Patient with chest pain
advertisement

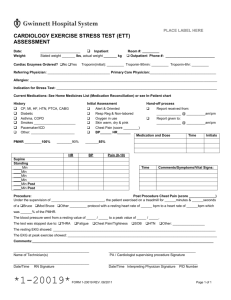
A Patient with Chest Pain A 58-year-old man comes to the Yale Emergency Department complaining of substernal chest discomfort. He states that it has occurred early in the morning when he walks outside to get the newspaper, and diminishes when he rests after about 5-10 minutes. He describes it as a dull ache in his midsternal area that doesn't radiate anywhere but causes him to feel like he can't catch his breath. He states that it began about five months ago and hasn’t changed in intensity or frequency but he is concerned because his brother (age 52) recently “died of heart attacks.” He denies headaches, visual problems, cough, epigastric pain or any known medical problems. He quit smoking 6 months ago, but drinks an occasional beer or two with dinner. He works in a pizzeria and lives at home with his wife and four children all of whom are healthy. Family history is also noted for hypertension and non-insulin dependent diabetes in his brothers. His mother died of a stroke; his father died of a heart attack at age 82. P.E. reveals an anxious WM. T 996; P 110; R 20; BP 160/92. Skin - normal. LN - nonpalp. HEENT - normal. Chest - clear. COR - JVP 7 cm; RRR 1/6 SEM at LLSB radiating to L 2nd IC space. + S4; - S3 or rub. Abd - soft without organomegaly or tenderness. G/R - benign with normal rectum; heme negative. Neuro - nonfocal. LABS: Na 138, Cl 104, K 3.9, HCO3 25, Cr 1.1, glucose 180 Hb 14.0, Hct 42.0, WBC 8.3, plts 355K UA: clear/1.016/no cells or casts EKG: S tach/110 rate/normal intervals no ST-T wave changes are noted CXR: normal heart size/clear lung fields 1. What is your most likely diagnosis and why? 2. Name at least 5 other common entities that need to be considered in the differential diagnosis? What aspects of the history, physical, laboratory features would you look for to suggest these other possibilities? 3. Describe the anatomic blood supply to the heart and the basic pathogenesis of cardiac ischemia. 4. What major risk factors for ischemic cardiac disease? Which are particularly relevant to this patient? 5. Would there be any diagnostic benefit from doing an exercise stress test on this patient? Describe the basic principles of this test. What if the patient cannot exercise? What if his baseline EKG showed a left bundle branch block? 6. What are the major classes of medications available for this patient? Describe their basic mechanisms of action, modes of administration and potential side effects. 7. Is coronary angiography indicated for this patient? indications, benefits and risks? 8. What would be an indication to consider coronary angioplasty or bypass surgery? Describe their benefits, longterm success rates, and risks. 9. Although employed, the patient does not have health insurance. How might his lack of insurance influence your treatment and follow-up care? What are its major A Patient with Anemia A 69-year old woman was admitted to the hospital because of severe anemia. She claimed that she had been healthy her entire life without any known medical problems other than occasional gastroesophageal reflux for which she takes a proton pump inhibitor. Her current problems began about 3 months ago when she began to notice a decreased appetite and fatigue. This progressed and recently she noted more fatigue, numbness in her distal extremities, and dyspnea when she walked upstairs. Her anorexia has continued and she states that she has a "sore throat all the time"; her weight has dropped 10 lbs over 3 months. She denies any travel, unusual ingestions, chest pain, headache, cough, back pain, vaginal or rectal bleeding. P.E. reveals a thin elderly woman in no acute distress. T 979, P 110; R 16; BP 110/78; O2 saturation 96%. SKIN - pale, dry with decreased turgor; no rash or lesions noted. LN - none palp. HEENT - conjunctivae are pale; fundi are benign; oropharynx is red with a smooth tongue and cracked lips at the lateral margins. Chest is clear. CORRRR II/VI SEM at LLSB radiating to L 2nd ICS; no diastolic murmurs; no S3. ABD - soft with a vague midepigastric tenderness but no palpable masses or hepatosplenomegaly. G/R - pelvic exam is normal without adnexal masses or bleeding from cervix; rectal exam is benign with brown stool and no gross blood; hemoccult is positive. Neuro exam reveals impaired recent and distant memory; proprioception and vibration sense are abnormal in upper and lower extremities; otherwise exam is normal. LABS: Na 143, K 3.9, Cl 106, HCO3 25, Cr 1.2, glu 119 Hb 6.0, Hct 18.2, WBC 3.9 (normal differential), MCV 89, plts 400 K UA: clear/1.012/no protein, glucose, cells or casts EKG: S tach 110/nl intervals/no ST-T changes CXR: mild increased heart size/clear lung fields QUESTIONS: 1. Describe where red cells are produced, what controls their production and what their normal life span is in the circulation. 