MEDICAL EMERGENCY 3rd lecture for 3rd year
advertisement

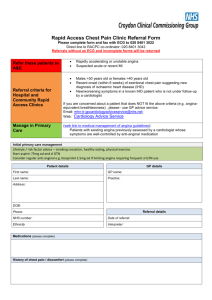
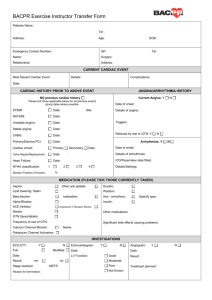
ADRENAL INSUFFICIENCY • The adrenal cortex produces mineralocorticoids and glucocorticoids that are important in maintaining fluid volume. • Cortisol, the principal glucocorticoid, maintains extracellular fluid. • Aldosterone, the principal mineralocorticoid, regulates salt and water balance. • Insufficient production of these hormones can result from primary (Addison’s disease) or secondary adrenal disease. • - • • Primary Adrenocortical Insufficiency Caused by a progressive destruction of the adrenal cortex. Idiopathic nature Autoimmune Hemorrhage Sepsis Infectious diseases (such as tuberculosis, human immunodeficiency virus, cytomegalovirus and fungal infection) Malignancy Adrenalectomy Drugs Clinical evidence of the deficiency generally arises only after 90 percent of the adrenal cortices have been destroyed. Affected patients have high levels of adrenocorticotropic hormone or ACTH in blood, and a very low to undetectable level of aldosterone and cortisol in blood. Secondary Adrenocortical Insufficiency • Results from hypothalamic or pituitary disease and from the administration of exogenous corticosteroids. Although classified together, these two entities have different physiological effects. • In the absence of hypothalamic or pituitary function, the adrenal cortex undergoes irreversible atrophy. • Long-term administration of corticosteroids blunts adrenal cortical function, with variable and reversible effects. • Cases of hypothalamic-pituitary disease are less common than those induced by use of corticosteroids. ADRENAL CRISIS • The most acute adverse outcome of AI is adrenal crisis. This event can occur when a patient with AI, most commonly in the form of Addison’s disease, is challenged by stress (Eg; illness, infection or surgery) and in response is unable to synthesize adequate cortisol & aldosterone. • This life-threatening emergency usually evolves slowly during a few hours and then is manifested by severe exacerbation of the condition including profuse sweating, hypotension, weak pulse, cyanosis, nausea, vomiting, weakness, headache, dehydration, fever, sunken eyes, dyspnea, myalgia, arthralgia, hyponatremia & eosinophilia. • If not treated rapidly, patient can develop hypothermia, severe hypotension, hypoglycemia, confusion and circulatory collapse. ACUTE ASTHMA • Asthma is described as a chronic inflammatory disorder involving many cell types, manifesting with episodes of chest tightness, coughing, labored breathing and wheezing, all of which are related to bronchiole inflammation. Symptoms can last for a few moments or as long as days. • The airway obstruction in asthma is initiated by inflammation and muscle spasm but is mostly reversible. • It generally is believed that both genetic and environmental factors, as well as allergens, are important in the initiation and continuation of the airway inflammation. MANAGEMENT IN DENTAL CARE CHEST PAIN (ANGINA PECTORIS ) • Angina pectoris commonly known as angina is severe chest pain due to ischemia (a lack of blood supply, hence a lack of oxygen supply) of the heart muscle, generally due to obstruction or spasm of the coronary arteries. • Coronary artery disease, the main cause of angina, is due to atherosclerosis of the cardiac arteries. Classification • Stable angina • Unstable angina • Stable angina / effort angina is that of chest discomfort and associated symptoms precipitated by some activity (running, walking, etc.) with minimal or non-existent symptoms at rest. • Unstable angina occurs at any time and should be considered and managed as a form of acute coronary syndrome. Signs and Symptoms • Most patients with angina complain of chest discomfort rather than actual pain described as a pressure, heaviness, tightness, squeezing, burning, or choking sensation. • Apart from chest discomfort, anginal pains may also be experienced in the epigastrium (upper central abdomen), back, neck area, jaw, or shoulders. This is explained by the concept of referred pain, and is due to the spinal level that receives visceral sensation from the heart simultaneously receiving cutaneous sensation from parts of the skin. • Typical locations for referred pain are arms often inner left arm, shoulders, neck and into the jaw. • Angina is typically precipitated by exertion or emotional stress. It is exacerbated by having a full stomach and by cold temperatures. • The pain usually lasts for about 3 to 5 minutes but the symptoms actually starts 15 to 20 minutes before the pain and is relieved by rest or specific anti-angina medication. MANAGEMENT OF CHEST PAIN WITH ANGINA PECTORIS Recognize problem (chest pain, patient states he/she is having an anginal attack) Discontinue dental treatment Activate office emergency team P— Position patient comfortably A- B- C- Assess airway, breathing, and circulation D— Provide definitive management HISTORY OF ANGINA PRESENT Administer vasodilator and O, (up to 3 doses) NO HISTORY OF ANGINA Activate EMS, STAT IF PAIN IF PAIN DOES administer O2 and RESOLVES NOT RESOLVE consider nitroglycerin Consider future dental Activate EMS Administer Aspirin Monitor and record vital signs Monitor and record ACUTE MYOCARDIAL INFARCTION • Commonly known as a heart attack, is the interruption of blood supply to part of the heart, causing heart cells to die. • This is most commonly due to occlusion (blockage) of a coronary artery following the rupture of a vulnerable atherosclerotic plaque, which is an unstable collection of lipids (fatty acids) and white blood cells (especially macrophages) in the wall of an artery. • The resulting ischemia and oxygen shortage, if left untreated