Impact of process flow tool on wait times from the emergency department to the ICU
advertisement
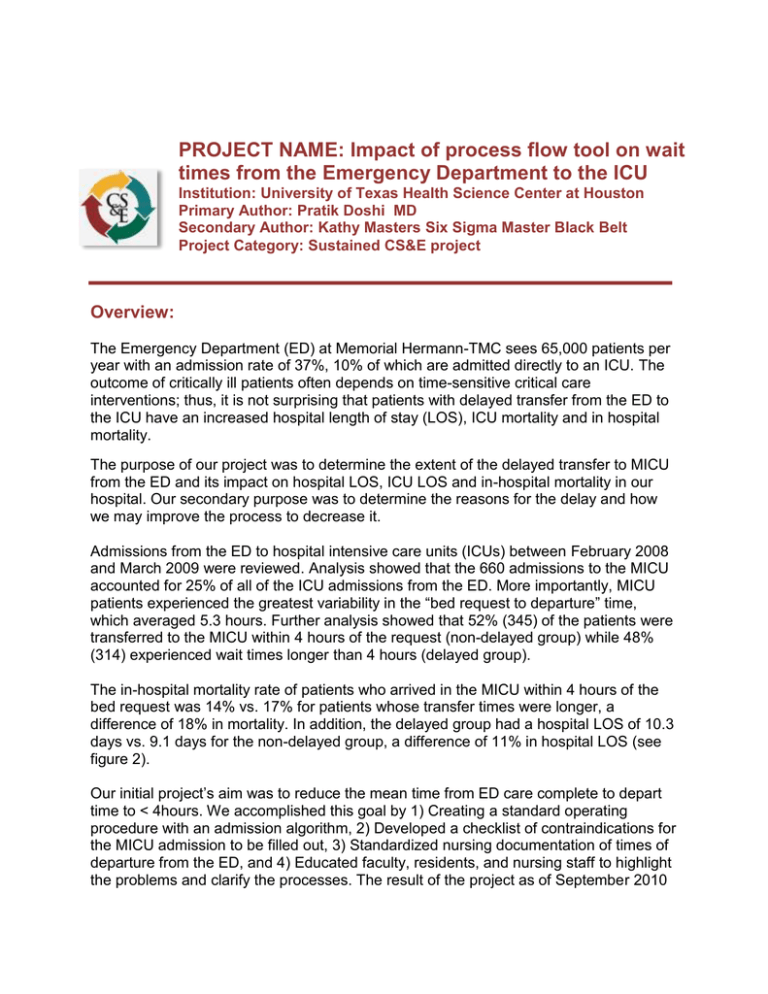
PROJECT NAME: Impact of process flow tool on wait times from the Emergency Department to the ICU Institution: University of Texas Health Science Center at Houston Primary Author: Pratik Doshi MD Secondary Author: Kathy Masters Six Sigma Master Black Belt Project Category: Sustained CS&E project Overview: The Emergency Department (ED) at Memorial Hermann-TMC sees 65,000 patients per year with an admission rate of 37%, 10% of which are admitted directly to an ICU. The outcome of critically ill patients often depends on time-sensitive critical care interventions; thus, it is not surprising that patients with delayed transfer from the ED to the ICU have an increased hospital length of stay (LOS), ICU mortality and in hospital mortality. The purpose of our project was to determine the extent of the delayed transfer to MICU from the ED and its impact on hospital LOS, ICU LOS and in-hospital mortality in our hospital. Our secondary purpose was to determine the reasons for the delay and how we may improve the process to decrease it. Admissions from the ED to hospital intensive care units (ICUs) between February 2008 and March 2009 were reviewed. Analysis showed that the 660 admissions to the MICU accounted for 25% of all of the ICU admissions from the ED. More importantly, MICU patients experienced the greatest variability in the “bed request to departure” time, which averaged 5.3 hours. Further analysis showed that 52% (345) of the patients were transferred to the MICU within 4 hours of the request (non-delayed group) while 48% (314) experienced wait times longer than 4 hours (delayed group). The in-hospital mortality rate of patients who arrived in the MICU within 4 hours of the bed request was 14% vs. 17% for patients whose transfer times were longer, a difference of 18% in mortality. In addition, the delayed group had a hospital LOS of 10.3 days vs. 9.1 days for the non-delayed group, a difference of 11% in hospital LOS (see figure 2). Our initial project’s aim was to reduce the mean time from ED care complete to depart time to < 4hours. We accomplished this goal by 1) Creating a standard operating procedure with an admission algorithm, 2) Developed a checklist of contraindications for the MICU admission to be filled out, 3) Standardized nursing documentation of times of departure from the ED, and 4) Educated faculty, residents, and nursing staff to highlight the problems and clarify the processes. The result of the project as of September 2010 was a 37% reduction in mean time from the ED care complete to depart, from 5.53 hours to 3.49 hours, and 16% reduction in hospital LOS, from 9.67 days to 8.13 days, with the mortality remaining stable. This had resulted in estimated $1,039,500 of cost avoidance over a 12 month period. Aim Statement (max points 150): To ensure that the improvements achieved in the initial project have been sustained and to identify opportunities for further improvement. Measures of Success: • • Mean time from ED care complete to MICU admission Percentage of patients admitted within 4 hours of ED care complete. Use of Quality Tools (max points 250): Process audits were conducted on a quarterly basis for the first year after completion of the initial project, and the results were reviewed. When fall-outs occurred, the project team conducted mini-root cause analyses (RCAs) to determine whether the standard operating procedure flow chart previously developed had been followed and took actions based on the results of the RCAs. Interventions (max points 150 includes points for innovation): The initial few RCAs revealed that the main reason that the standard operating procedure was not followed was that it was thought to be a temporary process for the intervention