Medical Complications of Illicit Drugs
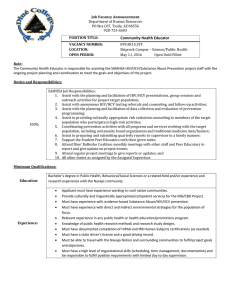
advertisement

Medical Complications of Drug Use Jeanette Tetrault, MD Assistant Professor of Medicine Yale University School of Medicine Focus of today’s discussion • Complications of Injection Drug Use (IDU) – Acute • Withdrawal • Bacterial infections: Skin, endovascular – Chronic • Hepatitis B • Hepatitis C • HIV – Prevention – Mortality and drug overdose Case: 31 yo man presents to ED feeling “sick” • • • • • • • • 10 year history of injection heroin use 6 month history of increasing cocaine use Symptoms - myalgias, weakness, cough No history of TB or HIV PE – T 101.2, fresh and old track marks No cardiac murmur, non-tender abdomen Labs - WBC 12,000 with normal differential Urine-trace protein Should the patient be hospitalized? • What clinical diagnoses are likely based on this presentation? • Which of these diagnoses merit hospitalization? Presentation of febrile IDUs • Of 296 febrile IDUs presenting to urban teaching hospital, 64% (180) had apparent major illness: • Therefore, 36% (103) without apparent illiness 89% (92) with minor illness Abscess 6% Cellulitis 37% Endocarditis 6% Pneumonia 34% Samet JH, Shevitz A, Fowle J, Singer DE. Am J Med. 1990;89:53-57 11% (11) with major illness Diagnoses of patients with occult major illness Patient Diagnosis Bacteremia 1 Infective Endocarditis Group G β-hemolytic streptococcus 2 Infective Endocarditis Staphylococcus aureus 3 Infective Endocarditis Staphylococcus aureus 4 Infective Endocarditis Staphylococcus aureus 5 Infective Endocarditis Staphylococcus aureus 6 Infective Endocarditis Staphylococcus aureus 7 Infective Endocarditis Staphylococcus viridans 8 Pneumonia None 9 Pneumonia None 10 Disseminated intravascular coagulation None 11 Deep venous thrombosis None Management of febrile IDUs • Significant univariate predictors of major illness – Fever (RR 4.76, 95% CI1.52-14.92) – Last IDU < 5 days PTA (RR 6.30, 85% CI 1.05-37.79) – Proteinuria (RR 4.44, 95% CI 1.27-15.5) • Recommendations for febrile IDUs – Decision to hospitalize rests on need for follow-up after blood cultures returned – If follow-up is not possible, patients should be hospitalized Case follow-up • Tests – Chest x-ray-normal – Blood cultures negative after 24 hours • Assessment/Plan – Diagnosis-Viral Syndrome – Patient discharged home – Referred for substance abuse counseling Heroin: A brief history • 1874-first synthesized by an English chemist – Diacetyl-morphine • 1897-resynthsized by Felix Hoffman working for Bayer trying to produce codeine • 1898-1910-marketed as a cough suppressant and non-addictive morphine substitute – Then discovered it was metabolized to morphine • 1914 Harrison Narcotics Act banned sale and distribution • 1924 became a Schedule 1 drug Injection drug use • Lifetime prevalence 1.33% (NSDUH, 2008) • 425,000 current IDUs • Medical complications of IDU result from: • Taking compound of uncertain composition • Solubilizing compound with a solvent (usually water) that has been sterilized to a widely-varying degree • Sterilizing the resulting mixture to a widely-varying degree • Violating the body’s most effective barrier vs. infection through use of needle • Injecting mixture directly into vasculature Acute complications: Opioid withdrawal • Severe flu-like symptoms • Anxiety • Hyperactivity • Drooling • Lacrimation/Tearing • Rhinorrhea/Runny nose • Anorexia • Nausea • Vomiting • Diarrhea • Myalgias • Muscle spasms IDU acute infectious complications: Soft tissue • Cellulitis, abscess, fasciitis: most likely reason for IDU hospital admission • Sites: any site of injection • Organisms: predominantly staph. and strep. • Antibiotics may fail due to local necrosis of vessels (especially in those who inject cocaine) • Drainage, often multiple times, may be required IDU acute infectious complications: Endocarditis • High risk of “right-sided” endocarditis – “left-sided” still more common • Usually skin flora – may be mouth flora from needle-licking • High degree of suspicion in febrile IDU (+/- heart murmur) – Blood cultures • Infection may be relatively benign or highly virulent • Treatment – Long term antibiotics – Surgery if valvular destruction, abcess or cerebral emboli Samet, Am J Med, 1996 IDU acute infectious complications: Endovascular • Septic emboli – Small colonies of bacteria flick off vasculature (valves, vessels) into soft tissue/organ parenchyma • Metastatic seeding – Transient bacteremia from injection can settle in bone, muscle, joint space etc Harm reduction for IDUs • • • • • Use clean needles Use sterile water as solvent Rotate injection sites Alcohol wipes on skin Do not lick needles IDU chronic infectious complications: Viral • Hepatitis B • Hepatitis C • HIV Epidemiology of Hepatitis B • • • • Estimated 1.25 million chronically infected in U.S. Approximately 300,000 new cases per year