Skeletal muscular disease- dystrophy
advertisement

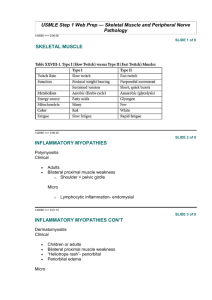
Pneumonia Skeletal muscle diseases 1 Pneumonia Skeletal muscle diseases a. Discuss the muscular dystrophies. - Describe their pathogenesis. - Describe their morphology. - Discuss their clinical picture and management. b. Discuss the disease of neuromuscular junctions. - Describe their pathogenesis. - Discuss their morphology. - Discuss the clinical picture and management. Reference: Robbins Basic Pathology, 8th edition (pages 827 – 830). 2 Pneumonia Diseases of Muscles Myopathies: disorders of muscle fibres Dystrophy: a genetic myopathy. Neurogenic: interference with nerve supply. Bilateral & symmetrical: myopathy Asymmetric: neurogenic. Diagnosis: - Clinical. – Muscle biopsy. - Nerve conduction. 3 a. Discuss the muscular dystrophies. Definition Muscular dystrophy is a heterogeneous group of inherited disorders recognized by progressive degenerative muscle weakness and loss of muscle tissue (started in childhood). Affect muscles strength and action. Generalized or localized. Skeletal muscle and other organs may involve Limitation: Difficulties with walking or Maintaining posture, Muscle spasms. Neurological, Behavioral, Cardiac, or other Functional limitations. a. Discuss the muscular dystrophies. Definition Muscular dystrophy Causes Inheritance Dominant genes Recessive gene Depends on the age when symptoms appear, and the types of symptoms that develop. Risk Because these are inherited disorders, risk include a family history of muscular dystrophy How Many People Are Affected It is estimated that between 50,000 -250,000 are affected annually. 1 per 3500 live male births Who Discovered Muscular Dystrophy Each neuromuscular disease (muscular dystrophy) was discovered by different person. 43 Types of Neuromuscular Diseases e.g: 1- X-Linked Muscular Dystrophy (Duchenne Muscular Dystrophy- DMS) 2- Becker Muscular Dystrophy- BMS 3- Myotonic Dystrophy. 2- Other Muscular Dystrophies: Less common, share many features with DMS, BMS, affect certain muscle groups (Fascioscapulohumeral muscular dystrophy; autosomal dominant\Oculopharyngeal muscular dystrophy; autosomal dominant, Congenital muscular dystrophies; autosomal recessive etc..). Muscular dystrophies- Pathogenesis DMS& BMS: 1- Caused by abnormalities in DMD, a gene that is located in the Xp21 region It encodes a 427-kD protein named dystrophin. 2- The genetic abnormalities are deletions with point mutations accounting for the rest. Approximately two thirds of the cases are familial, and the remainder represent new mutations. Dystrophin is a cytoplasmic protein located adjacent to the sarcolemmal membrane in myocytes, it concentrated at the plasma membrane over Z-bands, where it forms a strong mechanical link to cytoplasmic actin. dystrophin and the dystrophin-associated protein complex form an interface between the intracellular contractile apparatus and the extracellular connective tissue matrix transferring the force of contraction to connective tissue. The absence of dystrophin myocyte degeneration Myotonic Dystrophy 1- Inherited as an autosomal dominant trait a\w a CTG trinucleotide repeat expansion on chromosome 19q13.2–q13.3affect the mRNA for the dystrophia myotonia protein kinase (DMPK) sustained involuntary contraction of a group of muscles & stiffness. a. Discuss the muscular dystrophies. Morphology- DMS, BMS 1) Variation in fiber size (diameter) (2) Increased numbers of internalized nuclei (beyond the normal range of 3% to 5%). (3) Degeneration, necrosis, and phagocytosis of muscle fibers. (4) Regeneration of muscle fibers. (5) Proliferation of endomysial connective tissue. (6) Mytonic dystrophy-MS: (1-5)+ the ring fiber, with a subsarcolemmal band of cytoplasm that appears distinct from the center of the fiber (+\-) irregular mass of sarcoplasm (sarcoplasmic mass)+ relative atrophy of type 1 fibers (IHC) in advanced cases muscle fibers undergo degeneration and are replaced by fibrofatty tissue and collagen. In some types od MS , heart muscle and other involuntary muscle and other organs are affected. NORMAL DYS-1 test NEGATIVE DYS-1 test Mytonic dystrophy Fiber size variation- Internal nuclei in some fibers- Pyknotic nuclear clumps Esterase NADH stain a. Discuss the muscular dystrophies. Clinical features a. Discuss the muscular dystrophies. Clinical features Muscular Dystrophy- clinical features Type Onset Age (years) Clinical Features Other organ systems involved Duchenne Before 5 1.Progressive weakness of girdle muscles. 