CALIFORNIA STATE UNIVERSITY, NORTHRIDGE
advertisement

CALIFORNIA STATE UNIVERSITY, NORTHRIDGE
CONSU!mR PERCEPTIONS AS A
GUIDE TO HOME HEALTH PLANNING
A thesis submitted in partial satisfaction of the
requirements for the degree of
Master of Public Health
by
Charlotte Lee Laubach
August, 1981
The Thesis of Charlotte Lee Laubach is approved:
California State University, Northridge
ii
ACKNOWLEDGEMENTS
There are so many people who deserve recognition
for their contributions to this project.
First, I wish to express my gratitude and
appreciation to the directors and staff at National In-Home
Health Services who provided the setting for, generously
supported, and enthusiastically participated in this study.
Words cannot express my deep appreciation to Ruth Geagea,
Associate Director of Nursing Services and Director of
Educational Activities, and also a member of my thesis
committee.
Her personal interest, support and guidance
were invaluable to me.
I acknowledge my indebtedness to other members of
my committee, to Dr. Michael Kline for his constructive
criticism and enthusiasm, and to my chairman, Dr. Goteti
Krishnamurty for his patience, encouragement and counsel.
I also wish to express my thanks to Dr. Roberta
Madison for her assistance with analysis of the data.
To
Phyllis Mitchell, whose contributions reach far beyond
her typing skills, I express thanks also.
Last, and by no means least, I wish to express my
sincerest appreciation to my friends and family whose interest, encouragement and assistance sustained me
iii
throughout this project.
Very special thanks go to my
husband, Peter, and my four sons for their love and
understanding during my years in school.
iv
;.:
'
TABLE OF CONTENTS
PRELIMINARIES
PAGE
APPROVAL •
ii
ACKNOWLEDGEMENTS • •
iii
LIST OF TABLES
viii
ABSTRACT • • • •
X
CHAPTER
I.
I I.
INTRODUCTION • •
1
Statement of the Problem •
2
Statement of the Purpose
4
Objectives of the Study
4
Definitions
5
Limitations of the Study
6
LITERATURE REVIEW
7
Development of Consumer Role
7
Consumer Role in Health Services
Planning • • • . . . . • . • .
9
Home Health Care Services - Structure
and Utilization
. • • . .
11
Utilization
14
Perceptual Functioning .
15
Attitudinal Research .
17
Behavior of Older Adult
v
.
17
CHAPTER
PAGE
Similar Studies .
III.
• 18
METHODOLOGY
• 20
Target Population .
• • 20
Selection of Survey Instrument
• . 21
Selection of Study Sample .
.
.
• • 22
Construction of the Survey Instrument .
. 23
Pre-Test and Revisions
25
Implementation of the Survey
. 25
Collection and Organization of the Data
Follow-up of Non-Respondents
Organization of Data
~/
/'
'
. . . .
• • 27
.
Description of the Study Sample .
IV.
V.
26
RESULTS OF THE STUDY
•
•
30
•
• 35
Part
I.
Part
II.
Consumer Needs Responses . . . 45
Part III.
Rating of Consumer Responses
by Management Advisory
Committee
. . . • • . . . . . 57
SU}~RY,
Quality of Care Responses
29
. . 35
CONCLUSIONS, AND RECOMMENDATIONS . . 61
Summary . •
61
Limitations and Weaknesses of the Study
67
• • 68
Conclusions
. 69
Recommendations
BIBLIOGRAPHY
• • • 72
vi
'.··.i.,..
PAGE
APPENDIXES . • •
78
A.
Questionnaire
79
B.
Cover Letter . .
80
C.
Management Advisory Committee Instrument
83
vii
LIST OF TABLES
TABLE
PAGE
lo
Response to Mailed Questionnaire
2o
Telephone Follow-up: Reasons for NonResponse to Questionnaire o o o o o o o o o 28
3o
Identification of Respondent to
Questionnaire o o o o o o o o
0
0
0
0
0
27
30
4o
Comparison of the Characteristics of
Patients in Sample by Office and Totals o o 32
5o
Patient Characteristics of Sample and
National Study (1978) o o o o o o o
o o 34
6.
Consumer Perceptions of Patient Teaching
o o 37
7o
Respondent by Interest in Additional
Information o o o o o o o o o o o o . o o o 39
8o
Consumer Perceptions of Delivery of Services
9
Consumer Perceptions of Quality of
Professional Staff o o o o
0
0
41
0
43
lOo
Health Education Needs
llo
Relationship of Survey Respondents to
Health Education Needs o o o
o o o • o 48
l2o
Supportive Service Needs
13o
Relationship of Living Arrangement with
Supportive Service Needs o o o o o o o o o 51
14o
Relationship of Age by Sex by Supportive
Service Needs
o o o . o o
o o o o o 53
15o
Needed Psychological Counseling by
Living Arrangement
o o o
46
0
viii
0
0
0
50
o . o o o 54
TABLE
16.