Transmission is blood borne, sexual, or perinatal Approximately 50% of active injection drug users have serological evidence of prior exposure to HBV Natural history of Hepatitis B • Early disease manifests with symptoms of hepatic inflammation with elevated LFTs (> 10-20x normal) • Chronic viral hepatitis manifests as chronic liver disease with portal hypertension and poor hepatic synthetic function • Likelihood of developing chronic infection is related to age: – 80 to 90% of infants infected develop chronic disease – only 2 -10% of infected adults progress to chronic disease Epidemiology of Hepatitis C (HCV) • Most common blood-borne infection in the U.S. • Incidence: 35,000 new cases per year in U.S. • Seroprevalence studies reveal that approximately 1.8% of the U.S. population have been infected with HCV • IDU is the major risk factor for HCV – 65% of new cases – 20-50% of chronic infections – 40-90% of injection drug users (IDUs) have HCV antibodies National Institutes of Health Consensus Development Conference Statement: Management of hepatitis C: 2002--June 10-12, 2002 Hepatology. 2002 Nov;36(5 Suppl 1):S3-20 Natural history of HCV Acute HCV HCV Antibody + 10-20 years Resolved 15% to 20% Chronic HCV 80% to 85% Stable 85% to 90% Cirrhosis 10% to 15% Slowly progressive 75% HCC, liver failure 25% (2% to 4%) NIH Management of Hepatitis C Consensus Conference Statement. June 10-12, 2002. Available at: http://consensus.nih.gov/2002/2002HepatitisC2002116html. Sexual Transmission of HCV • Efficiency low • Rare, but not absent—estimated 0.03-0.6% per year between long-term monogamous discordant partners— no change in sexual practices recommended • Risk amongst those with multiple sexual partners is 1% per year—barrier methods or abstinence recommended • Presence of other sexually transmitted diseases increases risk of transmission Factors influencing progression of HCV • Virus • Behaviors and Environment – Viral Load – Alcohol use – Genotype – Drug use (licit and illicit) • Host – HBV co-infection – Sex – HIV co-infection – Age – Fatty liver infiltration – Race – Iron overload – Duration of infection – Genetics – Immune response Patients* With HCV infection (%) Liver Function Tests in HCV 100 80 60 42 43 40 15 20 0 Persistently Normal ALT Intermittently Elevated ALT Persistently Elevated ALT *Patients with ≥ 4 serum ALT level measurements during 25 months of follow-up (n = 1042). Inglesby TV, et al. Hepatology. 1999;29:590-596. Treatment milestones in HCV • RVR= rapid virologic response; week 4 – Absence of detectable HCV quantitative viral load • EVR= early virologic response; week 12 – cEVR=absence of detectable HCV quantitative viral load – pEVR=greater than 2 log (10) reduction in HCV viral load • EOTR=end of treatment response – Week 48 for genotype 1 and 4 infection or HIV-coinfection – Week 24 for genotype 2 and 3 infection • SVR=Sustained virologic response – Absence of detectable viral load 24 weeks after end of treatment Treatment of HCV: Pegylated IFN + Ribavirin • Goal of treatment=SVR – 42% for genotype 1 – 82% for genotypes 2 and 3 • Side effects – Pegylated interferon • Flu-like symptoms, depression, • 5-10% require discontinuation of therapy – Ribavirin • Pancytopenia, hemolytic anemia IDUs and Treatment of HCV • 2002 NIH guidelines on treatment of HCV – Management of HCV-infected IDUs is enhanced by linkage to drug treatment programs – Promotes collaboration between HCV experts and addiction medicine experts – HCV treatment of active IDU should be considered on a case-by-case basis – Active IDU should not exclude patients from HCV treatment Patients (%) Methadone treatment and HCV 100 90 80 70 60 50 40 30 20 10 0 P = .01 76 P = .16 50 56 42 n= 50 50 50 ETR SVR Response Outcomes Mauss S, et al. Hepatology. 2004;40:120-124. 50 Controls (no IDU for ≥ 5 years) Patients on methadone maintenance Emerging therapies for HCV: Direct acting antivirals (DAA) Receptor binding and endocytosis Transport and release Fusion and uncoating ER lumen (+) RNA LD LD Translation NS3/4 and protease polyprotein inhibitors processing Boceprevir Telaprevir Virion assembly LD Membranous web ER lumen NS5A* inhibitors *Role in HCV life cycle not well defined Adapted from Manns MP, et al. Nat Rev Drug Discov. 