2. What are the major pathophysiologic mechanisms by which anemia can develop? Give three examples of each. 3. What are the major morphologic classifications of anemia based on RBC volume? Give three examples of each. 4. What aspects of the history, physical exam and lab data suggest specific possibilities for this patient? What other information would you seek in the history and physical? 5. What would be your first diagnostic steps in evaluating this patient's anemia? The intern orders a Fe studies which reveal the following: Serum Fe 20 ug/dL Serum TIBC 400 ug/dl Serum ferritin 10ug/L The patient is discharged with Fe supplementation, but returns to the Emergency Department with minimal change in her symptoms. Her repeat CBC shows: Hb 8, Hct 24, WBC 3.8, MCV 112 6. What would your differential diagnosis be now, and what additional tests would you order? The peripheral smear is reviewed and reveals two six lobed PMNs in addition to macroovalocytes. 7. Describe a plausible scenario to explain the patient's entire presentation. A Patient with Shortness of Breath A 53-year-old man is admitted from the emergency room with shortness of breath (SOB). He had never had this problem until about 2 weeks PTA when he began to notice difficulty breathing when climbing stairs. Last week he began to have SOB when walking less than one block and last night he awoke from sleep and had to get up to "get some air". He denied any fever, cough, hemoptysis, chest pain or discomfort, back pain, urinary abnormalities, abdominal pain or ankle swelling. The patient has visited the Yale Emergency Department on many occasions over the last 15 years. He has a history of hypertension for 10 years and Type II DM diagnosed two year ago. He has been prescribed various medications to help control his hypertension and diabetes but he has been non-compliant and states cannot afford to pay for them. He is currently unemployed, lives in a New Haven shelter, has no health insurance and rarely keeps his clinic appointments in the Primary Care Center. He smokes and drinks alcohol regularly, but he can't quantitate the amount or duration of each. P.E. reveals a thin man appearing older than his age with difficulty breathing. T 976; BP 180/100; P 120 reg; R 36. SKIN - normal turgor without rash or spider angiomata. LN - none palp. HEENT - conj normal. FUNDI - sharp discs; vessels reveal "copper wiring" changes with A-V nicking but no exudates or hemorrhages; oropharynx, TMs and sinuses are benign. CHEST - diminished tactile fremitus with dullness to percussion at both bases about 1/4th the way up posteriorly; breath sounds are diminished at both bases but rales are audible about 1/2 way up bilaterally. COR JVP estimated at 12 cm H2O. PMI is diffuse, sustained and is felt lateral to the anterior axillary line. Ascultation reveals regular rhythm, but tachycardia; S1 is diminished in intensity; S2 is loud and there is evidence for an S4 and S3. There is a 2/6 holosystolic murmur heard at the apex that radiates to the left axillary line and can be heard as far back as the patient's thoracic vertebral spine. Abdomen is soft, without hepatosplenomegaly or evidence for ascites. G/R exam is benign, extremities are without edema and neuro exam is nonfocal. LABS: Na 129, K 3.0, Cl 100, HCO3 22, Cr 1.2, glu 258 13.0 Hb 13.0, Hct 38.6, WBC 11.0 UA: clear/1.025/2+ protein/2+ glucose/no ketones EKG: S tach 120/nl intervals/+ for LVH by voltage criteria no ST-T wave changes CXR: heart size enlarged; + Kerley B lines + bilateral alveolar interstitial edema with bilateral pleural effusions ABG (RA) 7.48/28/55 (O2) QUESTIONS: 1. Does this patient have congestive heart failure? If so, what aspects of history and physical exam support the diagnosis of CHF? What other clinical findings would you look for? 2. What are the most common underlying etiologies of systolic heart dysfunction leading to congestive heart failure? What are the most common etiologies of diastolic dysfunction? Which would be most likely in this patient? 3. What is the pathophysiology of the diminished S1, loud S2, and audible S4 and S3 sounds? What is the most likely source of the heart murmur? 4. Is there a role for echocardiography or stress testing for this patient? 5. Identify at least three factors responsible for the patient’s inability to adhere to medical regimen? What steps might you take to assure long term adherence in the future? 6. What acute medical interventions would you pursue to initially treat the pulmonary edema? 