KEHHonorsThesisFinal
advertisement

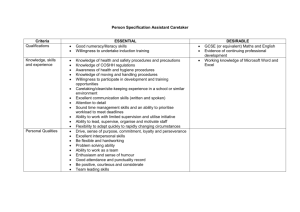
Running head: CARETAKING AND STRESS REACTIVITY Caretaking Behaviors and Stress Reactivity in Adolescents of Depressed Parents Kelsey Hudson Vanderbilt University CARETAKING AND STRESS REACTIVITY 2 Abstract This study was designed to explore the correlates of stress reactivity and caretaking behaviors in an at-risk sample of children living with a parent who has experienced at least one episode of major depressive disorder during the lifetime of their child. Specifically, the mechanisms of stress responses “fight or flight” and “tend and befriend” were used to define the stress response to parental depression. In a sample of 180 families of parents with a history of major depressive disorder, observed and reported caretaking behaviors and levels of stress-reactivity were examined. The association of children’s emotional and instrumental caretaking behaviors with levels of physiological and emotional stress response will be identified. Keywords: caretaking, stress reactivity, child depressive symptoms CARETAKING AND STRESS REACTIVITY 3 Introduction Parental depression is associated with significantly increased risk for behavioral and emotional problems in children and adolescents (Cummings & Davies, 1994; Goodman, 2007). The lifetime prevalence of major depressive disorder (MDD) is approximately 16% in the U.S., with young adulthood marking a period of increased prevalence of the disorder (Kessler et al., 2003). This means that a significant number of children will grow up in homes with parents who suffer from MDD. Because depression is such a prevalent mental health problem in our country today and because offspring of depressed parents have a dramatically increased risk of becoming depressed and experiencing other mental health problems, it is important to understand the processes that place these children at risk and that may protect some children from these risks. One mechanism of risk involves disruptions in parenting. Depressed parents are more likely than non-depressed parents to engage in negative parenting (e.g., Champion et al., 2009), which includes withdrawn, distancing, or intrusive behaviors. Withdrawn and distancing behaviors “reflect the degree to which the parent is uncaring, apathetic, uninvolved, ignoring, aloof, unresponsive, self-focused, and/or adult-oriented” (Melby & Conger, 2001). Examples of withdrawn/distancing behaviors include missing opportunities to respond to the child’s comment, sitting passively while the child engages in any particular behavior, or saying to the child, “I have too many things to do to be concerned with your problems.” Withdrawn behaviors physically and/or psychologically distance the parent from the child. Intrusive behaviors are defined as “intrusive and overcontrolling behaviors that are parent-centered rather than child-centered” (Melby & Conger, 2001). Examples of intrusive behavior include interrupting, telling the child how CARETAKING AND STRESS REACTIVITY 4 to solve a problem or task, or giving a continuous barrage of questions or directions without giving the child the chance to initiate any behavior on his/her own. Parents with current or past depression display high rates of both withdrawn and intrusive behaviors in their interactions with their children, and these parenting behaviors are associated with increased risk of internalizing and externalizing problems in children (e.g., Jaser et al., 2005). The negative parenting behaviors associated with parental depression are a source of significant chronic stress for a child or adolescent. Children of depressed parents need resources and skills to cope with and manage their stress so that they can develop sufficient coping and regulation skills that are needed throughout adulthood. Coping “describes how people mobilize, modulate, manage, and coordinate their behavior, emotion, and attention (or fail to do so) under stress” (Skinner & Zimmer-Gembeck, 2009). The child may cope with stress using primary control engagement coping (problem solving, expression of emotion), secondary control engagement coping (acceptance, positive thinking), or disengagement coping (avoidance, denial) (ConnorSmith et al., 2000). Secondary control coping is best suited to deal with uncontrollable sources of stress, including the stressors faced by children of depressed parents (e.g., Jaser et al., 2005). Multiple studies have shown primary and secondary control coping to be more effective ways of managing stress than disengagement coping (e.g., Weisz & Thurber, 1997). In a randomized clinical trial with 111 families of parents with a history of major depressive disorder, Compas and colleagues provided the first evidence that changes in secondary control coping and positive parenting can mediate the effects of a family group CARETAKING AND STRESS REACTIVITY 5 cognitive-behavioral preventive intervention on depressive, internalizing, and externalizing symptoms in adolescents; such changes accounted for approximately half of the effect of the intervention on the outcomes (Compas et al., 2010). Secondary control coping skills are particularly important to teach children and adolescents with depressed parents since they cannot control their parent’s depression. Depressed parents’ symptoms are reflected in their interactions with their children. In a study examining maternal stress and adolescent stress in response to mothers with and without a history of depression, Jaser and colleagues (2008) found that mothers with a history of depression exhibited greater levels of sadness during interactions with their children than mothers without a history of depression; likewise, the adolescent children of these mothers experienced higher rates of internalizing and externalizing symptoms than children of mothers without a history of depression. They found that secondary control coping mediated the effect of parental sadness on children’s adjustment, in that higher levels of secondary control coping were related to fewer child depressive symptoms (Jaser et al., 2008). The stressors associated with having a depressed parent may elicit certain stress responses from children. One way that children may respond to their parent’s depression is by trying to care for or tend to their parent. A child’s caretaking behaviors involve somewhat of a role reversal, as the child may take on some age-inappropriate parental roles. Two ways that a child may try to attend to a depressed mother’s needs (or withdrawn or distanced behaviors) include caring for her either emotionally or instrumentally (Champion et al., 2009; Cummings & Davies, 1995; Radke-Yarrow et al., 1994). Emotional caretaking is defined as a child’s awareness of parents’ personal and CARETAKING AND STRESS REACTIVITY 6 emotional problems. The child may suggest solutions, act as a referee in conflicts involving their parent, or even take responsibility for their parent’s problems. Instrumental caretaking includes taking on adult roles in the family, such as ageinappropriate behaviors like caring for younger children, helping to pay bills, or taking care of multiple chores. This type of caretaking can also be displayed during interactions with a parent if the child directs the focus of the interaction. At a broader level, two models of biobehavioral responses to stressful situations outlined by Taylor and colleagues (2000) can