2007;6:991-1000. NS5B polymerase RNA replication inhibitors Nucleoside/nucleotide Nonnucleoside HIV/AIDS • A blood-borne retroviral infection caused by the human immunodeficiency virus (HIV) • Transmission is through sexual contact, parenteral exposure, and perinatal or postpartum contact • 25% of the approximately 40,000 new HIV infections per year are through IDU • IDUs with HIV are less likely to receive antiretroviral treatment • IDUs less adherent to antiretroviral therapy, but addiction treatment found to increase medication adherence HIV/AIDS treatment • Standard is at least a three-drug regimen frequently called highly active antiretroviral therapy (HAART) • Medication classes: a)Nucleoside reverse transcriptase inhibitors (e.g., Zidovudine or AZT) b)Nucleotide reverse transcriptase inhibitors (e.g., Tenofovir or Viread) c)Non-nucleoside reverse transcriptase inhibitors (e.g., Efavirenz or Sustiva) d)Protease inhibitors (e.g., Indinavir or Crixivan) e)Membrane fusion inhibitor (e.g., enfuvirtide or Fuzeon or T-20) f) Newer Classes of medications (e.g., integrase inhibitors, CCR5 inhibitors) HIV seroconversion • Reduced by opioid agonist treatment among IDUs • Metzger, 1993: 2 cohorts of patients – 103 out-of-treatment intravenous opiate users – 152 subjects receiving methadone treatment HIV antibody conversion, 18-months – 22% of those out-of-treatment – 3.5% of those receiving methadone treatment Metzger DS, et al. Human immunodeficiency virus seroconversion among intravenous drug users in- and out-of-treatment: An 18 month prospective follow up. JAIDS. 1993 Methadone and HIV Prevention • Methadone patients report less needle and syringe sharing • Methadone patients are 3-6 times less likely to become HIV positive when compared to out-of-treatment heroin users, including the population who continues to use drugs De Castro S, Sabate E. Adherence to heroin dependence therapies and human immunodeficiency virus/acquired immunodeficiency syndrome infection rates among drug abusers. Clin Infect Dis. 2003 Dec 15;37 Suppl 5:S464-7 Buprenorphine and HIV prevention • Buprenorphine is a partial opioid at the µ-opioid receptor, treatment option for opioid dependence • Longitudinal analysis of primary care patients on buprenorphine† – N=166 patients – Decreased risk behaviors between baseline and 24 weeks • IDU: 37% to 7%, p<0.001 • Sex while high: 64% to 15%, p<0.001 † Sullivan LE et al. Buprenorphine/naloxone treatment in primary care is associated with decreased HIV behaviors. JSAT. 35: 87-92. 2008. Buprenorphine and HIV treatment • MANIF cohort* – N=164 pts on HAART; 32 on bup, 113 prior IDU, 19 active IDU – Those on buprenorphine were more likely to be adherent to HAART than those with active IDU (OR 5.1 95%CI 1.3-20.1) – 6 mo follow-up no difference in CD4 and VRL between patients on bup and prior IDU • HIV+, opioid dependent patients treated with bup† – N=16 patients – + Utox 100% to 16% at 3 mos – No difference in HIV parameters *Moatti JP, et al. Adherence to HAART in French HIV-infected injecting drug users: the contribution of buprenorphine drug maintenance treatment. AIDS. 14(2) :151-5, 2000. † Sullivan, LE et al. A trial of integrated buprenorphine/naloxone and HIV clinical care. Clinical infectious diseases. 43 suppl:184-190, 2006. Methadone interactions with antiretrovirals • Nucleoside reverse transcriptase inhibitors – Methadone increases AZT through inhibition of glucoronidation – May increase side effects of AZT • Non-nucleoside reverse transcriptase inhibitors – Efavirenz decreases methadone levels – May cause withdrawal • Protease Inhibitors – No clinically significant interactions Buprenorphine interactions with antiretrovirals • Nucleoside reverse transcriptase inhibitors – No clinically significant interactions • Non-nucleoside reverse transcriptase inhibitors – Efavirenz decreases buprenorphine levels – Not clinically significant • Protease inhibitors (P450 3A4) – Atazanivir increases buprenorphine levels – May cause sedation Routine screening for patients with addiction • Viral Hepatitis A, B, C: Screening antibody tests and liver enzymes • HIV screening yearly • Tuberculosis: Annual screening with PPD and/or chest xray • Syphilis: Annual VDRL or RPR • Cervical cancer: Yearly screening PAP smear, more frequent (q6month) in those with prior abnormalities • Immunizations: pneumovax, flu, Tdap, twinrix Mortality as a result of drug overdose • Death from overdose is rare but may have spikes of increased incidence due to increased purity of illicit drugs • Particularly vulnerable times – Release from prison – Discharge from drug treatment • Respiratory depression is a factor BUT CNS depression is often the cause – Mixture of CNS depressants have additive effect; mixture of opioids/stimulants has complex interaction Other factors affecting mortality • Harder to quantify and usually ignored – Poor preventative care, uninsurance/underinsurance, fragmented healthcare – Poor health literacy – Poverty, malnutrition – Co-occuring and often poorly recognized/treated mental illness Summary • Patients with addiction frequently have co-morbid medical conditions, especially infectious diseases • Important to screen for these disorders, and to provide treatment and prevention interventions • Monitor patients for interactions between medications used to treat addiction and medications used to treat chronic diseases • Linkage of addiction treatment with medical treatments and prevention for co-morbid disorders can enhance medical treatment outcomes Thank you!