period, and thus no longer needed to be adhered to. Based on these finding, the team met with all the stakeholders (faculty, residents, nurses and bed management) once again, and reiterated the idea that this is the “standard operating procedure”, and thus should be followed consistently. Over time, the result was that this process became part of the fabric of the culture when it came to admitting patients from the emergency department to the MICU. The project team brainstormed and developed a plan to ensure that all new staff and residents are trained on the process. Additionally, ongoing process audits were conducted to ensure that the process could not slip out of control without notice. Results (max points 250): A convenience sample of 197 patients over a three month period of May thru July of 2012 was collected and the data analyzed, which is now presented in the results. • • Mean time from ED care complete to MICU admission has remained stable at 3.38 hours, as compared to the 3.49 hours during the initial intervention period, which represents a 37% improvement over the baseline of 5.53 hours prior to this project. The percentage of patients transferred to MICU in < 4 hours after care complete in the ED has also remained stable at 73%, as compared to the 74% in the intervention period, which was a 22% increase from the baseline of 52% prior to this project. CC to Depart Baseline Feb 2008-Mar 2009 Sept 2009-Apr 2010 May 2012- July 2012 CC to Depart (in hrs) 5.53 (±5.16) 3.49(±3.49) 3.38(±2.96) Percentage of transfers in ≤ 4 hrs 346 (52%) 474 (74%) 144(73%) Percentage of transfers in > 4 hrs 314 (48%) 169 (26%) 53(27%) Revenue Enhancement /Cost Avoidance / Generalizability (max points 200): The previous study resulted in approximately $1,000,000 of cost avoidance over a 12 month period, primarily due to the reduction in length of stay. For the current sample, this detailed analysis was not completed. However, the impact of this process on patient flow can be extrapolated. There were 643 admissions to the MICU in the year of the initial study and the unit was frequently at capacity. In the current sample, there were 197 admissions to the MICU in a 3 month period, which annualizes to 788 admissions from the emergency department alone. This represents e an increase of 20% in admissions to MICU from the emergency department, which is effective increase in the MICU capacity by that percentage. The impact of this on cost avoidance, revenue enhancement (for both the hospital and the physician) and patient flow are significant. Conclusions and Next Steps: Boarding of critically ill patients in the ED is associated with worse outcomes With focused effort, it is feasible to streamline the process of transferring critically ill patients to the ICU and reduce mean time from “care complete” to admission, which in turn improves the flow of patients through the emergency department as well as the quality of care that is given to the patients who are in the emergency department. The process can be maintained “in control” over an extended period of time with the use of periodic audits and mini-root cause analysis of the fallouts along with with continued education for new staff and physicians. . For continued success, the process has to become part of the fabric of the culture of the hospital, not dependent on a single project team or team leader. The maintenance of this reduction has resulted in sustained improvements in patient flow, which in turn appears to have an impact on the effective capacity of the inpatient unit. While the previously achieved turnaround time has been sustained, further improvement is possible and will be pursued. Additionally, the tools that were successful in streamlining admission to the MICU will be utilized to achieve the same improvements for patients admitted to the shock-trauma and neuro-trauma ICUs.