7. What pharmacologic interventions should be considered for therapy on a chronic basis? Which ones have been shown to improve survival for patients with chronic CHF? Does race have an impact on response to therapy? A Patient with Fever and Cough In December, a 71-year-old woman is admitted because of fever and productive cough. She claims feeling okay until about 4d PTA when she noted the onset of cough. Initially nonproductive, the cough began to become productive of yellowish sputum and was associated with left sided chest pain. Two days PTA she noted feeling chills and had a temperature of 102oF. The fever, cough and chest pain continued over the next 48 hrs so she came to the Yale Emergency Department. She denied hemoptysis, weight loss, sore throat, sinusitis, back pain, diarrhea, rash, joint pain or headaches. She has a history of congestive heart failure related to ischemic heart disease that has been controlled with Lasix, an ACE- inhibitor, and Lopressor. She is a former smoker but quit 3 months ago when her husband died of lung cancer. She denies alcohol use, recent travel, domestic pets or any risk factors for HIV exposure. She is a retired corporate attorney and she lives alone in New Haven. P.E. reveals a thin woman in mild respiratory distress. T 102.4; R 28; P 120; BP 128/84; O2 saturation is 89% on room air. SKIN - normal but with decreased turgor; LN - none palp. HEENT - sinuses nontender; TMs mildly red but no middle ear fluid; oropharynx is mildly red but no exudate. CHEST - remarkable for splinting to the left side on deep inspiration. + dullness to percussion ≈ 1/4 way up on left side; decreased breath sounds at left base, but egophony and bronchial breath sounds are evident as one listens more superiorly on the left side. The right chest is clear. COR RRR without murmurs or rubs. ABD - soft, nontender without hepatosplenomegaly. NEURO - nonfocal. LABS: Na 143, K 4.2, Cl 100, HCO3 29, Cr 1.0, glu 150 Hb 13.8, Hct 39.8, WBC 18.0 (54 segs, 5 bands, 41 lymphs), plts 255K UA: clear/1.020/1+ protein/no cells or casts EKG: NSR/normal rate, intervals and no ischemic changes CXR: nl heart size/left lower lobe infiltrate is present that obscures the left heart border Sputum Gram’s stain: a few PMN, many epithelial cells, and scattered Gram positive and Gram negative cocci and rods are seen. QUESTIONS: 1. What is your most likely diagnosis? 2. What host factors unique to this patient places her at risk for such a diagnosis? 3. What features of the history and physical exam support this diagnosis? 4. Describe the physical findings in the chest and what they indicate. 5. Is the sputum sample helpful in the diagnosis of this patient? What features of the Gram stain do you look for in evaluating the value of the sputum sample? 6. What kinds of infectious agents can produce this syndrome? Which would be most common? 7. Are there any other diagnostic tests you would order before initiating therapy? 8. What antibiotic(s) would you initiate in this patient empirically? 9. Should the patient be hospitalized or could she be treated as an outpatient? The patient’s sputum culture grows normal flora. Blood cultures grow S. pneumoniae that is susceptible to penicillin. 10. What would you do now, and how can we prevent this from recurring again? A Patient with Syncope A 49-year-old man is admitted from the emergency room because of syncope. He states that it occurred while he was standing for a few hours watching his daughter’s softball game on the fourth of July. It was preceded by 5-10 seconds of lightheadedness, diaphoresis and nausea. He fell to the ground, awoke within a minute and sustained no injury or head trauma. He denied any associated headache, visual change, chest pain, SOB, palpitations or back pain. He never had such an episode before. His only past medical history was mild hypertension for 2 years treated with Lopressor. He is a smoker but denies any regular alcohol use. Physical exam reveals a scared middle aged man in no acute distress. T 992; P110; R 20; BP (lying down) 140/88. SKIN - normal; LN - none palp. HEENT - no head trauma; conj normal, Fundi show normal discs and vessels without exudates or hemorrhages; oropharynx is normal; TMs are clear. CHEST is clear. COR - RRR 1/6 SEM LLSB that decreases with Valsalva strain; no diastolic murmurs; rubs or S3 audible. ABD - soft nontender without hepatosplenomegaly or flank tenderness. G/R normal with no rectal masses; heme neg. NEURO - nonfocal. LABS: Na 142, K 4.0, Cl 106, HCO3 23, Cr 0.9, glu 107 Hb 14.6, Hct 43.0, WBC 9.6, plts 300K UA: clear/1.023/no protein, glucose, cells or casts EKG: S tach 110/normal intervals/no ST-T wave changes CXR: normal heart size/clear lung fields QUESTIONS: 1. How do you define syncope and does this patient fulfill the definition? 