Yale Medical Billing Compliance Program Manual Overview
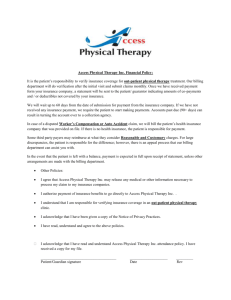
advertisement

Yale Medical Billing Compliance Program Manual Overview The Yale University School of Medicine ("YSM") holds that the long-term success of its programs is intimately tied to its reputation for integrity. The School's Medical Billing Compliance Program is designed to safeguard and enhance that reputation by defining a comprehensive effort to attain the Program's goals: adequately documented and uniformly accurate medical bills issued by or through the School. Although the task of billing may seem largely technical and generally remote from public scrutiny, experience shows that carelessness in billing can too quickly lead to a reputation compromised by public suspicions of wrongdoing, no matter how ill-founded. For this reason, and despite the many competing demands on your time, we strongly urge all members of the School's clinical community to devote significant energy and resources to making the Medical Billing Compliance Program an effective one. In accordance with its commitment to compliance with applicable laws and regulations and to ethical business practices, the Yale Corporation, through its Audit Committee, has approved the Yale University School of Medicine Medical Billing Compliance Plan (the "Plan"), attached as Appendix A. The Plan provides the blueprint for the School's Medical Billing Compliance Program (the "Program" or the "Billing Compliance Program"), which encompasses all of the School's efforts to achieve correct coding and adequate documentation and to ensure that all aspects of medical billing and collections are handled in accordance with applicable laws and regulations. This Medical Billing Compliance Manual has been prepared to explain the Program and to give detailed guidance about it to those who must comply. As the Manual describes, the Program contains educational, oversight, auditing, disciplinary and other components. Promulgated under the aegis of the Dean of the Medical School in accordance with the Yale Corporation's approval of the Plan, the Program charges the Director of the Yale Medical Group ("YMG") with supervising its implementation. Primary responsibility for day-to-day medical billing operations rests with the Executive Director of the School's Patient Financial Services, who works closely with the School's Director of Compliance. Each health care provider and staff member involved in billing has an important role to play in the Program, however. The obligations of each person covered by the Program are described in detail in this manual below. Please read the Manual with care. Table of Contents I. Medical Billing Policy It is the policy of Yale University School of Medicine to appropriately bill for professional services provided. The University recognizes that special billing requirements may apply to certain government-sponsored programs or to other providers. Any such requirements must be followed. In selecting codes to describe services rendered, University physicians, other health professionals, and billing personnel are to select codes that they believe, in good faith, correspond to services actually rendered, as documented in the medical record. University clinicians, other health professionals, and billing personnel have a collective responsibility to be knowledgeable about the meaning of the codes applicable to their area of practice, including relevant directives from billing authorities. The University further recognizes the importance of maintaining accurate patient accounts in accordance with applicable requirements. University physicians, other health professionals, and billing personnel should never submit a claim that is known to contain inaccurate information and any payments that are received in error will be refunded. When in doubt about how to bill a particular service, including the proper code to use, no Program Participant should submit any claim until appropriate guidance is obtained from departmental compliance leaders or from the Director of Compliance. The billing physician or other health professionals are responsible for ensuring that appropriate documentation supports the bill being submitted. II. Does the billing compliance apply to you? The Billing Compliance Program implements and enforces the University's medical billing policy. A "Program Participant" is an individual who is covered by the Billing Compliance Program and must comply with it. You are a Program Participant if you hold one of the following positions. 1. Health Care Providers: Physicians and Others. The following four categories of health care providers are Program Participants: Physicians for whom the School provides billing services. You are a Program Participant if you are a physician employed by the School on a full- or part-time basis (whether a clinical, teaching, community- based or other physician, or moonlighting fellow) and the School prepares and issues bills for your services. Other health care providers for whom the School provides billing services. You are a Program Participant if you are a nurse practitioner, a clinical nurse specialist, a physician's assistant, a licensed social worker, licensed psychologist, or any other health care provider employed by the School on a full- or part-time basis, and the School prepares and issues bills for your services. Other physicians and health care providers employed by the School. You are a Program Participant if you are a physician or other health care provider employed by the School either full- or part-time, charges for your services are payable to the School, and a nonSchool entity (such as a contractor) prepares and issues bills for your services. Residents and fellows. You are a Program Participant if you are a resident or fellow at the School who participates in the care of patients for which billing is done by the School of Medicine. You should consult with the Director of the Yale Medical Group or the Director of Compliance to determine when and how the Program applies to you. 2. Administrative Personnel. You are a Program Participant if you are employed as a School administrator and are responsible for medical billing. 3. Support Staff. You are a Program Participant if you hold a support staff position at the School and you participate in any way in the medical billing process. 4. Non-employees of YSM Who Are Involved in YSM Medical Billing. Entities and individuals who are not employed by the School but are involved in the School's medical billing process ("related participants") are affected by the Program. The School will advise current related participants of the Program and will request their compliance with it. Entities and individuals who become related participants after implementation of the Program may be required to comply with the Program in at least four ways as a condition of their relationship with the School: (a) attend educational programs; (b) review YSM compliance publications; (c) accede to and assist in carrying out the Program's monitoring functions; and (d) report potential compliance issues to appropriate authorities. III. School Administrators' Roles in the Billing Compliance Program Oversight responsibilities for the Program have been assigned to several individuals and groups in the School's administration, as described below. (Yale University officials will also play roles in the Program's operations, as set forth from time to time in this Manual.) 1. The Dean. The Dean is responsible for implementing the Program. The Dean has delegated certain of his responsibilities under the Program to the Chief Operating Officer of the School (the "COO"). As the Dean's designee, the COO imposes discipline for noncompliance with the Program, in close consultation with the Director of the Yale Medical Group (the "YMG"). Also as the Dean's delegee, the School's COO is charged with reviewing any proposal by a clinical department (a) to use an entity other than the Patient Financial Services (PFS) for its billing; (b) to manage its own billing compliance plan other than through two Billing Compliance Leaders (as described in Article IV, below); and (c) to staff the position of the Billing Compliance Resource Specialist in cooperation with another department. 2. The Director of the Yale Medical Group The Director of the Yale Medical Group bears primary responsibility for implementing and managing the Program. He/she supervises the activity of the Director of Compliance, oversees the School's compliance education and monitoring programs, and ensures that the Departmental compliance plans are consistent with overall policies. The Director of the Yale Medical Group is responsible for ensuring that all aspects of the Medical Billing Compliance Program are effective and executed consistently with these policies. 