be used to understand children’s responses to the stress of living with a depressed parent. Their research suggests that females exhibit a different type of stress response than males. While the “fight or flight” model has traditionally been used to represent the stress response for both genders, the “tend and befriend” model may be more accurate in describing women’s response. “Fight or flight” is characterized as the activation of the sympathetic nervous system, which then innervates the adrenal medulla and eventually results in the secretion of catecholamines norepinephrine and epinephrine into the bloodstream. This response is a survival mechanism to prepare for an active response to threat (Taylor et al., 2000). In contrast, “tend and befriend” is characterized as a pattern of behavior that involves caring for offspring (tending) and creating social resources and networks to further facilitate care (befriending). Children may experience physiological responses to the stress of having a depressed mother. Research on fight or flight has shown that the basic acute stress response does not differ between gender (e.g., Jezova, Skultetyova, Tokarev, Bakos, & Vigas, 1995), but that the protective measures immediately following the release of stress CARETAKING AND STRESS REACTIVITY 7 hormones may be different for women than men (Taylor et al., 2000). Fleeing and/or fighting in response to stress may be more adaptive for males, as a female’s stress response may be more oriented towards protecting offspring. Studies have shown that the male hormone testosterone has been linked to hostility and aggressive behavior (e.g., Brismar, 1994; Olweus, Mattson, Schalling, & Low, 1980; Archer, 1990) and to rough play (Collaer & Hines, 1995), providing evidence that fighting or fleeing in the face of a threat may be especially adaptive for males. Contrarily, females may experience a different physiological response to stress (“Tend-and-Befriend), specifically marked by displaying nurturing activities that promote safety and protect the self by creating and maintaining social networks (Taylor et al., 2000). These two stress responses are important to examine in the context of maternal depression, as having a depressed mother is a source of chronic stress. Previous Findings Parenting behaviors from a depressed mother may elicit certain caretaking behaviors in children. Radke-Yarrow and colleagues (1994) found that children may try to take care of the mother by tending to her needs, but that gender accounted for the caretaking behaviors displayed. These researchers wanted to examine gender, affect, impulse control problems, and the mother-child attachment relationship. They observed clinically depressed and well mothers with their children (aged 24-48 months of age) over a 3-day span in a naturalistic setting. Their complex findings suggested that there are gender differences in caring behaviors of children of depressed mothers. Girls exhibited more caring behaviors towards the mother, while boys exhibited caretaking behaviors only when the mother was severely depressed. CARETAKING AND STRESS REACTIVITY 8 Cummings and Davies (1994) compiled a review of many findings concerning maternal depression and child development, finding that children may take on roles usually identified with parents, whether emotional or instrumental, and that the caretaking behaviors may be negative or positive. Since heavy amounts of ageinappropriate caretaking behaviors may hinder a child’s natural development of identity and independence, these behaviors are important to study. Champion and colleagues (2009) examined caretaking behaviors as predictors of adjustment in adolescents. As part of a preventive intervention, they brought depressed mothers and children into the lab and videotaped them as they talked for 15 minutes about a pleasant and a stressful task, respectively. They measured caretaking behaviors using parent reports, self-reports, questionnaires, and observed behavior. Their findings indicate that caretaking behaviors were related to anxiety and depression in adolescents with depressed mothers. Specifically, they found that in adolescents with depressed mothers, only emotional caretaking behaviors were related to their anxious-depressive symptoms and social competence. Limitations of Previous Research Limitations in this area of study are found in the lack of research concerning caretaking roles in the specific context of maternal depression. Considerable research has focused on other stressful situations, but not the stress associated with parental depression. Many studies have examined similar behaviors but for abuse, divorce, or life events that cause chronic stress (Champion et al., 2009). In addition, more research is needed to understand the associations between caretaking behaviors and characteristics of depression. CARETAKING AND STRESS REACTIVITY 9 Other limitations include the measures of caretaking behaviors. Caretaking has most often been measured using self-reports. Reports by the parent and child, while still an accepted method of measuring caretaking behavior, could be augmented with more information by measuring additional aspects of caretaking, like level of reciprocity and duration using direct observations of children’s interactions with their parents (Jurkovic, 1999). Observed behavior is one of the measures included in the current study, and is an important measure because there may be differences in reported behaviors versus observed behaviors. When trained coders with no previous knowledge of a family watches the interaction tasks and rates the child on his/her caretaking behaviors, a potentially less biased perspective is added to the measurement of caretaking. One specific problem in current research lies in defining “caretaking behaviors.” Defining caretaking brings up an important issue because it causes for a lack of consistency in the literature. Some researchers label the behaviors as “parentification” (Jurkovic, 1999). This label is focused on the child taking on adult-specific tasks. Some researchers label the behaviors as instrumental and emotional caretaking, but from a report-based perspective. In our research, we describe emotional caretaking and instrumental caretaking in terms of observed behavior and reported measures. Current Study Given the importance of understanding the potential costs and benefits of caretaking behaviors, particularly within the context of prevention programs, this study was designed to examine the association of children’s emotional and instrumental caretaking behaviors with levels of physiological and emotional stress. I hypothesize that there are differences in caretaking behaviors when gender is a factor. Further, I expect CARETAKING AND STRESS REACTIVITY 10 that the female stress response will be marked by more self-reported and observed caretaking behaviors (following the Tend-And-Befriend model) and that male stress response will be marked by more physiological responses to stress. Finally, I expect caretaking to be associated with adolescent depressive symptoms. Method Participants The sample consisted of 180 children (ages 9-15-years) and their parents. All parents had experienced at least one episode of major depressive disorder (MDD) during the lifetime of their child, with 132 in a current episode of depression. One hundred sixty of the parents were mothers and 20 were