Aspiration (gastric feeding) • Immobility. • Pressure sores. • Venous stasis. • Musculoskeletal deterioration. • Disturbed GI. Unconsciousness: • Planning and goals: – – – – – – – – – – – Maintenance of a clear airway. Protection form injury. Attainment of fluid volume balance. Achievement of intact oral mucus membranes. Maintenance of normal skin integrity. Absence of corneal irritation. Absence of complications. Attainment of thermoregulation. Absence of urinary retention and infection. Absence of diarrhea or fecal impaction. Maintenance of intact family or support system. Head Injury: • Head injury includes any trauma to scalp, skull or brain, includes an alteration in consciousness. • Types of Head Injury: – Scalp Lacerations: • Most minor of the head traumas. • Because your scalp contains many blood vessels with poor constructive abilities, most scalp lacerations are associated with profuse bleeding. • The major compilation is infection. Head Injury: • Types of Head Injury: – Skull Fractures: • Frequently occurs with head trauma. • Frontal fracture: – Exposure of brain to contaminants through frontal air sinus. – CSF Rhinorrhea (CSF leakage from the nose) or otorrhea (from the ear). • Orbital fracture: – Raccoon eyes (periorbital ecchymosis) • Temporal Fracture: – Battle sign. – Oval shaped bruise behind the ears. Head Injury: • Types of Head Injury: – Skull Fractures: • Parietal Fracture: – – – – – Deafness, CSF or brain otorrhea, facial paralysis, loss of taste; battle sign. • Posterior fossa fracture: – Occipital bruising resulting in blindness, – visual field defects, – rare appearance of ataxia. Head Injury: • Types of Head Injury: – Skull Fractures: • Basilar skull fracture: – – – – – – CSF or brain otorrhea, bulging of tympanic membrane caused be CSF or blood, battle sign, tinnitus or hearing difficulty, facial paralysis, vertigo. Head Injury: • Types of Head Injury: – Concussion: • Minor head injury. • A sudden transient mechanical head injury with disruption of neural activity and a change of LOC. • The patient may not loss total consciousness with this injury. • Signs: – Brief LOC, – Amnesia (of incident), – Headache. • If the unconsciousness lasted less than 5 minutes the patient is usually sent home with instructions of when to notify MD. Head Injury: • Types of Head Injury: – Brain Contusions: • Major head injury. • Bruising of the brain tissue within a focal area that maintains the integrity of the pia mater and arachnoid layers. • A contusion develops area of necrosis, infarction, hemorrhage and edema. • Usually occurs at the site of the fracture. • Bleeding at the site is usually minimal and the blood is reabsorbed slowly. • Seizures are a common complication of brain contusion. – Brain Lacerations: • Major head injury. Head Injury: • Types of Head Injury: – Brain Lacerations: • Involve actual tearing of the brain tissue and occur frequently in association with depressed and compound fractures and penetrating injuries. • Tissue damage is severe and surgical repair of the laceration is impossible because of the texture of the brain tissue. • Signs and symptoms: – – – – – Hemorrhage, Hematoma formation, Seizures, Cerebral edema. Prognosis is usually very poor when a patient has a hemorrhage. Head Injury: • Types of Head Injury: – Brain Lacerations: • Etiology: – Blunt – MVA, Pedestrian event, fall, assault, sports injury. – Penetrating – gun shot wound, arrow. • Complications: – – – – Epidural Hematoma. Subdural Hematoma. Chronic subdural hematoma. Intracerebral Hematoma. Head Injury: • Diagnostic Studies: – Skull x-rays r/o skull fx and facial fx. – CT scan and MRI r/o cranialcerebral trauma, Allows for rapid dx’s – PET differentiates head injuries. – Transcranial Doppler allow for measurement of cerebral blood flow velocity. Head Injury: • Collaborative Care: – – – – – – – – – – – Ensure patent airway. Administer O2. Establish IV access. Monitor V/S, LOC, O2 sat, cardiac rhythm, GCS, pupil size & reactivity Skull Fracture , craniotomy or craniectomy maybe necessary. Promote nutrition. Prevent injury. Maintain body temperature. Maintain skin integrity. Prevent sleep disturbance. Support family. Head Injury: • Nursing Diagnoses: – Ineffective airway clearance and ventilation r/t hypoxia. – Fluid volume deficit r/t disturbances of consciousness and hormonal dysfunction. – Altered nutrition r/t metabolic changes, fluid restriction, and inadequate intake. – Risk for injury r/t disorientation, restlessness, and brain damage. – Pain r/t headache, nausea and vomiting. – Self-esteem disturbance r/t altered appearance of head and face. Head Injury: • Planning: – Maintain adequate cerebral perfusion; remain normthermic; be free from pain and infection and maintain max cognitive, motor and sensory function. • Nursing Implementation: – Health Promotion- to Prevent head injuries promote safety