3. The Medical Billing Compliance Committee. The Medical Billing Compliance Committee ("MBCC") is chaired by the Director of the YMG . Its membership includes the COO, the Director of University Auditing, the Director of Compliance, and representatives from the School's clinical departments, Patient Financial Services, the Office of General Counsel, and the Provost's Office. (Its complete membership is set out at Appendix C.) It meets quarterly to review billing compliance issues and to address policy questions arising in connection with the Billing Compliance Program. It periodically reviews audit findings of internal and external audits. It is charged with reviewing annually the status and achievements of the Plan. 4. The Director of Compliance. The Director of Compliance reports directly to the Director of the Yale Medical Group. The Director of Compliance oversees the daily operations of the Program, monitors each department's compliance efforts, supervises the educational programs offered pursuant to the Program, and generally promotes and advocates the goals of the Program. The Director of Compliance's specific responsibilities include: a. Coordinating compliance functions by (i) attending clinical practice meetings conducted by the PFS; (ii) participating in MBCC meetings; and (iii) conducting quarterly meetings of the Billing Compliance Leaders (described below). b. Establishing and operating educational programs by (i) regularly reviewing and revising all Program-related educational materials (including any website maintained under the Program) in conjunction with the Office of General Counsel, PFS, and the Director of the Yale Medical Group, to reflect changes in billing and coding protocols, and notifying Program Participants of such changes; (ii) disseminating educational materials related to physician billing practices and medical record documentation; (iii) educating and training future Program Participants regarding billing, documentation, and the Billing Compliance Program generally; and (iv) collecting, retaining and reporting educational program test results to the Director of the Yale Medical Group and departmental Billing Compliance Leaders. c. Assisting the clinical departments in fulfilling their billing responsibilities by (i) working with the departments to develop tailored educational resources and facilitating department-based training programs and; (ii) performing independent evaluations of departmental compliance. d. Evaluating YSM compliance efforts by (i) training compliance audit staff to conduct audits of billing and documentation; (ii) monitoring billing, coding and documentation practices used throughout YSM; (iii) conducting independent evaluations of a department if a problem is suspected or an inquiry is received; and (iv) reviewing a sample of medical records and corresponding bills for each department at least annually. e. Investigating complaints of noncompliance received by the YSM Hotline or other means. f. Monitoring proposed employment by determining whether any person or supplier to whom YSM proposes to extend an offer of employment has been sanctioned or excluded from participation in any government programs. g. Preparing the School's Annual Medical Billing Compliance Report, which describes compliance efforts and results achieved during the year. h. Assist with medical billing policy development as needed by the departments, faculty and PFS. 5. Patient Financial Services The Patient Financial Services ("PFS") and the Associate Director of the Yale Medical Group are charged with ensuring accuracy and completeness in the School's billing process and related information systems. In particular, PFS: a. Ensures the availability of up-to-date billing tools, such as encounter forms, through annual review of the forms and revision as necessary. b. Holds regularly scheduled meetings with each clinical department to discuss procedure code and other issues related to the Billing Compliance Program. PFS apprises the Director of Compliance of any departmental compliance issues that arise. c. Distributes materials regarding compliance, such as newsletters received from insurance carriers, to appropriate Program Participants. d. Works with the Director of Compliance on providing training for PFS staff and the administrators of the clinical departments connected with billing. Every two years, PFS will provide a minimum of one hour of medical billing training to PFS employees and to each of the departmental clinical administrators. e. Facilitates responses to routine requests for medical records (i.e., requests made other than in conjunction with an audit). f. Ensures that refunds for payments erroneously made to the School are handled properly and in accordance with the Credit Balance Corrective Action Plan of September 1998 as revised August 2000 and December 2002.. IV. Departmental, Physician and Related Responsibilities 1. Departmental Obligations. Each clinical department is expected to: a. Prepare a written plan addressing compliance efforts on a departmental basis, to be reviewed and approved by the Director of the Yale Medical Group (Appendix A, Compliance Plan, Departmental Implementation Plans) b. Develop departmental expertise in documentation, coding, and billing, and maintain resources to aid providers in achieving accurate billing. c. Appoint one departmental faculty member and one administrator to serve as the department's "Billing Compliance Leaders," with responsibilities described below. d. Appoint a suitable individual or individuals from among its members (or, in small departments and with the approval of the COO, from a cooperating department), to serve as its "Billing Compliance Resource Specialist" (BCRS). The BCRS may be a clinical practice specialist, a coding specialist certified in physician coding, a certified procedural coder, a registered record administrator, or an accredited record technician. Large or high-volume departments may require more than one BCRS. e. In response to requests by the Compliance Department, provide copies of inpatient, outpatient and office medical records for the purpose of facilitating internal and external audits. f. Assist in implementing corrective measures responsive to internal auditing results when deemed appropriate by the Director of the Yale Medical Group (Senior Associate Dean) . g. Timely perform related administrative tasks, including: (i) initiating corrective action on overpayments identified by the department or the Compliance Department including timely notification to PFS and department verification of corrective action; (ii) sending copies of all correspondence with insurance carriers regarding billing or compliance to the Director of Compliance, who monitors all such correspondence; (iii) submitting all draft departmental training materials regarding billing and documentation to the Director of Compliance for review and approval in advance of use; and (iv) notifying the Director of Compliance of any proposed outside affiliation, for review in accordance with the Excluded Persons Policy (Appendix B). h. Support departmental employees in maintaining their status as Certified Procedural Coders, or other credentials that ensure the department has current coding expertise. i. Maintain a record of all its outside affiliations with other health care provider institutions, and the related bills, and provide the Director of Compliance a list detailing any such affiliation before billing for the affiliated party. j. Request a review of contracts with outside affiliations, including YNHH, by the General Counsel's Office, PFS and the Compliance Department as appropriate. 2. Billing Compliance Leaders. The two Billing Compliance Leaders in each clinical department are charged with managing the department's compliance-related tasks and overseeing the department members' compliance with the Program. The Billing Compliance Leaders are expected to work closely with School administrators in fulfilling departmental obligations. A department desiring to oversee the effectiveness of its Compliance Program by a mechanism other than Billing Compliance Leaders must propose its alternative to the COO in writing and should have COO approval before proceeding. The person assigned the billing compliance leader position may be changed every two years or as needed. As a part of their general duties, the Billing Compliance Leaders will: a. Conduct regular intradepartmental discussions of compliance, billing practice, and documentation issues. b. Develop and coordinate departmental educational programs and materials related to the Program. c. Assist as needed with questions raised by the Compliance Department relating to compliance audits and other compliance activity of the department d. Conduct departmental follow-up meetings with faculty and staff to discuss the results of Compliance Program monitoring. e. Attend quarterly meetings with the Director of Compliance and Billing Compliance Leaders from other departments. f. Review and revise as necessary the departmental compliance plans g. Participate in and approve annual encounter form updates h. Assist with ensuring 100% compliance with the training requirement for their department and as needed with the development and coordination of departmental training programs. 