fathers, with a mean age 41.9 years. Eighty-two percent of the parents were Euro-American, 11.2% were African American, 1.1% were Asian American, 2.2% Hispanic American, 0.6% were American Indian or Alaska Native, and 2.2 % mixed ethnicity. The annual household income for the families ranged from below $5,000 to over $180,000, with mean annual income between $40,000 and $60,000. Education levels for the parents ranged from less than high school to completion of a graduate program: 5.6% of the parents had not completed high school, 8.9% had a high school education, 30.6% had received a degree from a technical school or had completed at least one year of college, 31.7% had received a degree from a 4 year college, and 23.3% had completed graduate education. Sixty-two percent of parents were married, 21.7% were divorced, 5% were separated, 10.6% had never married, and 1.1% was widowed. Children in the sample included 91 boys (mean age =11.2) and 89 girls (mean age = 11.8 years). Seventy-four percent of children were Euro-American, 12.8% were CARETAKING AND STRESS REACTIVITY 11 African American, 3.3% were Asian American, 1.7% was Hispanic American, 0.6% was American Indian or Alaska Native, and 7.2 % were mixed ethnicity. In order to determine the children who might be at risk for depression, children were screened and excluded from the study if they met criteria for current major depressive disorder. In families with more than one child in the targeted age range, one child was randomly selected for inclusion in the analyses to avoid possible problems of non-independence of children within the same family. Measures Adolescents’ depressive symptoms. The Child Behavior Checklist (CBCL), the Youth Self-Report (YSR), and the Center for Epidemiologic Studies of Depression (CES-D) were used to assess children’s depressive symptoms. The CBCL was used to assess symptoms of anxiety/depression (as a measure of general emotional distress) and total internalizing and externalizing problems in children and adolescents. The CBCL includes a 118-item checklist of problem behaviors that parents rate as 0 (not true), 1 (somewhat or sometimes true), or 2 (very true or often true) of their child in the past 6 months. The CES-D is a self-report measure of the frequency of 20 depressive symptoms over the past week using a 4-point Likert scale. The use of self- report scales such as the CES-D as a measure of depressive symptoms has been successfully validated with both adults (Dohrenwend & Shrout, 1984) and adolescents (Fendrich et al., 1990; Lewinsohn et al., 1991). The CES-D is short and easy to read, has been successfully administered in several large school samples (Lewinsohn et al., 1991; Schoenbach et al., 1982), and has good psychometrics with youth (Roberts et al., 1990). CARETAKING AND STRESS REACTIVITY 12 Adolescents completed the Youth Self Report (YSR, Achenbach, 1991) to provide their own perceptions of their functioning. Items on this scale include the child’s involvement in organizations and teams, number and frequency of contact with friends, and a rating of how well the child is able to get along with others relative to peers. Reliability and validity of the CBCL, YSR, and CES-D are well established (Achenbach & Rescorla, 2001; Fendrich et al., 1990; Lewinsohn et al., 1991). The Affective Problems scales from the CBCL and YSR were used in the current analyses as an index of children’s depressive symptoms (items include lack of enjoyment, sleep disruption, appetite disturbance, sadness, suicidal ideation, underactivity, feelings of worthlessness). The discriminant validity of the Affective Problems scales in predicting diagnoses of depression has been established (Ferdinand, 2008; van Lang et al., 2005). Internal consistency for the scales used in this study were = .84 for the CBCL, =.90 for the YSR, and = .88 for the CES-D. All children in the sample completed the YSR to allow for complete data on all measures. The internal consistency for the YSR Affective Problems scale was adequate with the younger 9-10- year-old group in the current sample ( = .80). Raw scores on the CBCL and YSR scores were used in all analyses to maximize variance (i.e., some variability is lost when the raw scores are converted to T-scores). A composite measure of adolescents’ affective symptoms was created by converting scores from adolescent and parent reports to z-scores and calculating the mean z-score for each participant ( = .80). Children’s stress reactivity. The parental depression version of the Responses to Stress Questionnaire (RSQ; Connor-Smith et al., 2000; Jaser et al., 2005, 2008) was used CARETAKING AND STRESS REACTIVITY 13 to assess levels of adolescents’ stress reactivity in response to stressors related to their parents’ depression (e.g., My mom/dad seems to be sad or cries a lot of the time; My mom/dad does not want to do things with the family; My mom/dad is too upset, tense, grouchy, angry, and easily frustrated). Items from the involuntary engagement/stress reactivity factor were used in the present study to assess stress reactivity involved in the Fight-or-Flight model (Connor-Smith et al., 2000). Items on this factor reflect physiological reactivity (e.g., increased heart rate), emotional reactivity (e.g., becoming upset by previously non-threatening events), and intrusive or uncontrollable thoughts (e.g., inability to stop thinking about a problem when attempting to sleep). Adolescents and their parents were asked separately to rate each item with regard to the degree/frequency with which the adolescent responded to the identified stressors. To control for response bias and individual differences in base rates of item endorsement, proportion scores were calculated by dividing the score for each factor by the total score for the RSQ (Vitaliano, Maiuro, Russo, & Becker, 1987). Internal consistency for the involuntary engagement/stress reactivity factor was = .75 for parents and = .82 for adolescents. Adolescents’ caretaking behaviors. Three measures were used to assess caretaking behaviors by adolescents directed toward their depressed parent: direct observations of children and their parents, composite parent and child reports of child caretaking behaviors on the RSQ, and children’s reports of their caretaking on the Parentification Questionnaire for Youth (PQ-Y; Godsall & Jurkovic, 1995). Observations of caretaking. First, the emotional and instrumental caretaking codes adapted from the Iowa Family Interaction Ratings scales (IFIRS) were used to code CARETAKING AND STRESS REACTIVITY 14 videotaped interactions between each child and his or her parent (Melby & Conger, 2001). Parents and children participated in two 15-minute interactions, first about a pleasant activity that the parent and child enjoyed doing together in the past couple of months (i.e., Task 1, positive task), and second about a recent stressful time when the parent was depressed, down, or grouchy, making it difficult for the family (i.e., Task 2, stressful task). The sequence of the discussion of the positive topic followed by the discussion of the stressful topic was used to allow for analyses of changes in children’s emotions in response to a stressor. The IFIRS is a global coding system comprised of codes that reflect content of conversation, emotional affect, and non-verbal behavior to determine scoring (Melby & Conger, 2001). There are multiple codes in the