17.
18.
19.
PAGE
Interest in Attending Group Support
Meetings . . . . . . . . . . . . .
55
Identification of Respondent Interested in
Group Meetings • • . . . . . . . .
56
Management Advisory Committee Rating of
Consumer Responses to Selected Variables •
58
Mean Rating Scores of Variable Categories
by Management Advisory Committee • . . . .
60
ix
ABSTRACT
CONSUMER PERCEPTIONS AS A
GUIDE TO HOME HEALTH PLANNING
by
Charlotte Lee Laubach
Master of Public Health
August 1981
This exploratory study was conducted to collect
and analyze consumer subjective responses toward home
health services, for the purpose of providing added perspective to agency performance evaluation, and to identify
needs which might suggest modification in planning and
delivery of agency services.
An interdisciplinary literature review was carried
out in the fields of Gerontology, Sociology, Psychology,
Health Services, Consumer Science and Attitudinal
Research.
Using the literature as a background and work-
ing closely with home health agency staff members a survey
questionnaire instrument was constructed.
X
The instrument
contained 19 items with Likert-type scale format being
used where attitudinal responses were desired.
Following
pre-testing and revision the instrument was administered
to 400 randomly selected horne health care consumers who
had received service from the agency during the previous
eight months.
One hundred and forty-three usable ques-
tionnaires were obtained for the study.
Questionnaire response data was coded and mean
frequencies, statistics and cross-tabulations were obtained using the Statistical Package for the Social
Sciences.
Data was tabulated and analyzed.
A second instrument was constructed to collect
ratings of consumer response data by the Management Advisory Committee.
The committee independently rated
those responses from the first questionnaire which pertained to quality of care (teaching, delivery of services
and quality of the professional staff) and consumer needs
(consumer awareness or Health Education needs and support
services needs).
Mean rating scores were tabulated and
analyzed.
The Advisory Committee indicated that they were
most satisfied with consumer perceptions of quality of
care, less satisfied with the unrnet needs expressed by
consumers, and least satisfied with the lack of consumer
awareness of the potential of horne health care services.
xi
Conclusions of the study were consistent with
beliefs held by agency staff personnel prior to the study.
Most of the consumers felt that they were receiving comprehensive and quality care.
Many were unaware or misin-
formed about potential services available from a home
health agency.
A number of home health consumers, espe-
cially elderly persons living alone, felt the need for
more supportive services than they were able to obtain.
Recommendations related to the needs of the home health
care consumer, and to the collection of consumer perceptions.
xii
CHAPTER I
INTRODUCTION
"Good Health care is a basic human right!"
(58:528).
Good health care by recent definition, includes
the right of the consumer to be "heard" and to be "informed" in planning and delivering that health care (1:24)
(2).
This right has been encouraged and protected by
government regulations (U.S. Congress PL 93641)
(OAA).
Planning and responding to consumer needs are considered
essential characteristics of good health services (16:13)
(19:14).
Home-health care is a new and rapidly developing
industry due to the increase of the elderly in our population, the extension of average life-expectancy and rising costs of institutional care (9:14).
Growth has been
spurred by the financial support from government through
Medicare and Medi-Cal (California's Medicaid).
This
growth of home health services accompanied by increased
emphasis on consumer involvement has created a need for
reliable and unbiased methods of eliciting consumer responses.
In 1976 a National Public Health Task Force on
Research and Evaluation suggested in a policy statement
that "research and evaluation activities be designed to
1
2
assess variables such as . • . , consumer satisfaction,
(54:2).
A national professional Horne Health Associ-
ation advocates that "planning strategies should be responsive to gaps in service programs and unrnet needs as
they are identified" (9:4).
Health Services provided away
from the agency setting present a challenge to adrninistrators in evaluating the quality of care.
In an atmosphere
that lends itself to the exploitation of the homebound
and their rights, monitoring and maintaining professional
standards of care is extremely critical (16:13).
Bloom suggests that social research be carried out
which concerns "the sensitivity to and responsibility for
the well being of the participant" (6:292).
An Administration on Aging goal suggests that we
learn about the characteristics, attitudes and behaviors
of older persons, which will require consideration in relation to existing and future policies and program designs
(40:v).
Effective methods for collecting and analyzing
consumer input from a predominantly ill, elderly and hornebound population have not yet been established.
Statement of the Problem
The rationale for consumer involvement is that
it is
An opportunity for the patient to retrieve the
bargaining power dissipated through third party
payment mechanisms, but also to insure that the
3
services and care provided to him will be of
high quality, at a reasonable cost, and relevant
and responsive to the needs of those for whom
they are intended. Community participation in
health services also serves to raise the consciousness of the people regarding the definition of good health care and how to get it
(17:52).