driving, use of seat belts and helmets. – Avoid driving while under the influence of alcohol. – Educate parents on the proper use of seat belts and restraints for their children. – Patient and Family Teaching. Head Injury: • Nursing Implementation: – Home Care –Notify MD if pt with s/s of: • • • • • • Increased drowsiness. Nausea/vomiting. Worsen HA or stiff neck. Seizures. Vision difficulties. Behavior change. Glasgow Coma Scale: • GCS- uses three indicators of response are evaluated. – Opening of the eyes. – Best verbal response. – Best motor response. • Specific behaviors are seen and given a numeric value and can be plotted on a graph. • The higher the scores, the higher the level of brain functioning. Intracranial Pressure: • Normal ICP – is the pressure exerted by total volume from 3 components within the skull: brain tissue, blood, and CSF. • Head of bed elevated 30 degree, ICP 0-15 mmHg. • Normal compensatory adaptations: – – – – Dispensability of dura, increased venous outflow, decreased CSF production, changes in intracranial blood volume via constriction & dilation & slight compression of brain tissue. Cerebral Blood Flow: • CBF is the amount of blood in ML passing through 100 g of brain tissue in 1 min. CBF 50 ml/min. • Brain requires 20% of the body’s oxygen and 25% of its glucose. • Autoregulation: – Ensures a consistent CBF to provide for metabolic needs to maintain cerebral perfusion pressure. Cerebral Blood Flow: • Autoregulation: – Normal MAP 50 mm hg, below this CBF decreases s/s – cerebral ischemia, I.e, syncope & blurred vision. – The systemic arterial pressure that autoregulation is effective is 150 mm hg. When this pressure is exceeded, vessels are constricted. – Resulting in an increase ICP. – CPP=MAP-ICP. – Oxygen tension, carbon dioxide tension and hydrogen ion concentration affect cerebral tone. Cerebral Edema: • Cerebral edema results in an increase in tissue volume that may increase ICP. • 3 types of cerebral edema: – Vasogenic cerebral edema, – Cytotoxic. – Interstitial cerebral edema. • Complications: – Major complications are cerebral herniation, if unrelieved respiratory arrest may occur. Cerebral Edema: • Clinical manifestation: – Change in LOC, – Change in V.S, – Ocular signs, decrease in major function, headache and vomiting. – Loss of consciousness confuses clinical s/s of increased ICP. • Diagnostic Studies: – Identifying the underlying cause of >ICP. – MRI, CT, cerebral angiography, EEG, cerebral blood flow, transcranial – Doppler studies. Cerebral Edema: • Collaborative Care: – – – – Preventing secondary injury to brain. Oxygenation to support brain function, Pao2 @ 100 mm hg or>. ET or tracheostomy to maintain ventilation/ Mechanical ventilation. If cause by mass lesion I.e, tumor or hematoma, surgical removal of mass maybe necessary. – Drug Therapy: • • • • Osmotic diuretics. Loop diuretics. Corticosteroids therapy. High dose barbiturates e.g., pentobarbital and thiopental. – Hyperventilation therapy. – Nutritional therapy. Cerebral Edema: • Nursing Assessment: – Subjective & objective data. – GCS data. – Mental status, cranial nerve functioning, motor functioning, sensory status, cerebellar functioning and reflexes. – Pupil size & response. Cerebral Edema: • Nursing Diagnoses: – Altered cerebral tissue perfusion r/t cerebral tissue swelling AEB MS ICP> 20 mm Hg. – Risk of infection r/t immobility. – Risk for impaired skin integrity r/t nutritional deficit and immobility. • Planning: – Goals: • Client will: – Have decreased ICP to within normal limits. – Maintain patent airway. – Demonstrate normal fluid and electrolyte balance. Cranial Surgery: • Types of cranial surgery: – – – – – – Burr hole, Craniotomy, craniectomy, Cranioplasty, Stereotaxis Shunt procedures. • Preoperative evaluation: – CT scan: • To demonstrate the lesion and show the degree of surrounding brain edema, the ventricular size, and the displacement. Cranial Surgery: • Preoperative evaluation: – MRI: • Provides information similar to that of the CT scan and examines the lesion in other planes. – Angiography: • Used to study the tumor’s blood supply or give information about vascular lesions. – Transcranial Doppler: • Studies are used to evaluate the blood flow of intracranial blood flow. Cranial Surgery: • Complications of intracranial surgery: – Increased ICP, infection and neurologic defiects. – Increased ICP may develop as a result of cerebral edema or swelling and is treated with mannitol and use of paralyzing agents. • Preoperative management: – Anticonvulsant medication before surgery to reduce the risk of poet-op seizures. – Steroids (Dexamethasone) may be administered to reduce cerebral edema. – Fluids may be restricted. – Hypertonic solutions such as as mannitol and a diuretic lasix may be given IV immediately before and sometimes during surgery if the patient tends to retain