summer12humanbio#2.ppt
advertisement

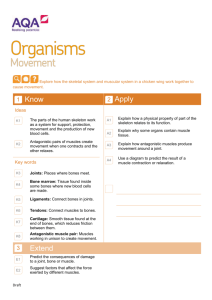
Bones, Muscles, Blood • Skeletal System is made up of bones, the ligaments that bind bones together, and cartilage • Bones are the hard elements of the skeleton whose function is to: 1. Support the muscles & soft organs 2. Interact with muscles 3. Protect delicate internal organs 4. Contain bloodproducing cells 5. Store minerals like calcium & phosphate • Parts of a long bone are the shaft (diaphysis) and ends (epiphyses) • Compact bone makes up the periphery, spongy bone internally, and the cavity is filled with yellow bone marrow (fat), except for a few places of red marrow- the hip, sternum, ribs, skull, and epiphyses of the humerus & fumur (produces RBC’s & WBC’s & platelets) • Spongy bone (trabecular) is in the epiphyses & extends from compact bone into marrow • Bone is covered with a periosteum membrane, epiphyses covered with cartilage • Bone is hard because of extracellular calcium phosphate, which surrounds osteocyte cells • The cells are in spaces called lacunae that are arranged in osteons (Haversian system) surrounding a central canal that carries blood vessels, canaliculi connect them • Ligaments attach bone to bone, and are made of dense fibrous connective tissue with collagen • Cartilage has strands of collagen, and is smooth & flexible • Fibrocartilage has bundles of collagen, and make up the intervertebral disks & menisci of knee • Hyaline cartilage has a glassy appearance, is found at articulations, & forms the embryonic models of bone • Elastic cartilage is most flexible and found in the ear & epiglottis • Embryos have hyaline cartilage with chondroblasts surrounded by perichondrium, instead of bone, for most of their skeleton • The perichondrium eventually forms a bony collar • The cartilage inside the bony collar dies - nutrients can’t diffuse through bone – and then becomes calcified • Blood vessels invade the calcified cartilage, osteoblasts enter & secrete osteoid proteins and enzymes that help with the crystallization of extracellular calcium phosphate salts - forming hydroxyapatite • Grow in length occurs at the growth plate, which is stimulated by growth hormone • Growth stops when sex hormone levels rise • Ages 18 – females and 21 – males • Osteoclasts remodel bone by dissolving hydroxyapatite & digesting osteoid, releasing calcium & phosphate ions into the blood • Shapes of bone change in response to mechanical forces – weight bearing exercises increase overall bone mass & strength • Osteoporosis – bones lose mass to release calcium to maintain body levels of calcium • If there is low body calcium levels, parathyroid hormone stimulates osteoclasts to digest bone, with high levels, calcitonin stimulates osteoblasts to make bone • 10 million Americans have osteoporosis • 1.5 million fractures/year • Contributing factors include low calcium levels, estrogen decline, smoking, sedentary lifestyle, underweight • Steps in healing a fracture – • A hematoma (blood clot) forms within hours, then a fibrocartilage callus fills in the space within days, and is replaced by a bony callus within months, remodeled bone resembles prefracture status after a year • Bone classification is by shape: • Long bones • Short bones • Flat bones • Irregular bones • 206 bones in human body are divided into the axial & appendicular skeletons • Skull has 2 categories: • Cranial bones surround the brain: frontal, parietal, temporal, sphenoid, ethmoid, occipital bone • Facial bones: maxilla, palatine, vomer, zygomatic, nasal, lacrimal bones • Mandible – the chin, hyoid bone – at top of neck • Sinuses make the skull lighter, and develop shortly before and after birth as invaginations from the nasal cavities • The vertebral column supports the head, protects the spinal cord, attaches limbs • 33 vertebrae bones with spinous processes • 7 cervical • 12 thoracic • 5 lumbar • 5 fused sacrum • 4 fused coccyx • Intervertebral disks • 12 pair ribs • sternum • The pectoral girdle (scapula and clavicle) attaches the upper extremity to the axial skeleton • Humerus arm • Radius, Ulna forearm • 8 Carpals wrist • Hand has 5 Metacarpals & 14 Phalanges • The pelvic girdle