With government support through financial
reimbursements Medicare and Medi-Cal (Medicaid) , also
come government regulations.
Health planners must now
include a social perspective to professional and organizational planning strategies.
A national professional
Home Health Association policy directs that
Community home care systems should be based on
continuous planning.
. Planning strategies
should be responsive to gaps in service programs
and unmet needs as they are identified (11:4).
During this author's internship with a community
based home health agency, it was revealed that the Subcommittee on Agency Evaluation had recommended that an
agency-wide survey of consumers (patients and/or families)
be conducted.
Data from the survey would be used by the
agency as a basis for program evaluation and also as a
resource for program modification and planning.
Discus-
sions with staff members at all levels revealed a high
interest in obtaining and assessing consumer perceptions
toward the services they had received.
In the past, while
helping elderly friends who were receiving Horne Health
services (from a different Home Health Agency), the author
4
had observed the need for home health care services to
be more responsive and relevant to the consumer.
Statement of the Purpose
The purpose of this study was to collect consumer
subjective responses, regarding their perceptions of home
health care services received from a community-based Home
Health Care Agency.
These responses were to be analyzed
and used as one perspective for agency evaluation of their
services and also as a basis for program modification and
planning.
The substantive hypothesis is:
(a) The following specific questions will be
answered by the data:
(1) Do home health consumers feel that they
are receiving comprehensive and quality
services?
(2) I'Vhich specific needs of the home health
consumer are not being met?
Objectives of the Study
There were two main objectives of this study.
The
first was to collect and analyze consumer perceptions of
home health care services.
The second objective was to
identify needs perceived by home health care consumers.
5
Definitions:
Home Health Agency:
A Home Health Agency is one which
basically provides multidisciplinary health care on a
family-centered basis to the sick, disabled, and injured
in their place of residence.
It provides the interweaving
of skills of a variety of health workers who participate
in planning and implementing community health programs.
It may also provide programs in addition to care of the
sick ( 50 : 18) .
Service:
A service refers to the discipline utilized to
give care to the family or patient:
nursing, nutrition,
occupational therapy, physical therapy, physician services, social work, speech pathology services, and homemaker home health aide services.
It also includes support
elements such as medical supplies and equipment, transportation, laboratory services (50:18).
Consumer:
The patient, and or family or household members
who are involved in his care, who have received services
provided by a Home Health Agency.
Perceptions:
The process of evaluating the information
gathered by the senses and "giving it meaning" (3:57).
Consumerism:
The response of people and organizations to
consumer problems and dissatisfactions.
6
Chronic disease:
(from the Commission on Chronic Illness)
All impairments or deviations from normal which have one
or more of the following characteristics:
are permanent;
leave residual disability; are caused by non-reversible
pathological alterations; require special training of the
patient for rehabilitation; may be expected to require a
long period of supervision, observation or care (45:1).
Limitations of the Study
The study population was limited to patients
and/or families who had received services from the agency
within the past eight months.
If the patient had died
within the past six weeks the family was excluded from
the study.
Poor general health status and/or advanced
old age with its frequently accompanying memory and endurance restrictions may have an impact on the quality
and quantity of responses as well as overall return rate
of the questionnaire.
This was a one-time study for which the agency
provided financial support with budget restrictions.
Agency limitations on the gathering of sensitive information, such as income and education, precluded the use of
such information in this study.
CHAPTER II
LITERATURE REVIEW
A search of the literature was conducted to
assist the researcher in the collection and analysis of
home health consumer attitudes.
This search called for a
multi-disciplinary approach involving the fields of
Gerontology, Sociology, Psychology, Health Services, Consumer Science, and Attitudinal Research.
Five areas of focus relevant to the study were
l.
The health care consumer role--its development and
significance in health care planning.
2.
The structure and utilization of home health care
services.
3.
Perceptual functioning--including age related factors.
4.
Attitudinal research--including age related factors.
5.
Health behavior--including age related factors.
Development of Consumer Role
Consumerism became a dominant political movement
in the sixties.
A great deal has been written about its
development and significance, but only in the last decade
has the health care consumer received much literary attention.
Aaker describes the growth of the consumer
7
8
concept and refers to John F. Kennedy•s message, when he
charged the Congress to
11
meet its responsibility to con-
sumers in the exercise of their rights.
The right to
safety, right to be informed, right to choose and the
right to be heard ...
Appointment of the first Consumer
Advisory Council followed.
This Council identified ten
fields of importance to consumers; the tenth and last on
the list was medical care (1:25).
Novello also reviews
the historical background of consumerism, and the subsequent legislation which has expanded the role of the consumer in the health care process.
Significant consumer
legislation discussed included the Hill-Burton Act of
1946, PL 89-749 in 1966, Amendment to Section 314 of the
Public Health Service Act and in 1974 PL 93-641, the National Health Planning and Resources Development Act.