2. What other questions would you ask the patient? 3. What particular physical exam findings are important? 4. What are the major causes of syncope? Which one is most common overall and which is most likely in this patient? The resident admitting the patient to you is worried about a neurological process and orders a head CT and an EEG. The attending physician is more worried about a cardiac cause and wants to obtain a cardiac echo, as well as ambulatory EKG monitoring for a possible arrhythmia. 5. Which one do you agree with, if either? Why or why not? A head CT and EEG are performed and are normal. A cardiac echo reveals normal ventricular function, normal chamber sizes and no valvular abnormalities. The patient’s brother is a cardiologist and wants the patient to be referred for electrophysiologic testing. 6. In very simple terms, what are the basic principles of electrophysiologic testing and would it help in the assessment of this patient? A Patient with Pleuritic Chest Pain and Dyspnea A 63-year-old woman is admitted to the hospital because of acute dyspnea and right sided chest pain. She has a long history of medical problems including hypertension, and insulin dependent DM. She sustained an inferior-lateral wall transmural myocardial infarction 5 years ago with a residual left ventricular ejection fraction of 30%. Three years ago, she underwent a left mastectomy for breast carcinoma and completed 6 months of adjuvant chemotherapy because of tumor involvement in 3 axillary lymph nodes (hormone receptors were negative). She had been feeling relatively well lately until the day of admission when she noted the acute onset of dyspnea in the morning. This progressed throughout the day and was associated with pain in her right chest that increased upon inspiration, so she came to the Yale Emergency Department. She denied fever, cough, headache, abdominal pain, back pain, or light headedness. Her medications include insulin, Lasix, Lopressor, and an ACE-inhibitor. PE reveals a dyspneic obese woman. T 99.4, R 32, P 120, BP 130/84. SKIN - no rash or lesions. LN - none palpable. HEENT - conj pink; Fundi - background but no proliferative retinopathy; oropharynx benign. CHEST - clear; mastectomy scar healed. COR - RRR without murmurs or rub. ABD - obese, soft, nontender without hepatosplenomegaly. NEURO - normal. EXT – benign without edema or erythema. LABS Na 136, K 3.0, Cl 99, HCO3 24, Cr 1.2, glu 160 Hb 14.0, Hct 42.1, WBC 12.2 (normal differential), plts 375K UA: clear/1.016/2+ protein/2+ glucose/no ketones, cells or casts EKG: Stach 120/ Q waves in II, III, avF, V4-6; no change from recent EKG CXR: clear lungs, normal heart size ABG (room air) pH 7.52/pCO2 22/pO2 51 1. What would be your differential diagnosis of this patient’s presentation and what would be your leading concern? 2. What are the most common risk factors predisposing patients to pulmonary embolism? Which ones are most relevant to this patient? 3. What diagnostic tests would you perform to assess the possibility of pulmonary embolus? Describe the advantages and disadvantages of each. 4. The intern orders a ventilation-perfusion scan which is read as “high probability”. What acute therapy would you choose and what benefit does it provide to the patient? 5. What would be your approach to long term management? A Patient with an Altered Mental Status Your first week on the medical service, you are asked to assume the care of an 88-year-old man who was recently admitted for a bleeding gastric ulcer. He was a resident of a nearby nursing home and has a long history of multiple medical problems including congestive heart failure, insulin dependent diabetes, chronic osteoarthritis, COPD with exacerbations of acute bronchitis, cerebrovascular disease (he sustained a mild thrombotic left hemispheric stroke 5 years ago), dementia, Parkinson’s disease, and depression. He underwent endoscopy the day after admission, he had his ulcer lasered locally to stop the bleeding, and he was transfused two units of PRBC to restore his hematocrit to 32%. You are called by the nursing staff because family members noted that he has had the new onset of confusion and somnolence that have fluctuated throughout the day. His medications include Lasix, Lisinopril, Digoxin, Insulin, Prednisone (20 mg/day), Sinemet, Haldol, and Effexor. P.E. reveals a thin elderly man who is awake but minimally responsive to questioning or stimuli. T 100.2; P 120 irreg irreg; R 16; BP 170/82. SKIN - dry with decreased turgor but no rash or lesions. LN - none palp. HEENT- conj normal; bilateral cataracts prevent fundoscopy; oropharynx has dry mucosa but no erythema; he wears bilateral hearing aids. CHEST - clear. COR - JVP 5 cm. Irreg irreg with variable S1 intensity, loud S2, no murmurs or rubs. ABD - soft; no masses or hepatosplenomegaly. G/R - normal; heme neg; a Foley bladder catheter is in place. EXT - no edema. NEURO - minimally responsive to questions and stimulation; cannot cooperate with cranial nerve, motor, cerebellar exam; reflexes are diminished throughout; Babinski signs are negative. LABS: Na 149, K 5.0, Cl 109, HCO3 29, Cr 1.6, glu 355 Hb 11.0, Hct 31.5, WBC 9.2 (normal differential), plts 255K UA: clear; 1.020; 1+ RBC, 2+ WBC; no casts EKG: Irreg irreg about 120/min; QRS and QT intervals are nl no ST-T wave changes noted CXR (AP only): nl heart size/loss of diaphragm shadow behind the heart on the left side. QUESTIONS: 1. Does this patient have delirium? What bedside features support this diagnosis? 2. What aspects of this patient predipose him to delirium? 3. What are potential precipitating causes of delirium exist for this patient? 4. Are there additional diagnostic tests you would order at this time? 5. On the day of admission, the patient’s family asks you not to institute any “heroic” measures if the patient stops breathing or if his heart stops beating. They indicate that he “has suffered enough” and that he is no longer competent to make decisions about his medical care. How do you respond? 6. Assuming that your management is successful, what measures can you recommend to diminish the likelihood that this scenario will recur? A Patient with Ascites A 52-year-old woman was admitted to the hospital because of increased abdominal girth and evidence for new onset ascites. About two months prior to admission she noted unexpected weight gain of 10 lbs. This was followed by ankle swelling when she stood up for long periods, and progressed to the point that her clothes became too tight. She said it felt like she was pregnant. Over the course of the last two weeks she noted increased fatigue, more difficulty sleeping and dyspnea on exertion. Today she claimed that her abdomen and shoulders hurt so she sought medical attention. She has a history of alcohol abuse over the past 20 years, and was hospitalized once for pancreatitis related to alcohol, but had no history of liver disease. She denied any chest pain, cough, change in bowel habits, jaundice, vaginal or rectal bleeding. She lives with her husband and has three healthy children. She has no family history of similar problems; her parents both died of heart disease. P.E. reveals a thin woman with protuberant abdomen in mild respiratory distress. T 99oF; P 100; R 30; BP 120/80. SKIN - normal but with scattered spider angiomata. LN - none palpable. HEENT - conjuctiva normal; FUNDI - normal; oropharynx dry without lesions. CHEST - clear with decreased breath sounds at both bases about 1/4 way up; percussion note is dull over the same area and there is an absence of tactile fremitus at both bases. COR - JVP is 6 cm; RRR with no murmurs, gallops or rubs audible. ABD - protuberant but symmetrical on inspection; there are no palpable masses; liver and spleen are not palpable; there is mild tenderness throughout but no rebound pain; flank dullness and fluid wave are evident; BS are diminished but present. G/R - speculum exam is normal; rectum is normal; stool heme negative. NEURO - nonfocal. EXTREMITIES - 2+ edema. LABS: Na 128, K 3.2, Cl 107, HCO3 17, BUN 4, Cr 0.5, glu192 Hb 13.0, Hct 39.0, WBC 10.5 (normal differential), plts 143 K UA: clear/1.010/1+ protein; no glucose, ketones, cells or casts EKG: NSR 100/nl intervals/no ST-T wave changes CXR: bilateral pleural effusions; normal heart size QUESTIONS: 1. What aspects of this patient's history and physical suggest the presence of ascites? 2. What other information would you seek from this patient, and what are the possible etiologies for her ascites? 3. Describe the basic pathophysiology for ascites development . 4. Explain the patient's serum Na, K, BUN and anion gap. The patient undergoes a paracentesis. Two liters of clear ascitic fluid is removed with the following values: albumin 0.7 gm/dL, protein 1.8 mg/dL, glucose 105, amylase 20, WBC 152 (13 segs, 20 monos, 67 tissue cells); gm stain reveals no bacteria. Serum albumin is 2.5 gm/dL. 5. How does this information assist you in the determining the cause of the patient’s ascites? The patient undergoes abdominal ultrasound which reveals a small, irregular liver and enlarged spleen in addition to ascites. No abnormal pelvic mass lesions are noted. 6. What pharmacologic therapy would you initiate at this time? How would you monitor the effectiveness of your therapy in the hospital? 7. What additional lifestyle changes would assist in the successful treatment of the ascites in the long term?