system, but the two of interest for this study are labeled in the IFIRS as Instrumental caretaking and Emotional caretaking. Instrumental caretaking includes the extent to which the child takes care of the parent or takes on tasks or responsibilities that may be typically considered parental roles. The emotional caretaking code includes the extent to which the child takes care of the emotional needs of the parent or takes on an emotional burden that may be ageinappropriate. All codes have a 9-point scale, 1 representing “not at all characteristic” and 9 representing “mainly characteristic.” Coders focus on frequency and intensity of the behaviors and verbal statements to assign each participant a score on all codes. Each 15-minute parent-child interaction was coded by two independent raters (doctoral students in clinical psychology and advanced undergraduate research assistants). Coders completed extensive training to learn the codes in the IFIRS system and to become reliable with other coders. After coding each CARETAKING AND STRESS REACTIVITY 15 parent-child interaction, the two coders then met to assign consensus codes for any codes that differed by two or more points on the 1 to 9 scale. They attained a consensus score for each discrepant code by discussing the examples they noted for each code and referring to the coding manual to verify their examples. Training for coding the interactions consisted of approximately 35 hours of instruction and practice, including reading and studying the manual, taking a written test on the content, coding specific interactions to test for reliability, and meeting weekly with a team of experienced coders. Once a newly trained coder achieved agreement with 80% of codes on an interaction with scores previously established by trained coders, he or she was considered prepared to code independently and able to complete consensus on interactions with other coders. All coders attended weekly meetings throughout the study, during which coders could discuss recently coded interactions and clarify questions in order to prevent drift between coders. For the present study, consensus codes were used for all testing; however, the original scores for each rater were used to determine inter-rater reliability. Ratings showed adequate inter-rater reliability (73% inter-rater agreement). Child and parent reports of caretaking: RSQ. Items 61-64 from the parental depression version of the Responses to Stress Questionnaire (RSQ; Connor-Smith et al., 2000; Jaser et al., 2005, 2008) were used to assess levels of adolescents’ caretaking in response to stressors related to their parents’ depression (e.g., I try to be on my best behavior so mom/dad won’t get upset; I try to be helpful with things around the house; I cheer my mom/dad up to make him/her feel better; I try to get my parents to stop arguing). A composite score was created for caretaking by converting parent and child reports to standardized scores (z-scores). CARETAKING AND STRESS REACTIVITY 16 Children’s reports of caretaking: PQ-Y. The Parentification Questionnaire-Youth (PQ-Y; Godsall & Jurkovic, 1995) is an adaptation of the Parentification Questionnaire (PQ; Sessions & Jurkovic, 1986) modified for children and adolescents and written at a 3rd grade reading level. This measure is a 20-item, yes-no self-report questionnaire that assesses the subjective experience of caretaking responsibility between children and their families. The items include both emotional caretaking (e.g., “I often feel like a referee in my family,” “I feel I’m asked too often to take care of some other family member”) as well as instrumental caretaking (e.g., “I often have to do other family members' chores,” “I have to help a lot with the family bills”). Internal consistency reliability of this measure is adequate (α = .75-.83) and in the current sample was also found to be adequate (α = .80). Procedure After expressing an interest in the study, each parent completed an initial phone interview to determine initial eligibility for the baseline assessment of the prevention study. If the parent was determined eligible from the phone interview, the family then participated in various baseline assessments in the laboratory to assess psychological history and ultimately determine eligibility for randomization into the intervention trial. These assessments included clinical interviews with the parent and child, questionnaires completed by parents and children, and two 15-minute-long video taped parent-child interactions between the parent and the child. Before beginning the diagnostic interviews, the parent and child completed a form to identify something pleasant they had recently done together and something stressful and difficult for the family that had occurred the last time the parent was sad, down, CARETAKING AND STRESS REACTIVITY 17 and/or irritable. The parents and children were informed that these topics would later be used for the videotaped discussions. Upon completion of the diagnostic interviews, the parent and child participated in the two video taped discussions. The positive task (i.e., the pleasant activity) was administered first. A cue card was provided with questions to guide the discussion. The interviewer filled in the cue cards using the form the parent and child completed before the interviews. Questions for the first task included: “What happened when we ___?”, “How did we feel when we ___?”, “What are some other fun activities would we like to do together?”, “What prevents us from doing fun activities together?”. After 15 minutes, the interviewer entered the room to exchange the cue cards and to tell the parent and child to switch to the stressful topic for the second 15-minute interaction (i.e., discussing stress related to the parent’s depression). The cue card for the second task contained the following questions: “What happened the last time___?”, “What kinds of feelings or emotions do we usually have when mom/dad is sad, down, irritable, or grouchy?”, “What do we do to reduce the stress when mom/dad is sad, down, irritable or grouchy?”. After 15 minutes, the interviewer turned off the camera and conducted a short debriefing with the parent and child to ask how the interactions went and to answer any questions. Families were screened to determine eligibility, primarily to discern that at least one parent in the family had experienced at least one major depressive episode or dysthymia during the child’s lifetime. If two parents met criteria for depression or dysthymia, the parent who initially contacted the study was designated as the target parent. The following parental diagnoses or characteristics were excluded from the CARETAKING AND STRESS REACTIVITY 18 sample: bipolar I, schizophrenia, or schizoaffective disorder. Child diagnoses that led to exclusion from the study included mental retardation, pervasive developmental disorders, alcohol or substance use disorders, current conduct disorder, bipolar I disorder, and schizophrenia or schizoaffective disorder. Additionally, if a child in the family met criteria for current depression or was acutely suicidal, the family was placed on hold, and a re-assessment procedure was applied. The Institutional Review Boards at the two participating university research sites approved all procedures in the study. Doctoral students in clinical psychology completed extensive training for the structured