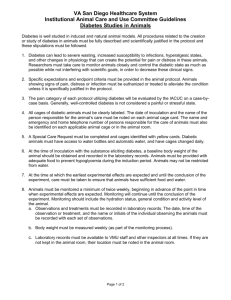
Pathology of diabetes complications
advertisement

Diabetes Mellitus complications.II PATHOGENESIS OF THE DM • Multifactorial, although persistent hyperglycemia (“glucotoxicity”) seems to be a key mediator. • Some tissue do not require insulin for glucose transport (e.g., nerves, lenses, kidneys, blood vessels), • DM- widely affect different vascular structures: • 1) Both large& Medium-sized muscular arteries (macrovascular disease) - accelerated atherosclerosis (MI, infarction,CVA) • 2) Capillary dysfunction in target organs (microvascular disease). • The assessment of glycemic control is best measure by glycosylated hemoglobin, also known as HbA1C, which is formed by nonenzymatic covalent addition of glucose moieties to hemoglobin in red cells. • The American Dietetic Association recommends that HbA1C be maintained below 7% in diabetic patients PATHOGENESIS OF THE DM • Hyperglycemia is not the only factor responsible for the long-term complications of diabetes. • The underlying abnormalities also play great role are: • (1) Insulin resistance, (2) Co-morbidities e.g obesity. • Three distinct metabolic pathways have been implicated in the deleterious effects of persistent hyperglycemia on peripheral tissues: • I) Formation of Advanced Glycation End Products. • II) Activation of Protein Kinase C. • III) Intracellular Hyperglycemia and Disturbances in Polyol Pathways. PATHOGENESIS OF THE DM • Three distinct metabolic pathways • I) Formation of Advanced Glycation End Products-AGE. • A) AGE-RAGE signaling axis: accelerates vessel injury&microangiopathy, which is expressed on inflammatory reaction (endothelial SMA, macrophages and T cells) - CK& GF \reactive oxygen species\procoagulant activit\ Proliferation of SM& synthesis of ECM. • B) AGEs Cross-linking with(collagen type I in BV& type IV in BSM& Protein) = Decreases their elasticity (Type I)+Increases extravasation of fluid (Type IV) + Decreases protein removal while enhancing protein& LDL deposition. • II) Activation of Protein Kinase C (PCK): activation signal by Ca[2]+ ions & 2nd messenger diacyl glycerol (DAG). • Intracellular hyperglycemia stimulates>> synthesis of DAG from glycolytic intermediates>> activation of PKC>>lead: Production of (VEGF)=retinopathy+ Vasoconstrictor endothelin-1 ↓ levels NO “dilator” +Profibrogenic factors like TGF-β , ↑ECM+ Production of PAI-1> ↓↓fibrinolysis> vascular occlusive+ ↑↑ Pro-inflammatory factor (CK) PATHOGENESIS OF THE DM • Three distinct metabolic pathways • III) Intracellular Hyperglycemia and Disturbances in Polyol Pathways.(lense , kidneys , nerves, blood vessels) • This excess glucose is metabolized by the enzyme Aldose reductase to sorbitol, a polyol, &to fructose, uses NADPH-co-factor>> Progressive ↓↓ NADPH by aldol reductase compromises GSH regeneration, increasing cellular susceptibility to oxidative stress. Morphology of DM& Its late complication. The most important morphological changes in DM are not related to pancreas (which is widely varies), but to late systemic complication. These are the major causes of morbidity and mortality. Principal organs affected in diabetes mellitus : Pancreas ( Islet Changes ) Diabetic Macrovascular Disease ( atherosclerosis) Diabetic Microangiopathy (Small vessels ) Diabetic Nephropathy (Kidneys). Diabetic Ocular Complications (Retinopathy) eye Diabetic Neuropathy (Nerves ). 1)Pancreas: Surprisingly , pancreatic lesions are neither constant nor necessarily pathognomonic. They are more likely to be distinctive in typeI >> in typeII. One or more of the following alterations may be present: 1. Reduction in the size and number of islets (DM-1) ↓islet mass (DM-2). 2. Increase in the size and number of islet s (nondiabetic newborns of diabetic mothers). 3. Beta cell degranulation. 4. Leukocytic infiltration (insulitis)- mostly T- cells, Eosinophilic infiltrates (Autoimmune diseases) 5. Amyloid replacement of islets (DM-2)_ around capillaries & b\w islet cells> obliteration & fibrosis. 6. Fibrosis of islet. Insulitis- Type I DM Amyloidosis- type II DM Blood vessels. Small vessels (Diabetes microangiopathy) . Diffuse thickening of basement membrane, more in the capillaries of the skin , skeletal muscles, retina , renal glomeruli , and renal medulla. However, it may also be seen in such nonvascular structures as renal tubules, Bowman’s capsule, peripheral nerves and placenta. Morphologic features: Thickening appears as widening of the basement membrane by a homogeneous , sometimes multilayered hyaline substance , which is strongly positive with PAS stain. Diabetic capillaries are more leaky than normal to plasma proteins. Diabetic Macrovascular Disease (Atherosclerosis). 1) Endothelial dysfunction- predisposes (LDL deposition)& Myocardial diseases. 2) Accelerated atherosclerosis(large arteries: CVS, renal& CNS) whatever their ages, within a few years of onset of type I&II. 3) Myocardial infarction, caused by AT of coronary arteries. 4) Gangrene of the lower extremities (vessels of lower extremities) Hyaline arteriolosclerosis • It is not specific for diabetes, a\w HTN. • More severe in diabetics than in nondiabetics. • It takes the form of an amorphous, hyaline thickening of the wall of the arterioles, which causes narrowing of the lumen Kidneys. (Diabetic Nephropathy ). • The kidneys are second target for DM after the heart . • The second leading cause of death after MI from DM. • Three lesions are encountered: • (1) Glomerular lesions: Capillary BM thickening by (EM), Tubular BM thickening, Diffuse mesangial sclerosis with increase in mesangial matrix > with time become nodule in configuration. Nodular “intercapillary” glomerulosclerosis=Kimmelstiel-Wilson dis. (ovoid or spherical, often laminated, nodules of mesangial matrix situated in the periphery of the glomerulus+ Glomeruli arterioles show hyalnosis+ uninvolved lobules &glomeruli show striking diffuse mesangial sclerosis). • (2) Renal vascular lesions, principally arteriolosclerosis of • diabetic patients (severe changes in the arteries& arterioles). • (3) Pyelonephritis, including necrotizing papillitis: • Acute or chronic inflammation started in interstitium & then spread to the tubules.