attaches the lower extremity to the axial skeleton, made up of the coxal bones: • Iliac crest • Ischial tuberosity • Pubic symphysis • Femur – thigh bone • Tibia & Fibula are the leg bones • 7 tarsals at the ankle • Foot has 5 metatarsals & 14 phalanges • Joints connect bones to each other and are tabilized by ligaments & tendons • Fibrous joints – immovable (skull sutures) • Cartilagenous joints – slightly movable – intervertebral disks • Synovial joints – freely movable and lined with a synovial membrane • Examples of hinge joints are the knee & elbow • Knee: fibrocartilage menisci deepen the joint on the tibia, cruciate ligaments cross inside the joint between the tibia and fibula, and collateral ligaments hold it together on the sides • Examples of ball and socket joints are hip, shoulder • Tendons are what attach muscles to bones • A sprain is a partial tear to a ligament or tendon • Bursitis is inflammation of a bursa that protects a tendon • Tendinitis is inflammation of a tendon • Arthritis is inflammation of a joint – osteoarthritis is loss of cartilage at the joint • Muscles make up: • 40% of body weight males • 32% of body weight in females • Includes skeletal, cardiac, and smooth muscle cells • Muscles produce or resist movement, maintain blood pressure, generate heat • Muscles cells are excitable and can contract & relax • Skeletal muscles interact with skeleton & cause bones to move • >600 skeletal muscles • Work together as synergistic & antagonist groups – one side contracts while the opposite side relaxes • Attach to bones by tendons • Muscles consist of groups of multinucleated muscle cells (fibers) and bundles of fibers are called fascicles, enclosed in fascia sheath • Fibers contain sarcomeres – segments between Z lines that attach actin microfilaments • Myosin & actin microfilaments – made of protein – interact to cause muscle contraction • Motor neurons stimulate muscle contraction by releasing acetylcholine (ACh) at the neuromuscular junction • ACh causes the membrane (sarcolemma), including indents called t-tubules, to depolarize, allowing an influx of sodium ions, which causes the release of calcium ions from the sarcoplasmic reticulum terminal cisternae • Calcium ions allow myosin to contact the myosin binding site on actin, form crossbridges, split ATP, and swing, grab the next binding site, repeat; like pulling a rope - the ‘sliding filament’ mechanism • Troponin is attached to tropomyosin that wraps around the actin & hides the myosin binding site • Binding splits ATP bound on myosin into ADP & P, which then falls off the myosin so another can take its place • Muscles store enough ATP for 10 seconds of activity • Creatine phosphate is a molecule that attaches phosphate to ADP for 30 - 40 more seconds of activity • Muscles need stored glycogen for a quick source of glucose (anaerobic – 2 ATP, forming lactic acid) • Aerobic respiration takes place in mitochondria, requires oxygen, and oxygen debt occurs from build-up of lactic acid before aerobic kicks in • Muscles will store more glycogen, develop more mitochondria and capillaries to bring oxygen, if they are active all the time • Fatigue - from lack of ATP • Isotonic contractions – muscle shortens while maintaining a constant force • Isometric contraction – force is generated & muscle tension increases but bones do not move • Motor neurons stimulate muscles by releasing ACh • A motor unit consists of all the muscle cells that a neuron stimulates - an all or none situation • One action potential cause a muscle twitch • Muscle tone is produced by an intermediate level of force, causing some fibers to contract • Increasing force recruits more motor units • After stimulation and contraction there is a latent period where the membrane repolarizes and calcium transports back • Additional stimuli cause greater force • An increase of force by an increase of rate of stimulation is called summation • Too much summation with no relaxation is tetanus – sustained contraction – that leads to fatigue • Rigor mortis – myosin can not unlock from actin • Slow twitch muscles contract slowly, use aerobic metabolism – have many mitochondria & blood vessels, little