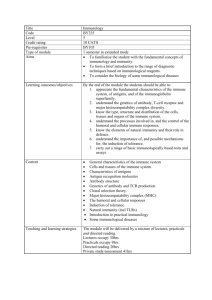
Case 4
advertisement

VS206C: Anatomy and Physiology of the Eye CASE 4: RECURRENT INFECTIONS (IMMUNOLOGY CASE 1) Part 1 Mark, a 2 year old white male, reports to clinic with his mother who reports bilateral ocular redness and discharge. His past ocular history is positive for three similar episodes over the past 12 months. Mark's general health history is positive for a severe bout of 'the flu' a little over one year ago. He has had a chronic, productive cough since. Mark has a healthy 5 year-old sister. Interestingly, his mother reports that her two younger twin brothers died at age 10 months of 'infection'. On ocular exam, vision measures 20/20 OU. External examination shows moderate periorbital swelling and bilateral conjunctival chemosis, hyperemia, petichial hemorrhages, and pseudomembrane formation. The conjunctival hyperemia is more pronounced in the inferior conjunctival fornix. In addition, mucopurulent discharge and matted lashes are noted. Slit lamp biomicroscopy confirms these findings and demonstrates a clear cornea and anterior chamber. A diagnosis of bilateral, conjunctivitis is made and Mark is placed on Neomycin ophthalmic ointment qid OU. Ocular cultures and smears are obtained and two days later implicate Haemophilus influenzae. A phone call with Mark's primary care practitioner reveals that the 3 earlier episodes also involved encapsulated bacteria. A pediatric consult is acquired. Major topics to cover during this case Antigens Natural immunity • complement • macrophages • polymorphonuclear leukocytes (neutrophils) Specific immunity • B-cells • Antibodies: their effector function, their role in the complement system, opsonization and phagocytosis T-cells (just understand what they are - not much detail yet) Cytokines and inflammatory mediators (overview) Haemophilus influenzae and other encapsulated bacteria Neomycin antibiotic Bacterial conjunctivitis The immune response to extracellular bacteria and toxins Topics that you need not get into now: MHC, antibody gene rearrangement, hypersensitivity reactions (except the one that comes up in this case!!!), aspects of cellular immunity not directly covered by this case, immunity to intracellular pathogens, immunity to tumor cells. Some of these will be covered later.... Approach In discussions spend at least 75% of time on the basic immunology (no more than 25% of time on clinical aspects of the case). Remember that this is your basic immunology course and these topics will not be covered again in lecture. Some references are provided on the following page. You are encouraged to find others. Specific approach 1. Understand the clinical signs and symptoms. 2. Answer the following questions: Is the cornea involved? How do you know? Why is the vision normal in both eyes? Will it stay that way? 3. Clearly there is something wrong with Mark's ability to fight infections. Why is this? In order to understand what is going on we need to learn some basic immunology. Guiding Questions What is an antigen? What is the difference between natural and specific immunity? What are the different types of antibodies and their functions? Which cells produce them and how? Which cells have antibody on their surface? What is the function of these surface antibodies? What is complement? What are the two types of complement activation? Could this patient's immune system use both? What are the differences between macrophages and polymorphonuclear leukocytes (neutrophils)? What are cytokines and where do they come from? What is the role of cytokines? How do antibodies act in concert with other aspects of the immune system? Are polysaccharides as efficient antigens as proteins? Are there differences in the way these two types of antigens stimulate an immune response? What are the different aspects of the immune response directed against extracellular bacteria? What is the timing of these events? What is special about encapsulated bacteria in terms of the immune response against them? Part 1: Suggested reading: For the immunology related to the case 1. Read this easy overview before reading any other references!!! NIH Booklet: The immune system - how it works. (9 copies on reserve in folders: VS206C No. 1) 2. Sunshine, Coico. Immunology - a short course. (2 copies on reserve) • Introduction and overview • Elements of innate and acquired immunity • Immunogens and antigens • Antibody structure • Biological properties of immunoglobulins • Biology of the B lymphocyte • Complement 3. “Evading complement, phagocytes and the antibody response.” In Bacterial Pathogenesis: A Molecular Approach (5 copies on reserve in folders: VS206C No. 5) 4. Roitt’s Essential Immunology (Similar to, but more complex than Coico - you may find it better for PMN's, macrophage, and immunity to infection than Sunshine, Coico. (1 copy on reserve) 5. http://pathmicro.med.sc.edu/book/immunol-sta.htm (This is probably the best introductory immunology site on the web.) http://www.nlm.nih.gov/medlineplus/ency/article/001307.htm For the clinical aspects of the case Yanoff and Duker. Ophthalmology. (1 copy on reserve) Various other books are in the library; the following are on reserve (there are many other relevant references too!!) 1. Forrester: The Eye. (2002) (1 copy on reserve) 2. Albert: Principles and practice of ophthalmology: basic sciences. (1 copy on reserve) 3. Kanski: Clinical Ophthalmology. (2 copies on reserve) 4. Tabbara: Infections of the Eye. Chapter 3. Immunology of infections. (1 copy on reserve) 5. Pepose: Ocular infection and immunity. (VS 206B no6) 6. Sell: Immunology, Immunopathology and Immunity. (2001) (1 copy on reserve) Case 4 - Recurrent infections Part 2 Two days later, Mark's mother brings him back to clinic where he is diagnosed with an allergic reaction to Neomycin. Polytrim ophthalmic drops are substituted and the conjunctivitis cleared in one week. Tests from the pediatrician show undetectable antibody titers, no leukocytes with surface immunoglobulin, and decreased erythrocyte sedimentation rate. A genetic consult is acquired and a diagnosis of x-linked agammaglobulinemia is made. Injections of gamma globulin are instituted and the incidence of ocular and respiratory infections significantly decline over the next year. Antibody titers at 3 years of age show near normal IgG and IgM with no detectable IgA. Guiding questions - Part 2. Why is this patient having infections with encapsulated bacteria? How does the immune system develop a memory to foreign antigens? How can he have the same type of infection more than once in his lifetime? Why is the infection bilateral and so severe? Why are there hemorrhages in the conjunctiva? Explain the mucopurulent discharge. What is the pseudomembrane? What type of hypersensitivity reaction is he having to the antibiotic and why does it take 2 days to develop? How can a patient with no antibodies have a hypersensitivity reaction to a drug? Why didn't he have an allergic response to treatment of his previous infections? Why did the infections only begin after 10 months of age? Why is he infection free after gamma globulin treatment when he has no IgA? Can you infer anything about the inheritance pattern of the disease? Suggested reading 1. Sunshine, Coico. Immunology - a short course. (2 copies on reserve) - Immunodeficiency - Hypersensitivity reactions: T-cell-mediated, type IV - delayed type hypersensitivity 2. Mims' Pathogenesis of Infectious Disease. Chapter 6 - The immune response to infection. (1 copy on reserve) 3. Parslow, Stites, et al. Medical Immunology. Chapter 21. (1 copy on reserve)