for a sufficient period of time, can cause damage or death of myocardium. • Classical symptoms of acute myocardial infarction include sudden chest pain (typically radiating to the left arm or left side of the neck), shortness of breath, nausea, vomiting, palpitations, sweating and anxiety. • Immediate treatment for acute myocardial infarction includes aspirin, sublingual nitroglycerin & oxygen. MANAGEMENT OF PATIENT WITH ACUTE MI Recognize problem (chest pain, patient states he/she is having an anginal attack) Discontinue dental treatment Activate office emergency team P— Position patient comfortably A- B- C- Assess airway, breathing, and circulation D— Provide definitive management HISTORY OF ANGINA PRESENT NO HISTORY OF ANGINA Administer vasodilator and O, (up to 3 doses) IF PAIN Activate EMS, STAT administer O2 and RESOLVES consider nitroglycerin Consider future dental Administer Aspirin Treatment modifications Manage pain (parentral opiods, N2O-O2) Monitor and record vital signs Prepare to manage complications (eg: sudden cardiac arrest) Stabilize and transfer to hospital ICU Cardiac Arrest • Cardiac arrest or circulatory arrest is the cessation of normal circulation of the blood due to failure of the heart to contract effectively and if this is unexpected can be termed a sudden cardiac arrest. • Cardiac arrest is different from (but may be caused by) a heart attack, where blood flow to the muscles of the heart is impaired. • Arrested blood circulation prevents delivery of oxygen to the body. Lack of oxygen to the brain causes loss of consciousness, which then results in abnormal or absent breathing. Brain injury is likely if cardiac arrest goes untreated for more than five minutes. • Cardiac arrest is a medical emergency that in certain situations is potentially reversible if treated early. • The treatment for cardiac arrest is cardiopulmonary resuscitation (CPR) to provide circulatory support, followed by defibrillation. Causes • Coronary heart disease is the leading cause of sudden cardiac arrest. 60-70% is related to coronary heart disease. • A number of other cardiac abnormalities can increase risk including: cardiomyopathy, cardiac rhythm disturbances, hypertensive heart disease, congestive heart failure. • Non-cardiac : Trauma, non-trauma related bleeding (such as gastrointestinal bleeding, aortic rupture, and intracranial hemorrhage), overdose, drowning & pulmonary embolism. Management CA is managed in five stages 1. initial response 2. basic life support 3. advanced life support 4. post resuscitation care 5. long term management Choking and Foreign Body Airway Obstruction • Choking is the physiological response to sudden airway obstruction. Obstruction may be partial or complete. • Foreign body airway obstruction (FBAO) causes asphyxia occurring very acutely, with the patient often unable to explain what is happening to them and with rapid loss of consciousness and death if first aid is not undertaken quickly and successfully. Immediate recognition and response is of the utmost importance. • Any object routinely placed into or removed from the oral cavity during dental or surgical procedures can be aspirated or swallowed. These items can include teeth, restorations, restorative materials, instruments, implant parts, rubber dam clamps, gauze packs and impression materials. The possibility of swallowing or aspirating an object is increased by the common practice of placing the patient in a supine position or semi-spine position. • Other factors that may increase the possibility of aspiration include age (a decreased gag reflex in elderly patients), medical conditions (such as stroke, dementia and Parkinson's disease), use of local anesthetics and altered states of consciousness associated with intravenous sedation. • The consequences of aspirating a foreign object or material can range from immediate obstruction of the airway to long lasting pulmonary complications. Early complications can include hypoventilation of the distal lung segment with subsequent atelectasis and hypoxia. Later complications can include infection, such as lung abscess or pneumonia, and atelectasis. Management • Action depends upon the severity of the situation and the adequacy of the cough. It may be classified as: 1. Mild 2. Severe but conscious 3. Severe and unconscious • In mild airway obstruction encourage him to keep coughing but more dramatic action is unnecessary. • If there is severe airways obstruction but he is conscious, give 5 blows to the back. • Stand to the side and slightly behind the victim, preferably to the left if you are right handed and the right if you are left handed. • Support the chest with one hand and lean the victim well forwards so that when the obstructing object is dislodged it comes out of the mouth rather than goes further down the airway. • Give a sharp blows between the scapulae with the heel of the hand. • After each blow, reassess the patient to see if the foreign body has moved. • If the airways are still obstructed, repeat the blow and reassess until 5 blows have been delivered. If this does not work, use the Heimlich maneuver (or abdominal thrust). HYPERTENTION • Elevated blood pressure for long time period (chronic) due to unknown cause is called essential hypertension. • Mild to moderate hypertension with systolic pressure of less than 200 or diastolic pressure of less than 110 is usually not a problem to the performance of ambulatory oral surgical care, but more than this value if present in a patient who needs elective oral surgery, then blood pressure is first controlled and surgery is postponed. • Care includes anxiety reduction protocol and monitoring of vital signs. • Epinephrine containing local anesthetics should be used cautiously.