She
identifies four major characteristics of the consumer•s
role which she feels are needed to improve the health system.
One of these is .. participation in direct health ser-
vices ...
She suggests that the
11
most accepted role of the
consumer is in planning .. (32:3).
The consumer•s role in direct health services is
supported by the Patient•s Bill of Rights (American Hospital Association, 1972) and through the use of ombudsmen
or patient representatives.
Although the Patient•s Bill
of Rights has been modified to cover the home health
9
consumer, the use of ombudsmen in a broad based community
setting would be costly and time consuming.
At the pres-
ent time patients must report dissatisfaction with services by talking directly to the provider, the home health
agency, or if they wish anonymity by calling the County
Health Services.
Consumer Role in Health Services Planning
Most reports in the literature substantiate the
belief that the use of consumer input is an important element in evaluating program effectiveness and planning that
is responsive and relevant.
Schmidt reports that patient needs have often been
evaluated by health status reports or in the case of the
elderly and infirm by those caring for them, or medical
personnel.
Often these reported needs have been found to
be quite different or of a different intensity than those
perceived by the patient himself (39:544).
Hochbaum feels
that "If people are involved in planning it gives them
some feeling of control--a visible symbol of their 'equal
human rights'" (15:267-269).
Sociological literature views the consumer rule
as one of little power and urges the consumer to take a
more active role.
"Consumer awareness of their role in
affecting the output of the health system must be extended
to include awareness of their input contribution and
10
primarily the need for consumer effectiveness on the
entire internal social organization of health" (26:23,24).
The sociologists suggest that social science
should be the discipline to evaluate consumer participation as a means to improve health services.
Social scientists .
. come closest to meeting
the professional and technical requirements for
reliable and objective investigations both of
the concept of consumer participation in the
planning of health services and of the various
operational systems based upon it.
. Such
scientific investigations . . . are desperately
and urgently needed (15:267).
The implementation of consumer participation in
the planning process is still in the exploratory and developmental stage.
In a review of health consumerism is-
sues, Feingold presents a ladder representing different
levels of consumer participation.
The lowest degree is
referred to as "informing" where there is information presented to consumers but no allowance is made for feedback
or discussion.
The second level he calls "consultation"
where the citizen's perceptions are elicited.
He suggests
that it is a step in the right direction but that there
is no assurance that the information will be used (38:
157,158).
A report on a workshop for health professionals
to discuss the new consumer role, reported skepticism
about learning "how to hear from those who need to be
heard"
(56:86).
Professional planners felt that consumer
11
interest is only shown when the patient is ill (56:87).
One participant suggested "Consumers could evaluate the
care they receive by a means of a questionnaire asking
what they thought of treatment received" (56: 87, 88).
Home Health Care Services Structure and Utilization
A
rapid growth in home health agencies followed
the advent of Medicare and Medi-Cal (Medicaid).
In 1980
there were approximately 2,500 home health agencies in the
United States (42:23).
Home health agencies are public
or private agencies that provide a coordinated multidisciplinary range of health care services to the homebound patient who needs skilled health care, on a parttime, intermittent basis.
Most of the time these services
are paid for by hospital and medical insurance plans
developed by Medicare (51).
In recent years private in-
surance companies have begun to recognize the cost benefits of covering health services in the home, instead of
in institutions, and an ever-increasing number are willingly providing reimbursement for in-home services.
A
very small percent of services are paid for by private
individuals.
"Your Medicare Handbook" printed in 1975, lists
services which are covered by Medicare and defines
12
eligibility requirements for hospital and medical
insurance coverage (51:35-37).
Home Health Services Covered by Medicare
Medicare can pay for:
1.
2.
3.
Part-time skilled nursing care
Physical therapy
Speech therapy
If you need part-time skilled nursing care,
physical therapy, or speech therapy, Medicare
can also pay for:
- Occupational therapy
- Part-time services of home health
aides
- J1.1edical social services
- Medical supplies and equipment
provided by the agency
Home Health Services Not Covered by Medicare
Medicare cannot pay for these items.
1.
2.
3.
4.
Full-time nursing care at home
Drugs and biologicals
Meals delivered to your home
Homemaker services
When Hospital Insurance Pays for Home Health Care
Medicare's hospital insurance (Plan A) can
pay for home health visits if six conditions are
met. All six conditions must be met. These
conditions are:
(1) you were in a qualifying
hospital for at least 3 days in a row, (2) the
home health care is for further treatment of a
condition which was treated in a hospital or
skilled nursing facility, (3) the care you need
includes part-time skilled nursing care, physical therapy, or speech therapy, (4) you are
confined to your home, (5) a doctor determines
you need home health care and sets up a home
health plan for you within 14 days after your
discharge from a hospital or participating
skilled nursing facility, and (6) the home
13
health agency providing services is
participating in Medicare.