clinical interviews and conducted all interviews in psychology laboratories at the two universities. All participants provided informed consent prior to participation in the study, and each participant received $40 compensation for their participation in the baseline assessment. Data Analyses Through prior research and empirical literature on caretaking, potential correlates of caretaking behaviors (e.g. stress reactivity and depressive symptoms) were identified. Correlations were run with 3 measures of caretaking to examine relationships to stress reactivity and depressive symptoms in adolescents. Independent and paired sample ttests were conducted to compare means and standard deviations. Results Gender Comparisons Independent sample t-tests were used to compare means and standard deviations for measures of children’s stress reactivity, caretaking behaviors, and depressive symptoms. Results are presented separately for boys and girls in Table 1. Boys and girls CARETAKING AND STRESS REACTIVITY 19 were significantly different on the self-reported RSQ Involuntary Engagement scale, with girls (M = .23) reporting higher levels than boys (M = .22), t = -2.75, p = .01. Additionally, girls’ (M = 3.10) levels of Instrumental caretaking during Task 1 were higher than boys (M = 2.75), approaching significance (t = -1.71, p = .09). It is noteworthy that there were no significant gender differences on any of the caretaking measures: Emotional caretaking Task 1 (MBoys= 2.42, MGirls= 2.47, t = .20, p = .84), Instrumental caretaking Task 1, Emotional caretaking Task 2 (MBoys= 3.83, MGirls= 3.85, t = -.08, p = .94), Instrumental caretaking Task 2, (MBoys= 3.21, MGirls= 3.37, t = -.60, p = .55); PQ-Y (MBoys= 5.75, MGirls= 6.32, t = -1.01, p = .31); RSQ (MBoys= -.04, MGirls= .04, t = -.59, p = .56). Further, there were no gender differences on parent reported Involuntary Engagement (MBoys= .24, MGirls= .25, t = -.78, p = .43) or Involuntary Disengagement (MBoys= .18, MGirls= .17, t = .84, p = .40). Child reported Involuntary Disengagement (MBoys= .17, MGirls= .17, t = .21, p = . 83) was also insignificant. Finally, no gender differences were found among measures of depressive symptoms, including child reported YSR Affective Problems (MBoys= 57.09, MGirls= 55.98, t = .99, p = .32), CES-D (MBoys= 13.78, MGirls= 14.36, t = -.36, p = .72), and parent-reported Affective Problems from the CBCL (MBoys= 59.93, MGirls= 60.94, t = -.83, p = .41). Overall, gender differences among caretaking, stress reactivity, and depressive symptoms were minimal. Correlational Analyses Measures of caretaking behaviors. Correlations among the three measures of children’s caretaking behaviors are presented in Table 2. Emotional Caretaking in Task 1 CARETAKING AND STRESS REACTIVITY 20 was significantly associated with Instrumental caretaking in Task 1 (r = .25, p < .01), Emotional caretaking in Task 2 (r = .27, p < .01), and Instrumental caretaking in Task 2 (r = .23, p < .01). Instrumental caretaking in Task 1 was not related to Emotional caretaking in Task 2 (r = .12, p = .12). However, Emotional and Instrumental caretaking in Task 2 showed a moderately strong correlation (r = .46, p < .01). The PQ-Y was not significantly correlated with Emotional caretaking in Task 1 (r = .01, p = .96) or Task 2 (r = -.09, p =.25), nor was it correlated with Instrumental caretaking in Task 1 (r = .10, p = .22) or Task 2 (r = .09, p = .25). Caretaking as reported by the RSQ was associated with Emotional caretaking in Task 1 (r = .20, p < .05) and Task 2 (r = .17, p < .05). RSQ caretaking was not significantly associated with Instrumental caretaking in Task 1 (r = .08, p = .33) or Task 2 (r = .12, p = .13). Additionally, RSQ caretaking was not significantly related to the PQ-Y (r = -.07, p = .34). The correlational analyses summarize that observed caretaking behaviors are related and seem to measure the same construct; in contrast, the lack of significant associations among observed behaviors and the PQ-Y provide evidence that the two measures are measuring different aspects of caretaking. Caretaking, stress reactivity and depressive symptoms. Correlations among measures of stress reactivity and caretaking are presented in Table 3. In observing the relationship between caretaking and stress reactivity, it is noteworthy that none of the observed caretaking were related to measures of stress reactivity. However, measures of stress reactivity were significantly related to child-reported parentification at a p < .01 level, showing that “parentification” and stress reactivity measure similar constructs. The PQ-Y was significantly associated with Involuntary Disengagement parent reports CARETAKING AND STRESS REACTIVITY 21 (r = .24, p < .01) and child self-reports (r = .34, p < .01), and with Involuntary Engagement child reports (r = .25, p < .01). In contrast, the PQ-Y was not associated with parent-reported Involuntary Engagement (r = .01, p = .93). Only child-reported Involuntary Disengagement was related to the RSQ composite caretaking scale, showing a negative association between child stress reactivity and combined child and parent reports of caretaking (r = -.16, p < .05). These intriguing findings show that children who report more levels of parentification as labeled on the PQ-Y also report higher levels of stress reactivity. To summarize, the correlations among children’s caretaking, stress reactivity, and depressive symptoms are presented in Table 4. Observed Emotional caretaking in Task 1 was not associated with YSR Affective Problems (r = 03, p = .74) or the CES-D (r = .08, p = .34) but was significantly associated with parent-reported Affective Problems on the CBCL (r = .19, p < .05). Emotional Caretaking in Task 2 was not associated with child reported Affective Problems (r = -.10, p = .21) or parent reported Affective Problems (r = .03, p = .71), but was found to be significantly and negatively associated with selfreported depressive symptoms on the CES-D (r = -.16, p < .05), indicating that children who engaged in Emotional caretaking during the negative tasked viewed themselves as having fewer symptoms of depression. Instrumental caretaking was not associated with depressive symptoms in either task. Interestingly, the PQ-Y was significantly associated with all 3 measures of depressive symptoms (YSR: r = 35, p < .01; CES-D: r = .44, p < .01; CBCL: r = .18, p < .05). Caretaking as measured by the RSQ was not associated with depressive symptoms. Measures of stress reactivity were significantly associated with child depressive symptoms. Child-reported Affective Problems from the YSR were CARETAKING AND STRESS REACTIVITY 22 significantly related to reports of Involuntary Engagement by parents (r = 23, p < .01) and children (r = .42, p < .01) and to Involuntary Disengagement by parents (r = .22, p < .01) and children (r = .39, p < .01), indicating that Affective Problems reported by children themselves are highly associated with both parent and child reports of stress reactivity. Depressive symptoms from the CES-D were associated with Involuntary Disengagement reported by parents (r = .18, p < .05) and children (r = .42, p < .01). The CES-D was also associated with child-reports of Involuntary Engagement (r = .49, p < .01), but not with parent reports of the same factor (r = .14, p = .07). Discussion This study was designed to extend past research on the costs and benefits