2.unable to walk after age 12 3.progressive kyphoscoliosis 4.Respiratory failure in 2dor 3d decade. Cardiomyopathy Mental impairment Becker 5-25yr early childhood to adult 1.Progressive weakness of girdle muscles 2. able to walk after age 15. 1.3. respiratory failure may develop by 4th grade Cardiomyopathy Emery-Dreifuss Childhood to adult Elbow contractures, humeral and perineal weakness Cardiomyopathy Limb-Girdle early childhood to adult Slow progressive weakness of shoulder and hip girdle muscles Cardiomyopathy Muscular dystrophy – clinical features Type Onset Age (years) Clinical Features Other organ systems involved Congenital At birth or within 1st few months .Hypotonia, contractures, delayed milestones Progression to respiratory failure in some; CNS and Eye abnormalities Facioscapulohumer al Before age 20 Slowly progressive weakness of face, shoulder girdle, and foot dorsiflexion Deafness Coat’s (eye) disease Oculopharyngeal 5th to 6th decade Slowly progressive weakness of extraocular, pharyngeal, and limb muscles ______ Myotonic Usually 2nd decade May be infancy if mother affected Slowly progressive weakness of face, shoulder girdle, and foot dorsiflexion Cardiac conduction defects Mental impairment Cataracts Frontal baldness Gonadal atrophy • Ultrasonography- high frequency sound waves. • Muscle biopsy- histopathology with application of others specific test, dystrophin and other special test. In the affected families females are carriers; clinically asymptomatic but often have elevated serum CK and show minimal histologic abnormalities on muscle biopsy. • Genetic “blood” test- looking for the portion of dystrophic gene e.g. Duchenne , Becker’s MS 1- Duchenne MD- Corticosteroid- prednisolone (improve muscle strength and delay progression) 2- Mytonic MD- Phenytoin, Carbamazepine, quinine (treat delayed muscle relaxation) b. Discuss the disease of neuromuscular junctions. Definition Myasthenia Gravis - MG is a muscle disease caused by immune-mediated loss of acetylcholine receptor. Prevalence: of about 30 in 100,000 persons. Age: < 40 yrs of life. Sex: commonly affect female> male, in older equally. Evidence based nearly all cases: decrease in the number of muscle acetylcholine receptors (AChRs), and circulating antibodies to the AChR are present in nearly all cases. Risk- thymic abnormalities are common in these patients b. Discuss the disease of neuromuscular junctions. PATHOGENESIS Autoimmune basis: Autoantibodies against the AChR lead to loss of functional AChRs at the neuromuscular junction by: (1) Fixing complement and causing direct injury to the postsynaptic membrane. (2) Increasing the internalization and degradation of the receptors. (3) Inhibiting binding of acetylcholine. Outcomes: A) Electrophysiologic studies are notable for diminished. B) Sensory as well as autonomic functions are not affected. b. Discuss the disease of neuromuscular junctions. Morphology 1- Muscle biopsy- (light microscopic): a) Specimens are usually unrevealing. b) In severe cases type 2 fiber atrophy due to disuse may be found. 2- Electron microscopy: a) The postsynaptic membrane is simplified, and there is loss of AChRs from the region of the synapse. b) Immune complexes and the complement membrane attack complex (C5–C9) can be found along the postsynaptic membrane as well. 3- administration of anticholinesterase agents- Test b. Discuss the disease of neuromuscular junctions. Clinical features 1- Weakness begins with the extraocular muscles; drooping eyelids (ptosis) and double vision (diplopia). 2- Generalized weakness- the weakness fluctuates over days, hours, or even minutes. 3- Intercurrent medical conditions can lead to exacerbations. 4- Respiratory compromise (major cause of mortality) b. Discuss the disease of neuromuscular junctions. Management 1- Better ventilatory support. 2- Anticholinesterase drugs. 3- Steroid- prednisone. 4- Plasmapheresis. 5- Thymectomy when thymic lesions are present.