3. Billing Compliance Resource Specialist. The Billing Compliance Resource Specialist will develop expertise in billing and coding protocols applicable to the department operations, and serve as a compliance resource for others in the department. 4. Particular Obligations of Physicians and Other Healthcare Providers. All physicians and other health care providers must assume accountability for their own medical record documentation and the corresponding diagnosis and procedure codes that appear on bills they submit for reimbursement. They must document medical records and assign billing codes in accordance with government regulations and in a timely and accurate manner. 5. Physician Educational Requirement. Annually , all billing physicians covered by the Program must complete one hour of medical billing compliance training. This requirement may be met in various ways. The first option is for physicians to participate in the Teaching Regulations Training Module published at the Yale Teaching Physicians website (http://learn.med.yale.edu/cms/caslogin.asp). Physicians may also meet the training requirement by electing alternate programs offered by the Compliance Department such as seminars, video training, audit selection, or other programs. New faculty must complete the Teaching Regulations Training Module and pass the accompanying test within a reasonable time after beginning employment at the School. Billing privileges may be suspended if a new faculty member does not timely comply with this requirement. The requirement may also be met by new faculty participating in a training session with the Compliance Department. A list of all participants and associated training activity will be maintained by the Director of Compliance, who will report the results to the Director of the Yale Medical Group and the relevant Billing Compliance Leaders. V. Obligation of all Program Participants All Program Participants must: (1) familiarize themselves with the Program and with applicable coding and documentation requirements; (2) attend all mandatory training sessions; (3) keep abreast of changes in the Program and coding and documentation procedures; (4) bill correctly and in good faith, and document adequately; and (5) promptly refund payments received in error. VI. Compliance Guidelines Coding and Documenting Bills The individual health care provider who provides a service bears the primary responsibility for accurately assigning procedure and diagnosis codes and adequately documenting the services rendered that they in good faith believe correspond to the services they render that are documented in the medical record. YSM abides by medical billing standards issued by the Center for Medicare and Medicaid Services ("CMS"), and, as appropriate, the American Medical Association ("AMA") in its book of Current Procedural Terminology (the "CPT" book) and the CMS Teaching Physician Guidelines. Program Participants are expected to familiarize themselves with the CMS/AMA standards. In case of a dispute among Program Participants, the Director of the Yale Medical Group is responsible for resolving the issue. Program Participants are expected to bring possible coding errors to the attention of the relevant provider. Entering Charges into the YSM- or Related Computerized Billing Systems A Program Participant must never enter a charge, or submit or process a claim or bill that he or she knows to contain any inaccurate information concerning the service provided, the charges, the identity of the provider, the date of service, the place or service, or the identity of the patient. Except as provided below, bills generated by Program Participants must be entered into the YSM computerized billing system and issued by the Patient Financial Services ("PFS"). Bills may be prepared by and issued through other than by PFS with the written approval of the School's Chief Operating Officer and the Director of the Yale Medical Group. To obtain approval for an alternative arrangement, the requesting Department should document its proposed arrangement, its past practice (if relevant), and its reasons for the departure from standard practice, and submit its request in writing to the COO and the Director of the Yale Medical Group. Managing Uncertainty in Billing When you are uncertain about how to bill for a particular service or what code to use, you must resolve that concern to the best of your ability before submitting a bill. Address your question to the following people in the following order, to the extent feasible: First, to your immediate supervisor or clinical administrator, who may consult with your Department's Billing Compliance Resource Specialist, Billing Compliance Leaders, or other knowledgeable Departmental billing personnel. Second, to PFS's Associate Director, Patient Accounts. Third, to the Director of Compliance. If the question has still not been resolved to your satisfaction, you may contact either the Executive Director of PFS, the Director of the Yale Medical Group, the Dean, or the University's Office of General Counsel or the Medical Billing Hotline VII. Hiring: The Excluded Persons Policy The School is not allowed to bill for services rendered by certain "excluded persons" individuals who have been sanctioned by the United States Government or excluded from participation in federal programs. The School abides by federal requirements pertaining to the employment of individuals who have been sanctioned by the United States Government or excluded from participation in federal programs. 1. Excluded Persons Policy. The School will follow the Excluded Persons Policy set forth at Appendix B regarding its relationship with any individual who has been sanctioned or excluded by the United States Government from participating in federal programs. 2. Credentialing Office Review. When the credentialing process is initiated, the Credentialing Office will request that the Compliance Office confirm that the individual's name does not appear on the CMS/OIG excluded persons and cumulative sanctions lists. The Credentialing Office will report the name of the individual hired, the hiring department, and the effective date of employment to the Compliance Office promptly after receiving notice of the hire. The Excluded Persons Procedure can be found in its entirety at: http://info.med.yale.edu/ymg/comply/alert/exdebar.html VIII. Education Program Working through the Departments and the Director of Compliance, the YSM will strive to educate all Program Participants with respect to obligations imposed by the Compliance Program and related laws, regulations and protocols. The YSM intends that every employee involved in professional fee billing shall at a minimum receive the equivalent of one hour of compliance training every year. 1. General Policies. a. Education and training may occur through a variety of media, including e-mail, newsletters, memoranda, presentations, online training, and formal programs. b. Education may be provided centrally by the Compliance Department or at the Department or section level. c. The Director of Compliance will ensure that Program Participants receive timely updates on changes in billing and coding regulations or protocols. d. The YSM will regularly review and revise all educational materials to reflect changes in billing and coding protocols. e. Participation in certain educational and training programs will be made available to Program Participants. 2. Oversight by the Director of Compliance. The Director of Compliance will oversee YSM and departmental educational programs regarding compliance and assure consistency in their content insofar as possible, and will review all training materials developed by the departments. The Director of Compliance will inform the faculty and staff of changes in documentation requirements and teaching physician guidelines, and will advise of incorrect billing practices and areas of abuse targeted by the Department of Health and Human Services Office of the Inspector General ("DHHS/OIG") or other external enforcement agencies. With respect to these tasks, the Director of Compliance will collaborate with other key administrators, including the Director of the Yale Medical Group, the General Counsel, the Director of University Auditing, the Executive Director of PFS, and departmental administrative leadership. 3. Training by the Patient Financial Services. The Patient Financial Services will annually provide PFS staff and department clinical administrators at least one hour of compliance training with respect to billing and the Billing Compliance Program at least every two years. 