of caretaking behaviors in children with depressed parents. Given that adolescents with depressed parents are at a higher risk for psychopathology, it is important to conduct additional research on the specific behaviors that may prevent this at-risk sample from developing depression. Previous studies have relied heavily on retrospective reports of caretaking behaviors. It is noteworthy that we were able to observe child and adolescent caretaking in a laboratory setting as well as by parent- and child-reports; using multiple measures of caretaking allows for a more broad assessment of the behaviors. Children in this sample did exhibit levels of caretaking behaviors (ranging from 2.4 to 3.8 on a 9 point scale) during the positive and negative task, as evidenced by the means presented in Table 1. In comparing gender differences among children, significant differences were found in means of self-reported Involuntary Engagement, showing girls (M = .23) to display higher levels than boys (M = .22). This finding provides interesting evidence that girls in CARETAKING AND STRESS REACTIVITY 23 this sample reported themselves as significantly experiencing more rumination, intrusive thoughts, emotional and physiological arousal, and involuntary action. Additionally, there is evidence to suggest that girls (M = 3.10) displayed higher levels of Instrumental caretaking in the first observation task (i.e., a discussion of positive topic|) than boys (M = 2.75), as the p-value approached significance (p = .09). Except for the previous two findings, gender differences in caretaking behaviors, stress reactivity, and depressive symptoms were minimal. This was somewhat unexpected, as some evidence has identified girls to be at a higher risk when living with a depressed parent (e.g., RadkeYarrow et al., 1994). Overall, results from the independent sample t-tests found minimal gender differences. The lack of significant gender differences in these at-risk children may be caused, in part, by the substantial amount of chronic stress experienced by members of a family with a depressed parent. Although findings on gender differences in children living with depressed parents are highly inconsistent, prior studies have also shown minimal gender differences in children and adolescents living with a depressed parent, suggesting that both genders may be equally affected due to the extreme familial stress. One hypothesis, the Equalization hypothesis, posits that sons and daughters have an equivalent number of symptoms or diagnoses of depression (Foster et al., 2008). Our results support this theory, showing both boys and girls to have elevated scores on stress reactivity and depressive symptoms with minimal differences (see Table 1). Although results found that caretaking behaviors were present in both observed and reported measures, the correlational analyses indicate that the different measures of caretaking may be assessing different constructs. Results showed that the observed in- CARETAKING AND STRESS REACTIVITY 24 task Emotional and Instrumental caretaking behaviors were significantly correlated with each other (r’s ranged from .23 to .46, Table 2), suggesting that the two types of caretaking behaviors are measuring a similar construct. As stated previously, these two measures are based on the intensity and frequency of behaviors in the interaction task, and may also include some behaviors at home. Additionally, the findings show that only Emotional Caretaking is moderately but significantly associated with depressive symptoms as reported by parents (CBCL) and children (CES-D), as shown in Table 4. This suggests that observed Emotional caretaking may be related to child depressive symptoms; however, these constructs are distinct and future research is needed to draw conclusions about their associations. Correlational analyses among all three caretaking measures (Table 2) also showed that the PQ-Y was not associated with observed caretaking on either task, suggesting that the two measures are capturing very distinct aspects of caretaking, or that they may not be assessing the same construct. The PQ-Y was also not associated with the RSQ caretaking measures. Many of the items on the PQ-Y are posed in a negative fashion (e.g., “I seem to get the blame for most of what happens in my family”) and may encourage generalizations about the child and adolescent behavior within the family. The Emotional and Instrumental caretaking codes as defined by the IFIRS scales specifically distinguish emotional from task-related caretaking behaviors, and rely on specific caretaking criteria that may be age-inappropriate (e.g., child suggests a solution to a mother’s marital problem) and less on generalized behavior in the home. The PQ-Y is a Yes or No questionnaire, which may influence a child to answer “yes” on a question even if the behavior occurs at a low or moderate level, whereas the Emotional and CARETAKING AND STRESS REACTIVITY 25 Instrumental caretaking codes are assessed on a 9 point scale, and can measure children’s caretaking at low, moderate, and high levels. Words such as “often”, “seem”, and “feel” are common among items on the PQ-Y, and may encourage a more broad and subjective perspective in a child reporting caretaking behaviors at home. These differences may account for the lack of significant association between the two measures. The composite score for child caretaking as measured by the RSQ was associated with Emotional Caretaking on both tasks, suggesting that the Emotional Caretaking code and the RSQ items measure similar aspects of caretaking (e.g. soothing a distressed parent or taking blame for a problem). Results from correlational analyses among depressive symptoms, caretaking, and stress reactivity (Table 4) confirm previous research and provide further evidence that stress reactivity is an important factor in understanding adolescent depressive symptoms. Observed caretaking was generally not associated with depressive symptoms, with two exceptions: Emotional caretaking Task 1 was moderately and positively associated with CBCL Affective Problems (r = .19), and Emotional Caretaking Task 2 was moderately and negatively associated with CES-D depressive symptoms (r = -.16). The CBCL assesses parents’ perception of their children’s social competence in the past 6 months, with Affective Problems being a subscale included in measuring overall social competence. The positive association between Affective Problems and Emotional caretaking when discussing a pleasant task is interesting and may suggest that depressed parents in our sample viewed their child’s caretaking in a non-stressful situation as problematic. Previous research has shown depressed parents to display more withdrawn and intrusive CARETAKING AND STRESS REACTIVITY 26 behaviors when interacting with their children (i.e. Radke-Yarrow et al., 1994; Jaser et al., 2007). The association found between parents’ report of child Affective Problems and caretaking behaviors in a pleasant task may further this evidence, suggesting that the depressed parent may not view caretaking behaviors as appropriate unless they are being cared for during stressful interactions. The negative association found between Emotional caretaking Task 2 and the CES-D depressive symptoms (r = -.16) shows that children who exhibited Emotional caretaking while talking about a negative task also reported lower