glycogen, store oxygen in myoglobin – body posture • Fast twitch muscles contract more quickly, have fewer mitochondria, store glycogen, need creatine phosphate & anaerobic metabolism, are unable to sustain long contractions (but can use aerobic mechanism too) – used for quick movements • Strength training builds more myofibrils, glycogen and creatine phosphate storage capacity • Aerobic training increase capillaries, mitochondria, myoglobin • Involuntary muscle types: • Cardiac – connected by intercalated discs, rhythm set by pacemaker cells – make up the heart • Smooth muscles – joined by gap junctions – make up walls of the guts and blood vessels • Myasthenia gravis – destroys acetylcholine receptors on skeletal muscle cells • Muscular dystrophy – abnormal dystrophin protein allows calcium to leak into muscle cells • Tetanus – bacterial toxin overstimulates the nerves controlling muscle activity, especially jaw & neck muscles, causing sustained contraction • Muscles of the Body • Facial expression: frontalis, zygomaticus major, orbicularis oris, orbicularis oculi, depressor anguli oris • Back: trapezius, latissimus dorsi, erector spinae • Chest and abdomen: pectoralis major, serratus anterior, external oblique, rectus abdominus • Upper extremity: deltoid, biceps brachii, triceps brachii, brachioradialis • Lower extremity: gluteus maximus, sartorius, quadriceps, tibialis anterior, hamstrings, gastrocnemius • The circulatory system is made up of the heart, blood vessels & blood • Supplies cells with nutrients from digestive system and removes wastes with urinary system • Exchange of gases with interaction with the respiratory system • Blood is classified as a connective tissue with cells in a watery extracellular matrix, functions include: • Transportation of all substances needed by the body – oxygen, nutrients, hormones, wastes • Regulation of body temperature, volume, and pH • Has defense cells to protect against infection & the ability to clot to prevent blood loss • Humans have 4-6 liters of blood – approximately a gallon • Blood has red blood cells, white blood cells & platelets • Plasma makes up 55% of the volume of blood and contains water, ions, proteins, hormones, gases, nutrients, wastes • Plasma proteins include albumin, globulins, clotting proteins • Electrolytes (ions) are sodium, potassium, chloride, bicarbonate, calcium, hydrogen, magnesium • Hormones, nutrients are transported in blood • Wastes include carbon dioxide, urea, lactic acid • Red blood cells have no nuclei, a biconcave disc shape, and transport oxygen • One cubic millimeter of blood has ~ 5 million RBC’s and each cells had ~ 300 million hemoglobin molecules/cell • Globulins have heme groups with iron atoms that bind oxygen, 4/molecule • RBC’s have no mitochondria, rely on glycolysis for energy, and make carbonic anhydrase to transport most of the carbon dioxide • A hematocrit measures the amount of cells • Stem cells in red bone marrow produce RBC’s, and are called normoblasts (or erythroblasts) • RBC’s live only 120 days and old ones get removed by liver & spleen cells called macrophages • Bilirubin pigment from hemoglobin gets secreted into bile and is taken up in urine, causing dark brown or yellow coloration • A hormone called erythropoietin which is secreted by the kidney stimulates RBC production • • • • • • There are far fewer white blood cells – 7,000/cubic millimeter – which are classified as granular or agranular types, also made in red bone marrow Neutrophils – 60% - function in infection Eosinopils – 2% - fight parasites, engulf immune complexes, moderate allergic reactions Basophils – 1%, granules initiate inflammatory response Monocytes – 5% - become macrophages in tissue Lymphocytes – 30% - function in immune response • Platelets are known as ‘formed elements’, break off of large bone marrow cells called megakaryocytes – 250,000/cubic millimeter of blood • Function in hemostasis • Steps in blood clotting after initial injury: vascular spasm, formation of platelet plug, coagulation • Vascular spasm happens within ½ hour – a platelet plug forms when platelets adhere to exposed vessel wall collagen & von Willebrand factor, damaged cells