4. Departmental Education. With the assistance of the Director of Compliance, the clinical departments may develop and operate educational and training programs focusing on particular coding and other issues relevant to their specific clinical practices. Departments should use the results of their own compliance monitoring efforts in their educational programs. The Director of Compliance will monitor the effectiveness and consistency of such programs. IX. AUDITS External Audits. a. Audit notice. The federal government and other third party payors periodically audit the bills of health care providers. Any individual at YSM who receives notice of such an audit shall immediately advise and provide the Director of Compliance with a complete copy of the notice. The Director of Compliance will notify the Executive Director of PFS and the Director of the Yale Medical Group. The Executive Director of PFS and/or Director of the Yale Medical Group will thereafter promptly notify the Medical Director, the COO, the General Counsel, the Chairman of the Department involved, and the Director of University Auditing of the audit notice. All contact with the entity initiating the audit will be coordinated by the Director of Compliance. b. Requests for medical records. An audit notice may contain a request for medical records. Multiple requests for medical records generally indicates that an audit is underway even absent an audit notice. Requests for medical records may be received directly by departments or the physician being audited. In these situations, a copy of the request should be promptly sent to the Director of Compliance by the department or physician. In order for the Director of Compliance to respond to such requests for medical records, the department will promptly gather and collate two copies of each of the medical records requested, retain one, and provide one to the Director of Compliance. The Director of Compliance will conduct a preliminary review of the requested medical records and associated bills and report his or her findings to the audit response team. c. Response to external audit. Under the management of the Director of Compliance and with input from the Executive Director of PFS, the Director of the YMG , the General Counsel's Office, the Office of University Auditing, and an appropriate Departmental representative the School's response to the audit will be formulated. Possible actions include identifying potential billing problems, communicating with the physician being audited, and communicating with the party conducting the audit. d. Completed audits. The Director of Compliance will review any correspondence related to an audit, including any document reflecting the results of the audit. The Director of Compliance and Billing Compliance Leaders will conduct any appropriate follow-up to a completed audit with the health care providers and staff involved. Generic material or information generated by an audit may be incorporated into educational materials and activity. e. Records related to an external audit. The Compliance department will maintain copies of the medical records produced in connection with an external audit for at least seven years after the close of an audit. f. Summary of audits. The Director of Compliance will provide quarterly, annual and cumulative summaries of the audits conducted at the School to the Director of the Yale Medical Group. The Director of the Yale Medical Group will provide a summary of audit results to the MBCC at its meetings. 2. Internal Audits The Director of Compliance and associated compliance staff will conduct regular internal reviews of billing and documentation activity at the School. The Director of Compliance will prepare an annual Audit Plan outlining the internal audits to be conducted. The audit plan will be based on: Areas targeted in the Office of Inspector General's Work Plan for the current year The results of last year's compliance audits Individual physicians who request a compliance audit Areas identified by the local Medicare carrier through its' newsletter or other media New physicians Teaching Physician Quiz Scores Randomly selected services Office of the Inspector General's Chief Financial Officer's audit results The audit plan will be prioritized and will be a flexible document allowing for audits to be added, revised or deleted in response to shifting priorities. The Compliance Department will conduct audits using standardized procedures and audit tools to ensure quality and consistency of audit results. The Director of Compliance will respond to the results of an internal departmental audit by addressing comments, when appropriate, to the healthcare provider, the Billing Compliance Leaders, and, if necessary, the department Chair. The Director of Compliance will provide summary results of the internal audit to the Dean, the COO, the Director of the Yale Medical Group, the General Counsel and the Director of University Auditing. The Compliance Department must give health care providers prompt feedback on their individual performances to allow for timely correction of improper practices X. Service of Process; Subpoenas Any School employee who receives legal process, such as a summons or subpoena, must immediately notify the General Counsel (phone: 203/432-4949) and provide the General Counsel a copy thereof. If the legal process received involves medical billing and compliance, the School employee must also notify the Executive Director of PFS or the Director of the Yale Medical Group, who will in turn notify the Director of University Auditing, the COO, and the Director of Compliance. The School employee must thereafter forward all relevant documents to the General Counsel, in accordance with instructions from that office. XI. Record Retention System Connecticut law mandates that the School retain certain records for prescribed lengths of time pertaining to the delivery of medical services. The University also desires to maintain certain records demonstrating its commitment to compliance. For these reasons, the School has instituted the following record retention policy, which applies to paper records and to those maintained on computer, magnetic tape, or in another electronic data processing storage medium. All such records should be amenable to ready retrieval upon demand. 1. Legal Requirements. Connecticut law requires that records are maintained as follows (Conn. Agencies Regs. ss 19a-14-41 through 19a-14-43): a. Retain all parts of a medical record for seven (7) years from the date of last treatment, or for three (3) years after the death of a patient. b. Retain pathology slides, EEG and ECG tracings for seven (7) years, but if an ECG is taken and the results are unchanged, then only the most recent result need be retained. Reports regarding each of these slides or tracings must be retained for the life of the medical record. c. Retain positive (abnormal) laboratory and PKU reports for at least five (5) years. (Under the regulations, negative reports need not be retained.) d. Retain x-ray films for three (3) years. e. If a claim of malpractice, unprofessional conduct, or negligence with respect to a patient has been made, whether or not litigation has actually commenced, retain all records regarding that patient until the matter is finally resolved. f. "A consulting health care provider should retain records if they are sent to the referring provider, who must retain them." (Note: YMG requires the consulting health care provider to retain a signed copy of the letter sent to the referring provider in the patient's medical record to support any billings that may have been generated. g. An initial health care provider is not required to retain records that he or she sends to a new primary provider upon a patient's written request. (Note: It is recommended that a copy of the records be kept to support any billings that may have been generated.) 2. Additional Requirements. In addition, the School has instituted the following policies regarding the retention of records. a. Retention of affiliation records. The School requires that clinical Departments maintain copies of records related to their affiliations with outside institutions, including related billing records, for seven (7) years. b. Document destruction policy. Disposal and destruction of documents, including by shredding, must be done in accordance with any applicable departmental or School policy. Documents containing social security numbers, medical diagnoses, and insurance policies, should be destroyed by shredding. All record destruction procedures must be amenable to being halted rapidly, in response (for example) to service of legal process. c. Privacy and security. Record creators, record users and record keepers at the School must use their best efforts to ensure the privacy and security of medical records and in accordance with the relevant federal and state guidelines. d. Privileged documents. All privileged documents must be segregated and clearly marked. For purposes of this requirement, "privileged documents" means any document covered by the physician-patient, therapist-patient, attorney-client, attorney work product, or other legal privilege or doctrine protecting it from production during legal proceedings. 3. Retention of Insurance Carrier and Government Correspondence. All correspondence that relates to billing issues between any insurance carrier and the School or any of its constituent parts (including all individuals employed by the School)) must be retained for seven (7) years. Copies of all such correspondence which pertain to medical billing issues should be sent by the School employee to the Director of Compliance and to PFS. Correspondence that must be retained includes, but is not limited to: letters received in response to a request for a policy clarification; billing instructions; fee schedules; and statements of policy or policy changes. For purposes of this section, "insurance carrier" means a Medicare carrier or intermediary, a private insurer, or any state or government agency. 