fluids. Cranial Surgery: • Preoperative management: – Nursing diagnosis: • Altered cerebral tissue perfusion r/t to cerebral edema. • Potential for ineffective thermoregualtion r/t damage to the hypothalamus, dehydration, and infection. • Potential for gas exchange. • Potential complications. • Increased ICP. • Bleeding and hypovolemic shock. • Fluid and electrolyte disturbances. • Infection. • Seizures. Cranial Surgery: • Preoperative management: – Arterial line and a venous line may be placed to monitor blood pressure and central venous pressure. The patient may be intubated and may receive supplemental o2 therapy. – Reduce cerebral edema. – Relieving pain and [preventing seizures. – Monitoring ICP. – Planning: • Pt w/ cranial surgery will return to normal consciousness, be free from pain & discomfort, maximize neuromuscular functioning and be rehabilitated to maximum ability. Cranial Surgery: • Preoperative management: – Nursing intervention: • • • • • • Achieving neurologic homestasis. Regulating temp. Improving gas exchange. Managing sensory deprivation. Enhancing self-image. Monitoring and managing potential complications. Seizure Disorders: • A seizure is a uncontrolled discharge of neurons in the brain that interrupts normal function. Seizures are frequently symptoms of an underlying illness. • Epilepsy is a condition in which a person has spontaneously recurring seizures caused by a chronic underlying condition. • Etiology & Pathphysiology: – Most common cause 1st 6 mos of life are congenital defects from birth injury. – 2 - 20 y.o. infection, trauma & genetic factors. – 20 - 30 y.o. structural lesions I.e., trauma, brain tumors or vascular disease. – After 50 y.o primary cause are cerebrovascular lesions & metastic brain tumors. Seizure Disorders: • Clinical Manifestations: – Phases of seizures: • • • • The prodromal phase w/ signs activity, which precede a seizure. The aural phase w/ a sensory warning. The ictal phase w/ full seizure. Postictal phase, which is the period of recovery after the seizure. – Partial seizures: • Partial seizures are focal in origin and affect only part of the brain. • Here maybe a finger or hand shakes. Maybe the mouth jerks. • The person may talk unintelligibly, may be dizzy and may experience unusual or unpleasant sights, sounds, odors, or taste, but without loss of consciousness. (AURA) Seizure Disorders: • Clinical Manifestations: – Partial seizures: • SIMPLE Partial seizures: elementary symptoms, generally without impairment of consciousness. • COMPLEX partial seizures: generally with impairment of consciousness. – Generalized seizures: • Generalized Seizures the entire brain is affected at the onset, there is no warning or aura, lost of consciousness for sec to min. • Tonic-Clonic seizures: – Most common loss of consciousness & falls, – stiffening of body (tonic phase)10-20 sec & jerking of extremities (clonic phase) for 30-40 seconds. Seizure Disorders: • Complications: – Physical: • Status epilepticus rapid succession of seizures. Pt. dose not regain consciousness a neurologic emergency. – Tonic-Clonic: • • • • • Ventilatory insuffiency, Hypoxemia, Cardiac arrhythmias, Hyperthermia Systemic acidosis. Seizure Disorders: • Complications: – Severe injury and even death from trauma can occur during a seizure. – Epileptic pt’s who lose consciousness are at risk, death can result from a head injury incurred in a fall, drowning in a tub or from severe burns. – Psychosocial. – Lifestyle: • • • • Social stigma. Discrimination. Transportation. Ineffective method of coping. Seizure Disorders: • Diagnostic Studies: – – – – – – CBC. Urinalysis. Electrolytes, creatinine, fasting blood Glucose. Lumbar puncture. CT, MRI, Pet scan. Electroencephalography. • Collaborative Care: – – – – – Antiseizure medication. Surgery. Vagal nerve stimulation. Psychosocial counseling. Alternative therapy – biofeedback. Seizure Disorders: • Nursing Management: – Subjective & objective data. – Planning: • Pt will be free from injury during a seizure, • have optimal mental and physical functioning while taking antiseizure medication, • Have satisfactory psychosocial functioning. – Nursing Care Plan: • • • • • Ineffective method of coping. Risk for injury. Ineffective airway clearance. Ineffective mgt of therapeutic regimen r/t lack of knowledge. Self-esteem disturbance r/t diagnoses of epilepsy. Seizure Disorders: • Nursing Implementation: – Health Promotion: • general safety,practice good health habits. – Acute Intervention: • observation, treatment of seizure, education and psychosocial intervention. – Ambulatory and Home Care: • • • • • • Medication taken regularly. Do not adjust dose w/o MD. Educate family members re: emergency management. Wear a medic alert bracelet or ID card. Avoid excessive alcohol, fatigue and loss of sleep. Regular meals & snacks in between if faint, shaky or hungry