levels of depressive symptoms. This association may result from the child’s understanding of Emotional caretaking as an encouraged and/or accepted behavior- a viewpoint that may or may not be encouraged by the depressed parent. While this may be true, it is important to note that caring for others is a basic human tendency; not all caretaking behaviors are inappropriate. Previous studies have suggested that moderate levels of caretaking may be acceptable for child adjustment (i.e. Cummings and Davies, 1994), and the negative association between child-reported depressive symptoms and Emotional Caretaking during a negative interaction may support prior research (as the mean caretaking level during Task 2 was moderate- 3.8 for both boys and girls). Another important finding was the association of the PQ-Y with all three measures of depressive symptoms (r’s ranged from .18 to .44). This finding, in conjunction with the lack of association between observed caretaking, RSQ caretaking items, and depressive symptoms, is important in considering the different constructs of caretaking. The strong association among all three measures of depressive symptoms and the PQ-Y suggests that the PQ-Y may measure aspects of caretaking that are also involved in symptoms of depression. As previously stated, this may be the result of the CARETAKING AND STRESS REACTIVITY 27 wording of the PQ-Y, which has negative undertones. The more negative wording may appeal more to children who are already more inclined to negative thinking and functioning (and therefore higher on measures of depressive symptoms). More generally, the PQ-Y may simply be a more accurate assessment of the kinds of negative caretaking behaviors that we are interested in when trying to understand risky behaviors in at-risk adolescents. More research is needed to understand the precise caretaking behaviors or mindsets that are related to depressive symptoms. Results showing stress reactivity reported by both children and parents are presented in Table 3 and Table 4. Stress reactivity was mostly significantly associated with depressive symptoms (r’s ranged from .18 to .49, Table 4), supporting previous research; however; depressive symptoms from the CES-D were not related to parentreported Involuntary Engagement and CBCL affective problems were not related to child-reported Involuntary Disengagement. These insignificant findings may be caused by differences in child and parent perceptions. Specifically, parents reporting on their child’s rumination, intrusive thoughts, and arousal (Involuntary Engagement) may not have a clear knowledge of these problems unless they have specifically discussed those topics with their child. Similarly, the CBCL is a parent-reported questionnaire and may not show associations with child reports of involuntary disengagement (e.g., emotional numbing, cognitive interference) due to lack of discussion or a difference in perception. The Tend-And-Befriend model, which provides a complementary model to the well-known Fight-or-Flight model of stress, posits that humans may also have biobehavioral tendencies that focus on affiliative and nurturing processes (providing and receiving mutual protection) in the face of distress. The findings from this study support CARETAKING AND STRESS REACTIVITY 28 this model, providing evidence that adolescents exhibit caring behaviors in response to a chronic stressor. Hypotheses involving gender differences relating stress reactivity in this sample to the Taylor Tend-And-Befriend model were not supported. Specifically, males and females in the sample generally did not show marked differences in caretaking or stress reactivity. Both boys and girls in the current study reported exhibiting caretaking behaviors at home (RSQ: M = -.04 for boys, M = .04 for girls); PQ-Y: M= 5.75 for boys, M = 6.32 for girls) and during both the positive and negative tasks (M = 2.42 Task 1 and 2.75 Task 2 for boys; M= 2.47 Task 1 and 3.10 Task 2 for girls). Although there were no statistically significant gender differences, it is noteworthy that girls in the sample scored higher on Emotional and Instrumental Caretaking during both tasks, on the PQ-Y, and on the RSQ Caretaking scale than boys. More research on children with depressed parents is needed to comprehend potential gender differences that may be important considerations when conducting preventive interventions. There are noteworthy limitations to this study that should be addressed. First, only 20 fathers were included in the sample of depressed parents. Although gender differences in children were minimal in our study (and have been minimal in prior research on children of depressed parents), parent gender may be an important factor in researching child caretaking. Second, there is evidence to suggest discrepancies in current measures of caretaking behaviors. Although this study included observed and reported measures of caretaking, these measures may not be accurately assessing the same construct, as evidenced by the associations (and lack thereof) among the PQ-Y, RSQ Caretaking, and observed Emotional and Instrumental Caretaking. Specifically, there is not a standardized definition of “caretaking behavior” in current literature. CARETAKING AND STRESS REACTIVITY 29 Differences in defining caretaking may lead to the measurement of different constructs when researching these behaviors. Given the empirical evidence to date on child caretaking behaviors, future research should focus on standardizing definitions of caretaking so that specific aspects of the construct may be examined to determine potential consequences. Specifically, examining which aspects of caretaking are harmful to children’s adjustment will allow researchers to understand which behaviors and/or coping skills are most beneficial to teach these at-risk children when conducting preventive interventions. The findings from this study show that measures such as the PQ-Y may assess caretaking behaviors that are particularly important in understanding caretaking as it relates to depressive symptoms, whereas observed behavior may assess other aspects of caretaking. Understanding the specific aspects of caretaking that negatively affect child adjustment is imperative, since some degree of caretaking is not only typical but also expected in most families. Examining the costs and benefits of caretaking behaviors in children of depressed parents will direct researchers to more accurately develop preventive interventions for families suffering from the consequences of depression. CARETAKING AND STRESS REACTIVITY 30 References Allen, J. P., McElhaney, K. B., Kuperminc, G. P., & Jodl, K. M. (2004). Stability and change in attachment security across adolescence. Child Development, 75, 1792–1805. Anderson, C. A., & Hammen, C. L. (1993). Psychosocial outcomes of children of unipolar depressed, bipolar, medically ill, and normal women: a longitudinal study. Journal of Consulting and Clinical Psychology, 61, 448-454. Barnett, B., & Parker, G. (1998). The parentified child: Early competence or childhood deprivation? Child Psychology and Psychiatry Review, 3, 146 –155. Champion, J. E., Jaser, S. S., Reeslund, K. L., Simmons, L., & Potts, J. E. (2009). Caretaking behaviors by adolescent children of mothers with and without a history of depression. Journal of Family Psychology, 23, 156-166. Compas, B. E., & Champion, J. E. et al.