4. Retention of Documents Connected with External Audits. The Compliance Department will maintain a copy of all medical records and correspondence related to an external audit in a secure location for seven (7) years. Note: If any Department or clinical activity is subject to more stringent medical record retention requirements than the requirements listed in this policy, the more stringent requirements apply. These more stringent requirements may include rules imposed by the federal government or an accrediting body. XII. Reporting Compliance Issues 1. General Principles. Each Program Participant must comply with the Program and is expected to report instances of suspected non-compliance to School or University officials, as described below. Employees who in good faith report possible compliance issues will not be subject to retaliation or harassment for the report. Any concerns regarding apparent or possible retaliation or harassment should be addressed to the COO and the General Counsel. 2. Reporting System for Potential Compliance Issues. The School will operate a confidential reporting system for potential compliance problems that is accessible to all faculty, staff, and other individuals. Individuals may make such reports either via a telephonic hotline, orally, or in writing to the Director of Compliance, departmental management staff, the Office of General Counsel, or the Director of University Auditing. All School employees will be advised of the hotline reporting system and the opportunity to report billing compliance concerns in writing. All inquiries, reports, or complaints must promptly documented and transmitted to the Director of Compliance and the Director of University Auditing. The Director of University Auditing will maintain the hotline reporting system and serve as liaison with any provider of a hotline service that may be retained. Upon the complainant's request, his or her anonymity will be preserved to the extent practicable. 3. Logs of Reports. The Director of Compliance will maintain a confidential log of compliance concerns reported directly to him or her and/or the Director of the YMG , recording the issue complained of, the departments or divisions affected, the status of the investigation, if any, and any issues remaining to be resolved. The log will also reflect the source of the complaint, and will maintain the anonymity of the complainant to the extent practicable. Access to the log will be limited to the Director of the Yale Medical Group, the COO, General Counsel, Director of University Audit, and other individuals as determined by the Director of Compliance as needing to have access in order to perform their duties. All documents reflecting an allegation regarding medical billing compliance will be maintained in a confidential manner. The Director of Compliance will keep the Director of YMG apprised of all open compliance concerns during their weekly meetings. The Director of University Auditing will maintain a confidential hotline log reflecting any billing complaints received by the hotline and the results of the investigation of those complaints. The Director of Compliance will forward on at least an annual basis a copy of the report log to the COO, Director of the Yale Medical Group and the General Counsel. 4. Response to Allegations, Inquiries, or Complaints. The Director of University Auditing will contact the COO, Director of the Yale Medical Group and the General Counsel to determine a suitable response to particular allegations, inquiries, or complaints. In consultation with the General Counsel, the Director of University Auditing will determine whether alleged wrongdoing appears to amount to a violation of state or federal law, regulation or policy, whether it conflicts with the School's Medical Billing Compliance Program, poses a risk to the general public, or could put the School at risk of economic or reputational injury. On the basis of that determination, and in further consultation with the COO, General Counsel, Director of the Yale Medical Group, and the Director of Compliance, the Director of University Auditing will designate a University official to investigate the allegation. 5. Summary Reports of Allegations and Investigations. The Director of Compliance will include in the quarterly report to the COO and the Director of the Yale Medical Group a summary of all compliance-related allegations, inquiries or complaints received and investigations conducted during the quarter. The Director of University Auditing and the Director of Compliance will disclose the fact and substance of any allegations, inquiries and reports only to the COO, Director of the Yale Medical Group, members of the Medical Billing Compliance Committee, the General Counsel, and their respective representatives having a need to know. The Director of University Auditing will closely monitor the progress of any investigation. XIII. Investigating Compliance Issues It is the School's policy to investigate allegations of non-compliance within a reasonable time after the allegation is received. 1. Investigatory Authority. If the Director of the Yale Medical Group determines that there is reasonable cause to believe that a compliance issue may exist, an inquiry will be undertaken. The Director of University Auditing will assign responsibility for investigating a hotline report to University officials on a case by case basis, and in consultation with other administration officials. The General Counsel will aid in the determination whether the School should retain an external consultant to conduct the investigation. The Director of University Auditing will timely advise the Director of Compliance of the identity of the investigator assigned to inquire into complaints received (if the Director of Compliance is not the investigator). The Director of University Auditing is authorized to investigate any function or individual upon his or her own initiative, reasonably exercised, and nothing in the Program limits that authority. 2. Investigative Process. At the start of an investigation, the General Counsel, the Director of University Auditing, COO, the Director of the Yale Medical Group, and the Director of Compliance will discuss its nature, determine an appropriate course of action including who will investigate the complaint, and set a timetable for completion. Investigations will be conducted as confidentially as possible under the circumstances. Investigators and their assistants will respect the privacy concerns of both complainant and the subject or subjects of the complaint. Records related to the investigation and to the reports of wrongdoing will be preserved in accordance with law and so as to assure their protection under the attorney-client privilege and attorney-work product doctrine, as applicable. 3. Findings. The investigator will provide interim reports, as requested, and written investigative findings to the Director of the Yale Medical Group, the General Counsel, the COO, the Dean, the Director of University Auditing, and the Director of Compliance. XIV. Corrective Action Whenever a compliance issue has been identified, the School will take action to remedy the problem, mitigate the harm done, and prevent a recurrence. The type of corrective action instituted will depend on the nature and gravity of the noncompliance found. 1. Authority The Director of the YMG in consultation with the Dean has final authority for directing corrective action in response to a finding of noncompliance. In formulating an appropriate course of corrective action, the Director of the YMG will consult with the COO, Executive Director of PFS, the Office of General Counsel, the Director of Compliance, and the Director of University Auditing, (and may consult with the COO and the Dean). The corrective action plan adopted will be set forth in writing. . 2. Process. Corrective actions will be set forth in writing and delivered to the individuals required to comply. Corrective actions will be designed to address provider-specific issues and to ensure that similar issues in the billing process are addressed in other departments. 3. Follow-up. Once corrective action has been taken, its effectiveness will be evaluated by the Director of Compliance as needed, or within a reasonable time after the corrective action has been completed. The Director of Compliance will discuss the findings of the evaluation with the health care provider or other involved individual, the applicable Billing Compliance Leaders, and the Director of the YMG . The Director of Compliance and the Director of the YMG will jointly determine whether any further corrective action is necessary or appropriate. XV. Discipline and Enforcement 1. General Policies. Compliance with the Plan is an essential element of the job responsibilities of all Program Participants. Program Participants who fail to adhere to the Plan may face disciplinary action, and their professional evaluations may reflect these failures. The School has a policy of progressive discipline and sanctions for infractions committed by an employee, including non-compliance with the Plan; in instances of gross misconduct, however, immediate disciplinary action, up to and including termination, may result. Whether the prohibited conduct was undertaken recklessly or willfully will be weighed heavily in administering discipline and sanctions. 