Under these conditions, hospital insurance
can pay the full cost of up to 100 horne health
visits after the start of one benefit period
and before the start of another.
Payment for
these visits can be made for up to a year following your most recent discharge from a hospital or participating skilled nursing facility.
You may be charged only for any non-covered
services you receive.
The horne health agency will submit the
claim for payment. You don't have to send
in any bills yourself.
When Medical Insurance Pays for Horne Health Care
Medicare's medical insurance (Plan B) can
help pay for up to 100 horne health visits in a
calendar year. You do not have to have a 3-day
stay in the hospital for medical insurance to
pay for horne health care. But medical insurance
can pay for the visits only if four conditions
are met. All four conditions must be met. These
conditions are:
(1) you need part-time skilled
nursing care or physical or speech therapy, (2) a
doctor determines you need the services and sets
up a plan for horne health care, (3) you are confined to your horne, and (4) the horne health agency
providing services is participating in Medicare.
Medical insurance can also pay for horne health
visits if this care is still needed after you
have used up the 100 visits covered under hospital
insurance.
After you meet the $60 yearly deductible,
medical insurance pays the full costs for
covered horne health services in each calendar
year. You may be charged only for any noncovered services you receive.
The horne health agency always submits the
medical insurance claim for horne health care.
You don't have to send in any bills yourself.
14
A revised, updated, edition of this book is soon
to be released.
Although home health agencies participating in
Medicare receive a very high percentage of their reimbursement for covered services from Medicare insurance
plans they still receive less than one percent of the
Medicare dollar.
Utilization
30 to 40% of patients in nursing homes could be
safely and effectively treated in the home . .
10% of patients in acute hospitals could be
managed at home
is Dr. Schrifter's interpretation of reports submitted
by the United States General Accounting Office (42:26).
Two doctors claim restrictive eligibility
criteria, over-regulation and inadequate reimbursement
from government sources are some of the reasons that such
a small portion of the Medicare budget is spent for services; services which they claim can improve the patients'
quality of life and reduce the costs of institutionalization dramatically (31:37-41)
(42:23-28).
The fact that
many physicians are unaware of potential services available from home health agencies reduces their utilization
rate.
A study of 600 physicians in New York State re-
vealed that one fourth were unaware of home health services (42:24).
15
Physicians' concerns over loss of control and
malpractice liability, restrict the prescribing of home
services (42:26), even though the patient is more happy
and comfortable at home and would prefer to be there.
Perceptual Functioning
The senses provide the means for assembling and
classifying information but they do not evaluate it. The process of evaluating the information gathered by the senses and giving it
meaning is called perception (3:57).
McKinley writes that the process of perception or
of "evaluating the information" is influenced by both external (social, cultural, economic) and internal (psychological) factors (29:285).
Botwinick agrees with McKinley and also claims
that the processes of perception and the processes of
sensation cannot be separated (7:156-157).
For the older
person, the ability to interpret what is going on around
him is affected by changes in perceptual processing and
sensory processing attributable to physiological aging
(28:9).
These changes in older persons reduce the rate
at which incoming information is integrated.
This is re-
£erred to, in the literature, as "perceptual slowing"
(28:9).
Atchley discusses similar findings in regard to
"perceptual slowing" but feels that they do not seriously
affect the behavior of the individual until after the age
of seventy.
Botwinick also reports on disparate views
16
presented in the literature, regarding the importance of
"slowing" to cognitive and perceptual abilities.
He con-
cludes, by proclaiming, that slowing with age is experienced by everyone, appears to be independent of culture
and health status and is related to vital functions
(7:203).
Factors which may reduce "slowing" include
exercise habits, opportunities for learning, motivational
activities and individual differences (7:203).
No clear-
cut pattern for perceptual functioning with age was found
in the literature.
Individual differences alone, are of
such a wide range that many old people respond more
quickly than many young adults (7:205).
Since sensory functioning is reported to be
inseparable from perceptual functioning, the literature
was examined on physiological aging of sensory organs.
Age associated changes in peripheral sensory apparatus
are reported to alter the quality and quantity of information received from the environment (28:9).
These sen-
sory losses associated with aging are well documented in
the literature ( 6)
( 3)
(53) .
Impairments in vision and hearing are agreed to
have the most impact on perception, with losses in taste
and touch also having a significant effect.
Other
17
physical and psychological factors involving perception
described are emotionality, mentation and intelligence
(6:292).
Attitudinal Research
No attempt will be made to report on the
literature examined on behavioral research.
Discussion
of some advantages and disadvantages of survey research
methods will be discussed under methodology and data
analysis.
Behavior of Older Adult
An understanding of age and its relationship to
behavior, prior to comparing age related behaviors with
selected variables was needed.
That age related behavior
patterns are extremely varied was shown.
Older people show more variability of lifestyles
and personalities than any other (3:53).