(2010). Coping and Parenting: Mediators of 12Month Outcomes of a Family Group Cognitive–Behavioral Preventive Intervention With Families of Depressed Parents. Journal of Consulting and Clinical Psychology, 78, 623-634. Cummings, M. E., & Davies, P. T. (1994). Maternal depression and child development. Journal of Child Psychology and Psychiatry and Allied Disciplines, 35, 73–112. Foster, C.E., Webster, M.C., Weissman, M.M., Pilowsky, D.J., Wickramaratne, P.J., Rush, J.A., Hughes, C.W., et al. (2007). Course and severity of maternal depression: Association with family functioning and child adjustment. J. Youth Adolescence, 37: 906-916. CARETAKING AND STRESS REACTIVITY 31 Grant, K. E., & Compas, B. E. (1995). Stress and anxious-depressed symptoms among adolescents: Searching for mechanisms of risk. Journal of Consulting and Clinical Psychology, 63, 1015–1021. Herer, Y., & Mayseless, O. (2000). Emotional and social adjustment of adolescents who show role-reversal in the family. Megamot, 3, 413– 441. Jaser, S. S., Champion, J. E., Reeslund, K. L., Keller, G., Merchant, M. J., Benson, M., & Compas, B. E. (2007). Cross-situational coping with peer and family stressors in adolescent offspring of depressed parents. Journal of Adolescence, 30, 917-932. Jaser, S. S., Fear, J. M., Reeslund, K. L., Champion, J. E., Reising, M. M., & Compas, B. E. (2008). Maternal sadness and adolescents’ responses to stress in offspring of mothers with and without a history of depression. Journal of Clinical Child and Adolescent Psychology, 37, 736-746. Jezova, D. (1995). Vasopressin and oxytocin in stress. Annals of the New York Academy of Sciences, 771, 192-203. Jurkovic, G. J. (1997). Lost childhoods: The plights of the parentified child. Philadelphia: Brunner/Mazel. Kessler, R. C., & McLeod, J. D. (1984). Sex differences in vulnerability to undesirable life events. American Sociology Review, 49(5), 620-631. McMahon, T. J., & Luthar, S. S. (2007). Defining characteristics and potential consequences of caretaking burdens among children living in urban poverty. American Journal of Orthopsychiatry, 77(2), 267-281. Radke-Yarrow, M., Zahn-Waxler, C., Richardson, D. T., Susman, A., & Martinez, P. (1994). Caring behavior in children of clinically depressed and well mothers. CARETAKING AND STRESS REACTIVITY 32 Child Development, 65, 1405–1414. Skinner, E. A., & Zimmer-Gembeck, M. J. (2009). Challenges to the developmental study of coping. In E. A. Skinner & M. J. Zimmer-Gembeck (Eds.). Coping and the development of regulation. New Directions for Child and Adolescent Development, 124, pp. 5-17. San Fransisco: Jossey-Bass. Stein, J. A., Riedel, M., & Rotheram-Borus, M. J. (1999). Parentification and its impact on adolescent children of parents with AIDS. Family Process, 38, 193–207. Taylor, S. E. (2006). Tend and befriend: biobehavioral bases of affiliation under stress. Current Directions in Psychological Science, 15, 273-277. Taylor, S. E., Burklund L. J., Eisenberger, N. I., Lehman, B. J., Hilmert, C. J., & Lieberman, M. D. (2008). Neural bases of moderation of cortisol stress responses by psychosocial resources. Journal of Personality and Social Psychology, 95, 197-211. Weisz, J. R., Thurber, C. A., Sweeney, L., Proffitt, V. D., & LeGagnoux, G. L. (1997). Brief treatment of mild-to-moderate child depression using primary and secondary control enhancement training. Journal of Consulting and Clinical Psychology, 65, 703-707. CARETAKING AND STRESS REACTIVITY 33 Table 1. Means and standard deviations of gender differences in measures of child caretaking and stress reactivity. t-test 1. EC 1 2.42 t = -.20 n.s. p = .84 2. IC 1 2.75 1.38 3.10 1.38 t = -1.71 n.s. p = .09 3. EC 2 3.83 2.11 3.85 2.17 t = -.08 n.s. p = .94 4. IC 2 3.21 1.77 3.37 1.68 t = -.60 n.s. p = .55 5. PQ-Y 5.75 3.58 6.32 3.76 t = -1.01 n.s., p = .31 6. RSQ Caretaking -.04 .86 .04 .79 t = -.59 n.s. (Composite) p = .56 7. RSQ IE (Parent .24 .05 .25 .05 t = -.78 n.s. on Child) p = .43 8. RSQ ID (Parent .18 .03 .17 .03 t = .84 n.s. on Child) p = .40 9. RSQ IE (Child) .22 .03 .23 .04 t = -2.75 p = .01 10. RSQ ID .17 .03 .17 .03 t = .21 n.s. (Child) p = .83 11. YSR Affective 57.09 7.89 55.98 6.83 t = .99 n.s. Problems p = .32 12. CES-D 13.78 10.45 14.36 11.03 t = -.36 n.s. p = .72 13. CBCL 59.93 7.92 60.94 8.18 t = -.83 n.s. Affective Problems p = .41 Note. EC 1: Observed Emotional Caretaking-Task 1; IC 1: Observed Instrumental Caretaking-Task 1; EC 2: Observed Emotional Caretaking-Task 2; IC 2: Observed Instrumental Caretaking, Task 2. PQY: Parentification Questionnaire for Youth. RSQ: Responses to Stress Questionnaire. IE: Involuntary Engagement; ID: Involuntary Disengagement. YSR: Youth Self-Report. CES-D: The Center for Epidemiological Studies Depression Scale. CBCL: Child Behavior Checklist. n.s: Not Significant. M (Boys) SD (Boys) 1.35 M (Girls) 2.47 SD (Girls) 1.52 CARETAKING AND STRESS REACTIVITY Table 2. Correlation among measures of EC, IC (both tasks), PQ-Y Total, and RSQ Caretaking Scale (boys and girls). 1. 2. 3. 4. 5. 1. EC 1 2. IC 1 .25** 3. EC 2 .27** .12 n.s. 4. IC 2 .23** .27** .46** 5. PQ-Y .004 n.s. .10 n.s. -.09 n.s. .09 n.s. 6. Composite .20* .08 n.s. .17* .12 n.s, -.07 n.s. RSQ Caretaking *p < .05, ** p < .01 Note. EC 1: Observed Emotional Caretaking-Task 1; IC 1: Observed Instrumental Caretaking-Task 1; EC 2: Observed Emotional Caretaking-Task 2; IC 2: Observed Instrumental Caretaking, Task 2. PQ-Y: Parentification Questionnaire for Youth. RSQ: Responses to Stress Questionnaire. n. s.: Not significant. 34 CARETAKING AND STRESS REACTIVITY 35 Table 3. Correlations among measures of stress reactivity and caretaking. 1. RSQ IE (Parent on Child) 2. RSQ ID (Parent on Child) 3. RSQ IE (Child) 4. RSQ ID (Child) EC 1 IC 1 EC 2 IC 2 PQ-Y -.02 n.s. p = .76 -.07 n.s. p = .37 -.02 n.s. p = .80 -.13 n.s. p = .11 .02 n.s. p = .81 -.04 n.s. p = .60 .03 n.s. p = .67 -.07 n.s. p = .38 -.12 n.s. p = .14 -.05 n.s. p = .56 -.14 n.s. p = .08 -.05 n.s. p = .52 -.07 n.s. p = .40 -.02 n.s. p = .80 -.07 n.s. p = .37 .01 n.s. p = .90 .01 n.s. p = .93 .24** .25** .34** RSQ Composite Caretaking .10 n.s. p = .18 -.12 n.s. p = .11 -.01 n.s. p = .92 -.16* *p < .05, ** p < .01 Note. RSQ: Responses to Stress Questionnaire; IE: Involuntary Engagement; ID: Involuntary Disengagement; EC 1: Observed Emotional Caretaking-Task 1; IC 1: Observed Instrumental Caretaking-Task 1; EC 2: Observed Emotional Caretaking-Task 2; IC 2: Observed Instrumental Caretaking, Task 2. PQ-Y: Parentification Questionnaire for Youth. CARETAKING AND STRESS REACTIVITY 36 Table 4. Correlations among children’s caretaking, stress reactivity, and depressive symptoms. EC 1 IC 1 1. YSR .03 n.s -.01 n.s Affective p = .74 p = .87 Problems 2. CES-D .08 n.s -.01 n.s p = .34 p = .89 EC 2 IC 2 PQ-Y RSQ Caretaking IE Parent Report ID Parent Report IE Child Report ID Child Report -.10 n.s p = .21 -.07 n.s p =.39 .35** .09 n.s p = .26 .23** .22** .42** .39** -.16* -.06 n.s p = .46 .44** .11 n.s p = .15 .14 n.s p = .07 .18* .49** .42** 3. CBCL .19* .04 n.s .03 n.s .05 n.s .18* .07 n.s .41** .37** .19* Affective p = .64 p = .71 p = .55 p = .37 Problems *p < .05, ** p < .01 Note. EC 1: Observed Emotional Caretaking-Task 1; IC 1: Observed Instrumental CaretakingTask 1; EC 2: Observed Emotional Caretaking-Task 2; IC 2: Observed Instrumental Caretaking, Task 2. PQ-Y: Parentification Questionnaire for Youth. RSQ: Responses to Stress Questionnaire. .10 n.s p = .20