2. Disciplinary Action. Corrective action for non-compliance, determined by the Director of the Yale Medical Group, may include a recommendation that the Dean impose a sanction or disciplinary action against a non-complying individual. The Dean has delegated his authority to effect discipline for non-compliance with the Program to the COO. Individuals who have demonstrated a propensity toward behavior that raises compliance concerns may be restricted from billing. Other possible disciplines include, for example: requiring attendance at additional training at the expense of the individual; having billing activity monitored regularly by an external billing expert, retained at the expense of the individual involved; reprimand; probation; and suspension or termination of employment. 3. Notification. Through publication and dissemination of this Manual, the School is advising all faculty, staff, other Program Participants, and related participants of the Billing Compliance Program and its requirements, the importance of adhering to the Program as a material condition of their employment, and the possible consequences of non-compliance, including immediate termination of employment. Program Participants will be notified of subsequent significant revisions to the Compliance Manual. 4. Consequences of Non-compliance for Related Participants. Non-compliance by related participants (entities that bill for services rendered by the School or perform services for which the School bills) may result in (a) termination of the person's or entity's agreement with the School; (b) a demand for reimbursement for any losses or damages resulting or required from the violation; or (c) other responsive actions, including referral to enforcement agencies, as permitted or required by law. XVI. Annual Review and Report 1. External Monitoring. The University may retain qualified external experts to review all or part of the Program, identify its strengths and weaknesses, make recommendations, and assist in implementing modifications to the Program. 2. Annual Compliance Audit. On an as needed basis, the Director of University Auditing will conduct an audit of the University's current medical billing operation to determine whether there are sufficient controls in place to assure that federal health insurance programs and other insurers are billed appropriately for services rendered. He or she will submit this report to the Audit Committee on or before July 15. 3. Annual Reporting. Annually, on or before each July 31, the Director of Compliance will prepare a report on the effectiveness of the Program in the preceding financial year and will make recommendations for improvement as needed. The Annual Medical Billing Compliance Report will also include at least the following elements: a summary of general compliance activity undertaken during the preceding year, including any changes made to the Compliance Plan; a copy of the Hotline log for the preceding year; a copy of the audit report if conducted by the Department of University Auditing; a description of actions taken to ensure the effectiveness of the training and education efforts; and a summary of actions taken to ensure compliance with the University's policy on dealing with excluded persons. The Director of Compliance will distribute the Annual Medical Billing Compliance Report to the Director of the Yale Medical Group, the Department Chairs, the General Counsel, the Director of University Auditing, the Dean, the COO, the Medical Billing Compliance Committee and to others with an interest in compliance, for their comments and suggestions for revisions to the Program. The Director of the Yale Medical Group will transmit the Annual Report to the University Audit Committee that is chaired by the Provost and the Audit Committee of the Yale Corporation. GLOSSARY AMA American Medical Association BCL Billing Compliance Leader BCRS Billing Compliance Resource Specialist CPT Current Procedural Terminology CPC Certified Procedural Coder CMS Center for Medicare and Medicaid Services DHHS U.S. Department of Health and Human Services GME Graduate Medical Education HCFA Health Care Financing Agency, a United States Government Agency (now CMS) MBCC Medical Billing Compliance Committee OIG Office of Inspector General PFS Patient Financial Services YSM Yale School of Medicine YMG Yale Medical Group APPENDIX A YALE UNIVERSITY SCHOOL OF MEDICINE MEDICAL BILLING COMPLIANCE PLAN Introduction The Yale University (the "University") has an ongoing commitment to ensuring that its activity are conducted in accordance with applicable law and sound and ethical business practice. The University also has a strong interest in making certain that its faculty and employees are fully informed about applicable laws and regulations so that they do not inadvertently engage in conduct that may raise compliance issues. Of particular concern, given the fact that many medical school faculty engage in clinical practice, are legal requirements relating to professional fee billing. Compliance in this area is challenging because the regulatory requirements governing professional fee reimbursement are complex and changing. To further its commitment to compliance and to protect its employees, the University has decided to formalize its compliance plan to address professional fee reimbursement. The compliance plan has the following key features: Designation of University officials responsible for directing the effort to enhance compliance, including implementation of the Plan; Incorporation of standards and policies that guide University personnel and others involved with the billing process with regard to professional fee billing; Development of compliance initiatives at the Department level; Coordinated training of clinical staff and billing personnel concerning applicable billing requirements and University policies; A uniform mechanism for employees to raise questions and receive appropriate guidance concerning professional fee billing; Regular chart and billing reviews to assess compliance, to identify issues requiring further education, and to identify potential problems; A process for employees to report possible compliance issues and for such reports to be fully and independently reviewed; Formulation of corrective act ion plans to address any compliance problems that are identified; and Regular reviews of the overall compliance effort to ensure that billing practices reflect current requirements and that other adjustments are made to improve the program. The compliance program described in this document is intended to establish a framework for legal compliance by the University and its employees. It is not intended to set forth all of the substantive programs and practices of the university that are designed to achieve compliance. The University already maintains various compliance practices and those practices continue to be a part of its overall compliance efforts. Scope The Plan applies to billing for clinical activity by Yale physician faculty that takes place within the scope of their employment at the Yale Medical Group (YMG). It includes the activity of the YMG as well as any situations where some other entity or group handles YMG billing. The Plan applies to all faculty, housestaff, fellows, and any other persons who are involved in YMG billing. Administrative Responsibility Primary responsibility for implementing and managing the University's medical billing compliance effort shall be assigned to the Director of the Yale Medical Group . The position of Director of Compliance will be created and will report to the Director of the YMG . The Director of Compliance will, with the oversight of the Director of the YMG and the assistance of University counsel where appropriate, perform the following activity: 1. Assist in the review, revision, and formulation of appropriate policies to guide billing of professional fees by organizations that bill for services provided by University medical faculty; 2. Work with Departments and faculty to develop plans for implementing University policies on billing; 3. Assist in developing and delivering educational and training programs; 4. Work with Departments and faculty to develop and/or enhance billing expertise and to facilitate Department based training programs; 5. Coordinate reviews of medical charts and associated billings; and 6. Provide other assistance as directed by the Director of the YMG The Director of Compliance shall work closely with representatives