Schutz, also reports that there is a wide range
of behavior in the elderly, and his studies examine the
behavior of older adults in relation to lifestyle
(40:152-159).
Botwinick completed an extensive review of the
literature on aging and behavior.
Some of his findings
were (1) the elderly show reluctance to be involved in
decision-making and may exhibit a pattern of avoidance or
non-commitment; that is, they are more inclined to give
18
"no opinion" or "don't know" responses.
( 2) There are
disparate study results regarding the relationship between
levels of "opinionation" and education (7:138-139).
A
study by Gergen and Back indicated that the elderly with
a high school education were more likely to exhibit low
"opinionation."
A previous study done by Botwinick him-
self showed that "opinionation" was higher among those
with a h·igh school education.
He suggests that "the role
of education in the cautiousness of later life requires
further investigation" (7:140).
Similar Studies
Very few actual studies have been done to examine
consumer behavior of the elderly with regard to health
care.
Schutz, Baird and Hawkes report on a study done in
1979, examining the relationship of lifestyle and adult
consumer behavior.
behavior.
Only one chapter deals with health
Unfortunately, only 9 people in this study had
received home health services.
Some conclusions reported
were that elderly people
are generally satisfied with health care services
and express favorable attitudes toward the leadership, professional competency and personal
qualities of health professionals.
They have
found greater concern for economic, time-related,
convenience, and psycho-sociological factors
than for quality of care or where to go for
health care (40:113).
19
Those least satisfied with health care services were
women, blacks and Medicaid recipients (40:113).
Actually there was not a high relationship between
age and consumer health behavior except in evaluating the
competence of doctors, where men over 65 gave them a positive ra-ting that was significant at the .05 level (40:113).
Those in poor health and needing a support
system of friends find the medical care system
least responsive to their needs (40:124).
Bloom discusses problems associated with
interviewing the elderly.
Although directed to those
doing personal interviewing the physical limitations
described are common to respondents of mailed questionnaires.
Physical disabilities which may affect the qual-
ity of data and/or response rate include impaired vision
and/or hearing, physical stamina, language function, emotionality and intellectual capacities (6:292-299).
CHAPTER III
METHODOLOGY
A research study was conducted to collect and
analyze consumer perceptions toward health care services
received from a selected home health care agency.
Re-
sponses would be used by the agency to assist in evaluating their services and to identify consumer needs which
are not being met.
Procedures discussed in this chapter
will include, description of the target population, selection of the survey instrument, selection of the sample,
construction and approval of the survey instrument, pretesting and revision of the instrument, implementation of
the survey, collection and organization of the data and
analysis of the data.
Also discussed will be the use of
a second instrument to obtain ratings by the Management
Advisory Committee of selected data from the first instrument.
These ratings will be analyzed and discussed.
Target Population
The target population consisted of consumers
(patients and/or families) who had received services from
National In-Home Health Services, a community-based home
health agency.
These consumers resided in widely
20
21
dispersed geographic locations covering a large portion
of Los Angeles County, including Santa Clarita Valley,
Glendale, San Fernando Valley and the west side of Los
Angeles, the service areas covered by either the Los
Angeles or San Fernando Valley branches of the agency.
Residential settings ranged from the densely populated
inner city to isolated rural ones.
alone or with an elderly spouse.
A large portion lived
Most of the patients
were over age 65, were predominantly female and had a high
incidence of one or more chronic diseases.
Selection of Survey Instrument
A mailed questionnaire was selected to collect
consumer responses for the following reasons.
1.
Its capability of reaching a larger number of people
living in widely dispersed geographic locations, with
less cost of money and human resources (43:238-245).
2.
Higher quality data can be expected when anonymity
and confidentiality are assured (43:238-245).
3.
Written responses allow the elderly respondent time
to deliberate, time to consult with family members
and thereby presenting a more reliable, better overall
response (43:240).
4.
Self-responding completion, allows self-pacing, that
can be done in small increments or delayed temporarily if patient's health status is lower than normal.
22
This method also reduces fatigue and avoids
emotionality (39:545).
The use of a mailed questionnaire was approved by
the agency and financial support (a budget of $400) was
allocated.
Selection of Study Sample
The budget provided resources which permitted 400
questionnaires to be used in the study.
Costs included
printing and mailing of a four-page questionnaire and
cover letter accompanied by a stamped return envelope.
Four hundred patients were selected randomly from the target population.
Starting with the current patient roster
and working back in time, patients were selected by rolling dice.
If the numbers presented, summed to an equal
number, the patient was chosen for the study, if odd, they
were rejected.
The sample included patients who had re-
ceived home health services between April 1980 and September 1979.
This selection included 120 patients from the
Los Angeles office and 280 from the Valley office.
The
numbers selected from each office correspond to the ratio
of patients serviced by that office in relationship to
total agency clients--approximately 1-3.
