ELECTRONIC SUPPLEMENTARY MATERIAL
advertisement

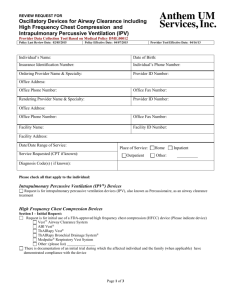
ELECTRONIC SUPPLEMENTARY MATERIAL Chest physiotherapy This treatment consisted of a standard sequence of techniques in three consecutive stages. At the beginning, assisted mucus clearance techniques (suction, postural, and manual drainage) were carried out to increase the cough reflex; subsequently, a nebulised saline solution was applied for 5 min, followed by another sequence of the same techniques; finally, tracheal suctioning was performed. Additional postures and active mobilization were encouraged to facilitate removal of secretions during these sequences. Intrapulmonary percussive ventilation (IPV) This technique provides continuous gas flow to the patient. A continuous and pulsatile gas flow (successive subtidal volumes) was delivered to the patients’ airways by means of an open breathing circuit called Phasitron, whose function is to convert low-flow, highpressure subtidal volumes into high-flow, low-pressure subtidal volumes. In other words, the Phasitron is a flow/pressure converter based on the Venturi principle associated with a pneumatic nebulizer. The circuit is a continuously open breathing circuit. This creates a physiological waveform (the patient inspiratory time corresponding to a pressure decrease) and a low mean intrapulmonary pressure. This technique may be associated with nebulization and has the potential to improve secretion clearance. During the percussive bursts of air into the lungs, a continued pressure is maintained, while a high velocity percussive inflow opens airways and enhances intra-bronchial secretion mobilization. In the present study we have used the IMP2 ventilator (Breas Medical AB, Mölnlycke, Sweden), which has been also used in previous trials (a,b). The device was set at both variable pressure (1.6 to 2.0 bar) and frequency (200 up to 300 cycles/min) according to the patient’s tolerance; I/E ratio was set at 1/1.2 and the maximum proximal airway pressure was limited to 40 cm H2O. a) Piaggi G, Ceriana P, Lazzeri M, Brivio A, Cirio S, Tonoli A, Nava S. (2004) Physiologic evaluation of high frequency intrapulmonary percussive ventilation (IPV) in healthy volunteers. Eur Respir J 24: 315s. b) Nava S, Barbarito N, Piaggi GC, De Mattia E, Cirio S. (2006) Physiological response to intrapulmonary percussive ventilation in stable COPD patients. Respir Med 100: 15261533.