of the Departments and any entities or individuals who handle professional fee billing for the University's faculty physicians to foster and enhance compliance with all applicable billing requirements. Policy Guidelines The policy of Yale University is to bill only for professional services provided. The University recognizes that special billing requirements may apply to certain governmentsponsored programs or to other providers; any such requirements must be followed. In selecting codes to describe services rendered, University physicians, other health professionals, and billing personnel are to select codes that they believe, in good faith, correspond to services actually rendered, as documented in the medical record. University clinicians, other health professionals, and billing personnel have a collective responsibility to be knowledgeable about the meaning of the codes applicable to their area of practice, including relevant directives from billing authorities. The University further recognizes the importance of maintaining accurate patient accounts in accordance with applicable requirements. University Physicians, other health professionals, and billing personnel should never submit a claim that is known to contain inaccurate information concerning the service provided, the charges, the identity of the provider, the date of service, the place of service, or the identity of the patient. Payments that are received in error will be refunded. When in doubt about how to bill a particular service, including the proper code to use, no claim should be submitted until appropriate guidance is obtained from departmental compliance leaders or from the Director of Compliance. The resolution of any such billing questions should be documented in writing. It is the responsibility of the billing physician or other health professional to ensure that appropriate documentation supports the bill being submitted. To guide physicians, other health professionals and billing personnel in meeting these objectives, the Director of the Yale Medical Group shall, with the assistance of legal counsel, review existing policy statements, revise those statements as necessary, and develop any additional statements that seem advisable. University policies concerning billing, as those policies may be changed periodically, should be considered an integral part of this Plan. A copy of the University's policy in dealing with excluded persons is attached to the Plan and incorporated herein. Departmental Implementation Plans Each clinical department shall appoint a faculty member and an administrator to serve as the compliance leaders for departmental billing activity. The departmental compliance leaders will coordinate departmental compliance activity with t he Director of the YMG and the Director of Compliance. There should be regular contact with the compliance leaders about matters of common interest. Each clinical department must prepare a plan to address compliance efforts on a departmental basis. Large departments may also choose to develop plans for specific divisions. Before becoming effective, such plans should be reviewed by the Director of the YMG to ensure consistency with overall policies. If there are concerns about the content of any departmental plan, the Director of the YMG should consult with the Department Chair to explore whether the plan can be modified through mutual agreement. If such consultations fail to resolve the concerns, the Director of the YMG may recommend that the Dean modify the department's implementation plan. The department (or divisional) implementation plans shall, at a minimum, include the following features: 1. written policies and procedures for billing activity undertaken by departmental personnel, including any specialty specific standards that may be relevant to regulatory compliance; 2. educational and training programs to address billing issues of particular importance to the department; 3. a program for ensuring, and documenting, that all new department personnel, including faculty and housestaff, receive training with regard to proper billing; 4. a program for routine "spot checks" of departmental billing (or proposed billing) to review compliance, with the results of such reviews being reported to the department's compliance leader and to the Director of Compliance; 5. a system that tracks billing or compliance issues that have been raised within the Department and the resolution of those issues; and 6. an annual review of the existing compliance plan in order to identify the need for changes and to identify specific compliance objectives during the succeeding year. Departments or Divisions should advise the Director of the YMG prior to engaging any outside billing consultant and should provide a copy of any reports prepared by such consultants. Education and Training The Director of Compliance shall be responsible for ensuring that the University policies concerning billing are disseminated to by faculty and billing personnel. To accomplish that objective, the Director of Compliance will work with the Director of the YMG, the Departments, and any other individuals or entities that handle professional fee billing for University faculty to ensure that there is a systematic and ongoing training program that enhances and maintains awareness of billing policies among existing staff and that introduces new personnel to University billing policies. All training materials directed to billing issues will be submitted to the Director of Compliance for review. All physicians and billing personnel should participate in training about billing issues and the Director of Compliance, working in concert with the Departments, should develop a system to document that such training has occurred. Moreover, if a concern develops about particular billing issues, the Director of the YMG may direct that physicians and/or billing personnel attend training sessions on particular issues. The training materials will identify the specific people who should be contacted by physicians or billing personnel about billing questions. It is the University's intent that every employee involved with professional fee billing receive the equivalent of one hour training each year. Monitoring Under the supervision of the Director of Compliance, a sample of medical records and corresponding bills for each department and division will be periodically reviewed for compliance with the University's billing policies and with legal requirements. The Director of Compliance may choose to review proposed charges that have not yet been submitted for payment. Each department shall be reviewed at least annually, but the Director of Compliance may require more frequent reviews. The results of such reviews will be reported to the Director of the YMG, the audited healthcare provider and to the department's compliance leaders. Moreover, the Director of the YMG and the COO may, after consultation with legal counsel for the University, engage an external billing expert to review records for a particular department or drawn from a cross-section of departments. If any of these reviews identify instances of possible non-compliance, the Compliance Officer shall report that fact to the Director of the YMG, the Chair for the department whose billings are at issue, the COO, the director of University Audit and to Office of the General Counsel. In consultation with legal counsel, the Director of the YMGshall review the situation to determine whether there appears to have been any activity inconsistent with university policies. Reporting Compliance Issues As a general matter, questions about billing issues should be presented initially to one of the departmental compliance leaders. But the training materials will also inform University employees and billing personnel that they may report to the Director of the YMG, the Director of Compliance, or to the Office of the General Counsel any activity that they believe to be inconsistent with University policies or legal requirements regarding billing. The materials will explain how those persons can be contacted. The Director of Compliance should use innovative communication methods, including computer communications, to assure that the elements of this compliance program are well understood by affected employees. Employees who report in good faith possible compliance issues should not be subjected to retaliation or harassment as a result of the report. Concerns about possible retaliation or harassment should be reported to the Director of the YMG. The Director of Compliance will maintain a log of compliance concerns that are reported directly to the Director of the Yale Medical Group. This log will record the issue, the departments or divisions affected and the resolution. As concerns are reported, they will be reported to the Director of the YMG and annually to the University's internal auditor and the Medical Billing Compliance Committee. The log reports should note any issues that remain open. This log should be treated as a confidential document and access should be limited to those persons at the University