cause release of prothrombin activator, a reaction that requires calcium • Formation of thrombin from plasma proteins converts fibrinogen into fibrin that weaves around and secures the platelet plug • Hemophilia is caused by a deficiency of clotting factors • Hemophilia A is X-linked, so boys are more prone to inheriting it – lack of factor VIII • Blood types - blood antigens are inherited equally from parents & antibodies are produced to protect against wrong blood types – include A, B, O & Rh factor • Anemia is defined as a reduction in blood’s oxygencarrying ability, there are many diffferent types: iron deficiency, hemorrhagic, pernicious, hemolytic, and sickle cell anemia • Leukemia is a cancerous overproduction of one type of blood cell • Multiple myeloma is the cancerous overproduction of an activated B lymphocyte • Mononucelosis – infection of lymphocytes with Epstein-Barr virus • Thrombocytopenia – reduction in amount of platelets • The immune system protects the body from pathogens like bacteria, viruses, fungi, protozoans, prions, parasites, and involves white blood cells • Bacteria are single celled prokaryotes (have no nucleus) that decompose, make products like drugs, hormones, vaccines, food, produce energy and make vitamins in our digestive tract, live on our skin & mucous membranes, but can cause infections • VIRUSES – TINY INFECTIOUS AGENTS, THAT CONSIST OF A SMALL PIECE OF RNA OR DNA SURROUNDED BY A PROTEIN COAT • ENTER CELLS AND INSERT GENETIC MATERIAL TO REPRODUCE • Prions – infectious proteins like bovine spongiform encephalopathy Creutzfeldt Jakob disease • Prions convert normal brain cell protein • Transmission and virulence determines disease • The lymphatic system defends the body, returns excess tissue fluid, transports fats • Lymph nodes filter lymph vessels and lymph eventually enters circulation at the subclavian vein • The spleen cleans blood in its red pulp and fights infection with its white pulp • Thymus gland produced T lymphocytes • Tonsils are patches of lymph tissue in the throat • The skin is a good barrier to infection and sweat has an antibiotic & low pH • Tears, saliva, cerumen also have lysozyme • Vomiting, urination, defecation rid body of harmful wastes • Resident bacteria on the skin and mucus membranes prevent bacterial infections from other bacteria • Inflammation can be caused by infection or damage and signs are rubor, dolore, calore, tumor, stupor, discharge • Injured cells release chemicals that cause mast cell histamine release that causes vasodilation and attracts neutrophils, monocytes & macrophages, lymphocytes & natural killer cells • Activation of complement, fever, interferons to protect neighboring cells • Phagocytosis by neutrophils and macrophages begins the cellular part of inflammation, macrophages process what they engulf and split it into different antigens • The body’s immune response relies on the major histocompatibility complex, which is a marker on every cell membrane (except RBC’s) that is unique for each person • Antigenpresenting cells like macrophages activate B & T lymphocytes designated for that specific antigen • Antibodies made by plasma cells (transformed B lymphocytes) are specific for antigens • IgG, IgM, igA, IgD, IgE bind to antigens • After 1st exposure – measurable after 14 days, 2nd exposure causes immediate response • Antigen presenting cells also stimulate T cell response • Cytokine proteins activate cells • Cytotoxic T cells destroy cells • Immune memory - Primary response in 2 weeks • Second response in a few hours - immunization – active & passive • Monoclonal antibodies are used as drugs • Type I allergic response – antibody known as IgE causes histamine release from basophils and mast cells • Type II & III allergic responses are antibodymediated as well • Type IV – tissue rejection, poison ivy response, comes from T cells • Autoimmune disorders include rheumatoid arthritis, lupus erythematosus, multiple sclerosis, grave’s disease, diabetes mellitis type I • HIV virus is specific for CD4 receptors- disables the T helper lymphocytes - T helper count < 200/cubic millimeter, allows an opportunistic infection or cancer to take over the body