23
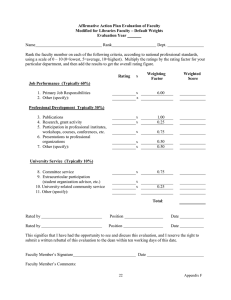
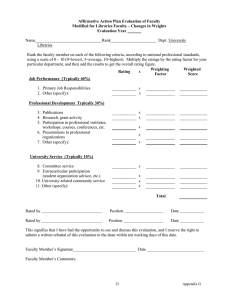
Construction of the Survey
Instrument
The purpose of the study, as stated in the
previous chapte4was to collect consumer subjective responses regarding their perceptions to home health care
services.
1.
Two questions were to be answered by the data:
Do home health consumers feel that they are receiving
comprehensive and quality services?
2.
Which specific needs of the home health consumer are
not being met?
Agency policies and objectives were reviewed to
identify content areas to be examined in program evaluation, which would suggest "comprehensive and quality services."
Personal interviews were conducted, by the
researcher, with the Management Advisory Committee, to
better understand various dimensions of the content areas
to be examined and identify other subject areas, that they
deemed useful in the study.
Based on the objectives of the study, the policies,
purposes and objectives of the agency and discussions with
management advisory staff personnel, three main content
areas were established to examine data for "comprehensive
and quality services" or to answer the first question.
1.
Teaching
2.
Delivery of Services
24
I
I
~ I
3.
Quality of Professional Staff
The identification of needs which are related to
agency services was also considered important to quality
of care evaluation.
The second question was approached by seeking to
identify all needs, both perceived and unperceived, of
the horne health consumer.
Questions which would elicit the data desired
were formulated and organized into a 19 item questionnaire
format.
This process was guided by reviewing attitudinal
research literature by Kerlinger, Parten, Isaac and
Miller (23)
(34)
(20)
(30).
Feedback from agency staff
suggested additional considerations.
Identification information, not available from
patients' records, was requested.
Questions asking for
sensitive information such as educational level or income
were not included.
Most of the questionnaire items asked for a fixedalternative response.
These included dichotomous choice
questions (yes or no) or selection of "appropriate response" questions.
Likert-type summated rating scales
were used when attitudinal (perceptual) information was
sought.
Some open-ended questions were included to probe
for additional information.
25
The questionnaire was then submitted to the
Management Advisory Committee for review and comment.
Their input added validity to the individual questions.
Modifications were performed.
Two research methodology
specialists were asked to review and comment on the questionnaire and appropriate revisions were made.
Two
elderly women, who had received home health services in
the past, were also asked to review and comment.
No re-
visions were indicated as a result of this step.
As a final step, the full agency staff was asked
to review and comment.
Agency approval was granted.
A
cover letter to accompany the questionnaire was written
and approved.
Its purpose was to explain the purpose of
the questionnaire and to encourage consumer response.
(Appendixes 1 and 2.)
Pre-Test and Revisions
The survey instrument (questionnaire) was pretested on 50 members of the sample population who had
received services from the Valley office.
Two very minor
revisions were made in the instrument as a result of the
pre-test but no other problems were identified.
Implementation of the Survey
Questionnaires were printed in two colors to
identify which office had provided services.
Yellow
26
questionnaires were sent to 120 patients who had received
services from the Los Angeles office and the remaining 230
sample members, who had received services from the Valley
office, received white one.
(A code number, representing
the patient's record number, was placed above the return
address of the return envelope, so that data from the
patient's record could be obtained to facilitate analysis
of selected responses.)
Collection and Organization
of the Data
The rate of response from the 400 questionnaires
is presented in Table 1.
Overall response rate was 35.8
percent which netted 143 usable questionnaires for the
study.
Individual office rates ranged closely with 36
percent from the Valley consumers and 34 percent from Los
Angeles consumers.
Nine of the undeliverable question-
naires that were returned had been sent to families where
the patient had died.
The remaining ten had post office
notices attached, stating that there was no forwarding
address.
Two questionnaires returned without data indi-
cated that the patient had died, and the other stated
that patient had been readmitted to the hospital.
Ten
post office notices informed the researcher that the questionnaire had been forwarded to a new address.
27
Table 1
Response to Mailed Questionnaire
Valley
Los Angeles
Total
280
120
400
116
11
3
49
8
0
165
19
3
Number of questionnaires
in study
120
41
Percentages of responses
to questionnaires in
sample study
36
34
Number of questionnaires
mailed
Number of questionnaires
returned not deliverable
without data
-
-
143
35.8
Follow-up of Non-Respondents
The researcher had planned to make ten follow-up
contacts with non-respondents, to complete questionnaires
and to look for non-respondent biases.
After 22 follow-up
telephone contacts, only three had been reached who were
able to complete a questionnaire.