who have responsibility for compliance matters. Confidential Hotline The Director of Compliance will establish a telephone "Hotline" to permit compliance issues to be reported on a confidential basis. The Hotline will be available 24 hours a day and the Director of Compliance will ensure that training and educational materials include information on how the Hotline can be accessed. The University shall maintain a log reflecting any billing complaints received via the Hotline and the results of the investigation of those complaints. All billing complaints will be investigated unless the information provided by the Hotline contains insufficient information to permit a meaningful investigation. In such instances, the log will explain why no investigation was undertaken. Investigating Compliance Issue Whenever conduct that may be inconsistent with a billing policy or requirement is reported to the Director of Compliance, the matter should be referred to the Director of the YMG. If the Director of the YMG determines that there is reasonable cause to believe that a compliance issue may exist, an inquiry into the matter will be undertaken with appropriate assistance from the Office of the General Counsel and the University's Internal Auditor. Responsibility for conducting the review will be decided on a case-bycase basis. The results of the inquiry will be made available to the Director of the YMG, to the Office of the General Counsel and to the Internal Auditor. University employees should cooperate fully with any inquiries undertaken by the Director of the YMG , the Office of the General Counsel, the Office of the Chief Operating Officer, or the University's Internal Auditor. To the extent practical and appropriate, efforts should be made to maintain the confidentiality of such inquiries and the information gathered. Nothing in this Plan shall limit the authority of the University's Internal Auditor to conduct investigations or to act on his or her own initiative. Corrective Action Plans Whenever a compliance issue has been identified, through monitoring reporting of possible issues, investigations, or otherwise, the Director of the YMG shall have the responsibility and authority to take or direct appropriate action to address that issue. The corrective action will be set forth in writing. In developing a corrective action plan, the Director of the YMG should obtain advice and guidance from the University's legal counsel. There should also be consultation with the Director of Compliance and with appropriate clinical and billing personnel. Information about the corrective action plans should be provided to the Dean, the Office of the Chief Operating Officer, the Office of General Counsel and to the Internal Auditor. Corrective action should be designed to ensure not only that the specific issue is addressed but also that similar problems do not occur in other areas or departments. Corrective action may require that billing be handled in a designated way, billing responsibility be reassigned, that certain training take place, that restrictions be imposed on billing by physicians or other health professionals, that repayment be made, or that the matter be disclosed externally. If it appears that certain individuals have exhibited a propensity to engage in practices that raise compliance concerns, the action plan should identify actions that will be taken to prevent such individuals from exercising substantial discretion with regard to billing. Corrective action may include recommendations that impose a sanction or disciplinary action. Moreover, if the Director of the YMG determines that any non-compliance has been willful, the Dean should be informed of that finding. University employees who have engaged in willful misconduct will be subject to disciplinary action, up to and including termination in appropriate cases, in accordance with School and University policies and procedures. Compliance Audit On an as needed basis, the University's Department of Internal Audit shall conduct an audit of the University's current professional billing operation including a review of billing policies, procedures and practices. The purpose of the audit, which should include such probe samples as the Department of Internal Audit considers advisable, is to ascertain whether the billing process has reasonable controls in place to assure that providers, including Federal health insurance programs, are billed appropriately for services rendered as claimed. A written report describing the results of the audit should be prepared. Annual Report On or before July 31st, the Director of Compliance should prepare and distribute a report describing the efforts during the preceding year. The report shall include the following elements: 1. A summary of the general compliance activity undertaken during the preceding financial year, including any changes made to the Compliance Plan; 2. A copy of the Hotline log for the preceding financial year; 3. A copy of the preceding financial year's Compliance Audit if such an audit was undertaken by the Department of Internal Audit; 4. A description of actions taken to ensure the effectiveness of the training and education efforts; 5. A summary of actions to ensure compliance with the University's policy on dealing with excluded persons; and, 6.Recommendations for changes in the Plan that might improve the effectiveness of the University's compliance effort . Revisions to this Plan This Compliance Plan is intended to be flexible and readily adaptable to changes in regulatory requirements and in health care systems as a whole. The Plan should be regularly reviewed to assess whether it is working. The plan should be changed as experience shows that certain approach is not effective or suggests a better alternative. To facilitate appropriate revisions to the Plan, the Director of Compliance should prepare a report, at least annually, that describes the general compliance efforts that have been undertaken during the preceding year and that identifies any changes that might be made to improve compliance. Circulate the annual report to the Director of the YMG, the Department Chairs, the University's General Counsel or her designee, to the University Internal Auditor, and to others with an interest in compliance for their comments about possible revisions to the Plan. 1 The University intends that this compliance plan embrace all elements of an "effective program to prevent and detect violations of law," as identified in Commentary 3(K) to 8A1.2 of the Federal Sentencing Guidelines. In addition, the plan has incorporated the objectives and components of the Committee of Sponsoring Organizations (COSO), Internal Control-Integrated Framework; comprising five major accounting groups. Appendix B Excluded Persons Policy The University confirms the importance of compliance with 42 U.S.C. 1320a-7a(a)(6), which imposes penalties for "arrang[ing] or contract[ing] (by employment or otherwise) with an individual or entity that the person knows or should know is excluded from participation in a Federal Health Care Program... for the provision of items or services for which payment may be made under such a program." Accordingly, prior to employing or contracting with any provider for whom the University intends to submit bills to a Federal health care program, the University will take appropriate steps to confirm that the provider has not been excluded. Those steps will include checking the provider's name against the HHS/OIG Cumulative Sanctions Report and the GSA Debarred Bidders List. The University's Compliance Officer will provide training to employees with responsibility for personnel functions about how to access those lists. If the University learns that a prospective provider (either as an employer or contractor) is excluded, the University will not hire or use that provider. . If the University learns that any of its current providers (either as employees or contractors) has been proposed for exclusion or excluded, it will remove such providers from any involvement in or responsibility for Federal health insurance programs until such time that the University has confirmed that such provider is not proposed for exclusion or excluded. APPENDIX C Medical Billing Compliance Committee: Membership List Cynthia Walker Deputy Dean for Finance and Administration James Brink, M.D. Chair Department of Diagnostic Radiology Jack Elias , M.D. Chair Department of Internal Medicine Marianne Dess-Santoro Executive Director of Patient Financial Services Ronald J. Vender, M.D. Chief Medical Officer, Yale Medical Group Judy Harris Director of Compliance, Yale Medical Group David J. Leffell, M.D. Director of the Yale Medical Group Jonathan Tamir, M.D. Associate Chairman for Finance and Administrator Internal Medicine Douglas Bebbington Director of University Internal Audit Dorothy K. Robinson Vice President and General Counsel, or Designee Stephanie Spangler, M.D. Deputy Provost for Biomedical and Health Activity Robert Udelsman, M.D. Chair Department of Surgery Rev. 12/98 Rev 2/01 Rev 3/01 Rev 9/01 Rev 12/01 Rev 3/05 Rev 5/06 Rev 1/08