+ Necrotizing papillitis=papillary necrosis. Severe renal hyaline (afferent art.) arteriolosclerosis Nephrosclerosis long-standing DM thickening of tubular BM Nodular “intercapillary” glomerulosclerosis Glomerular involvement a-Diffuse glomerulosclerosis. This consists of diffuse increase in mesagial matrix with mild proliferation of mesangial cells, and is always associated with the overall thickening of the GBM. The increase in mesangial volume appears to lag slightly behind basement membrane widening but becomes pronounced after ten to 20 years of diabetes. The matrix depositions are PAS positive. The changes almost always begin in the vascular stalk and sometimes seem continuous with the invariably present hyaline thickening of arterioles .As the diseases progresses, the mesangial areas expand further and obliterate the mesangial cells ,gradually filling the entire glomerulus (obliterative diabetic glomerulosclerosis). b-Nodular glomerulosclerosis. This is also known as intercapillary glomerulosclerosis of Kimmelstiel -Wilson disease. The glomerular lesion takes the form of ovoid or spherical , often laminated , hyaline masses situated in the periphery of the glomerulus .The nodule are PAS positive and contains lipids and fibrin .Often they contain trapped mesangial cells.The nodular lesion is virtually pathognomonic of diabetes. c-Exudative lesions .(Fibrin cap. And capsular drop.). The fibrin cap appears as homogeneous , brightly eosinophilic, crescentic subendothelial deposit in a peripheral capillary .The capsular drop is an eosinophilic , focal thickening of the parietal layer of bowman’s capsule , which apparently hangs into the uriniferous space . The capsular drop is PAS positive and contains plasma proteins. 2. Vessels involvement : Capillary basement membrane thickening, widespread thickening of the glomerular capillary basement membrane (GBM) occurs in virtually all diabetics, irrespective of the presence of proteinuria ,and is part and parcel of the diabetic microangiopathy . Pure capillary basement membrane thickening can be detected only by electron microscopy .Careful morphometric studies demonstrate that this thickening begins as early as two years after the onset of juvenile diabetes , and by five years amounts to about a 30% increase80. the thickening continues progressively , and usually concurrently with mesangial widening . Simultaneously there is thickening of the tubular basement membranes. Renal atherosclerosis and arteriolosclerosis (hyaline) 3. Stroma : The diabetes increase the susceptibility to the development of Pyelonephritis and particularly papillary necrosis (necrotizing papillitis) Eyes. ( diabetic Retinopathy) . Diabetes retinopathy classified in two groups : Diabetes microangiopathy(non proliferative) may present as (a) Thickening of the Basement membrane lead >> (a-1) Breakdown of the blood-retinal barrier lead to leakage with micro-occlusion >> giving rise to Macular edema (VISUAL LOSS). (b) Pericyte degeneration >> (c) Microaneurysms >>> (d) Retinal microhemorrhages 1) Intraretinal angiogenesis (proliferative phase) (of the disc or elsewhere) known intraretinal microangiopathy= (a) Retinal neovascularization (disrupted neovascular membrane)>> Posterior vitreous detachment > Massive vitreous hemorrhage. (b) Organization >> (c ) Retinal traction >> ( d) Retinal detachment >> (e ) Visual distortion. Eyes. ( Anterior chamber complications) . 1. CATARACT- lenticular opacities, opacification of the lens nucleus (nuclear sclerosis). 2. Development of Neovacular membrane on iris surface (a) Retinal neovascularization accompanied by >> (b) Development of IRIS neovascular membrane >> (c) Increased levels of VEGF in the aqueous humor.>> 3. Neovascular glaucoma: (a) Contraction of the iris neovascular membrane >> (b) Lead to adhesions >>> (c) Occluding a major pathway for aqueous outflow>> (d) Elevation of the intra-ocular pressure. Proliferative retinopathy. This occurs in response to severe ischemia and hypoxia of the retina.( retinitis proliferans) .Is defined by the appearance of new vessels on the surface of either the optic nerve head, which is termed neovascularization of the disc, or the surface of the retina (neovascularization elsewhere) Nerves ( Diabetic Neuropathy ). •80% of DM> more than 15 years. • Categorize as distal symmetric sensory or sensorimotor neuropathy, autonomic neuropathy, and focal or multifocal asymmetric neuropathy. • The mechanism- is not completely resolved, but there is evidence for involvement of both the polyol pathway and the nonenzymatic glycation of proteins. • Site: Peripheral nerves , brain, and spinal cord. • morphologic features- most common (a) Relative loss of small myelinated fibers and of unmyelinated fibers, large fibers are also affected.(Diffuse or segmental) (b) Endoneurial arterioles show thickening, hyalinization, and intense periodic acid–Schiff positivity in their walls and extensive reduplication of the basement membrane THE END