When offered the al-
ternative of completing one by telephone or having a horne
interview, all three chose to respond by telephone.
The
responses from these surveys closely resembled the mean
percentage ratings of the consumers who had returned
questionnaires.
No response bias was identified.
Data
from these questionnaires was not included in the study.
28
Based on the follow-up telephone calls, the reasons for
non-response were attributed to a variety of factors,
with death of the patient representing more than onequarter of them.
More than one-quarter of them were
unable due to health status.
Table 2
Telephone Follow-up:
Reasons for Non-Response
to Questionnaire
Number
NonResponses
Reasons for Non-Response
%
NonResponses
l.
Consumer stated questionnaire
not received (questionaire
completed by telephone)
3
13.6
2.
Expiration of Patient
6
27.2
3.
Physical weakness--mental
confusion
3
13.6
4.
Patient now in Nursing Home
3
13.6
5.
Readmitted to Hospital
l
4.6
6.
Language Barrier (Hispanic
household)
l
4.6
7.
Very short duration of
services (2-3 visits)
2
9.1
8.
Unable to locate patient
by telephone
2
9.1
9.
Stated that questionnaire
had been. returned
l
4.6
TOTAL
22
100%
29
Following follow-up contacts it was observed that
of the questionnaires mailed, 10 were undeliverable due
to no forwarding address.
new address.
Ten had to be forwarded to a
Seventeen were not returned or were returned
unopened or without data in cases where the patient had
died.
Eight were not returned or were returned without
data in cases where patient's health status was reduced
(confusion, weakness, institutionalization).
These num-
bers represent 45 recipients or more than 11 percent of
the sample population suggesting that morbidity, mortality
and fluctuating places of residence may have had considerable impact on the questionnaire response rate.
Organization of Data
Responses from the questionnaires were examined
for reliability, appropriateness and inconsistency.
The
data was then coded, cards were punched and using the
Statistical Package for the Social Sciences frequencies,
statistics and cross-tabulations were computed.
Results
were tabulated to prepare for analysis.
A second instrument was developed to assess the
Management Advisory Committee's ratings of consumer
responses, to achieve a broader-based, more objective
assessment of the data.
30
Description of the Study Sample
Respondents.
For purposes of this study the
consumer is defined as the person or persons who responded
to the questionnaire.
Table 3 shows that more than half
of the questionnaires were completed by the patient, 36
percent by a family member, and a little over 12 percent
by patient and family together.
Less than 2 percent of
respondents were unknown.
Table 3
Identification of Respondent to Questionnaire
Number
of
Responses
Respondent
Percent
of
Responses
Patient
70
50.4
Family
50
36.0
17
12.2
6
1.4
Patient
&
Family
Unknown
TOTAL
143
100%
While data from the questionnaire was supplied by
respondents, it is important for the reader to recognize
that patient characteristics data (age, sex, living arrangement, primary and secondary diagnosis) was obtained
31
from the patient's record and describes the patient who
directly received the horne health services.
Patient Characteristics.
A comparison of the
Valley patient characteristics, with those of Los Angeles
patients, reveals minor differences (Table 4).
The Los
Angeles sample included about 6 percent more females and
a little more than 6 percent more patients in the over-60
age group, than the Valley sample.
There was only a small
difference in numbers living alone (less than 3 percent).
The biggest difference was in the number living with an
older person or a younger person.
Los Angeles patients
were 13 percent more likely to live with an older person
while Valley patients were about 13 percent more likely
to be living with a younger person.
Los Angeles patients
had a higher incidence of heart and circulatory problems
(6%), CVA (3%) but were 6 percent less likely to have
musculo-skeletal problems and 4 percent less likely to
have diabetes.
Discussion.
The higher percentage of over 60-
year-olds in the Los Angeles area may be a result of population distribution, as a higher concentration of elderly
people are reported to live in the Los Angeles office
area.
Studies show that in an elderly population there
is usually a higher percentage of women and a higher
32
Table 4
Comparison of the Characteristics of Patients
in Sample by Office and Totals
Patient
Characteristics
Valley
Office
N = 102
%
N
Sex:
Male
Female
Unknown
36
65
1
36
64
Age:
Under 40
40-59
60-80
Over 80
Unknown
3
10
57
31
1
3
10
56
31
Total over 60
LA Office
N = 41
N
%
12
28
1
30
69
3
26
12
7
63
29
86.27
Combined
Offices
N = 143
%
N
48
93
1
34
66
3
13
83
43
1
2
9
58.5
30
92
88.11
Living Arrangement:
Alone
With older person
(over 60)
With younger person
Deceased
Unknown
27
33
27.3
33.3
10
19
25
47.5
37
52
26
37
23
16
3
23.2
16.2
4
7
1
10
18.8
27
23
19
16
23
19
4
8
9
22.5
18.6
3.9
7.8
8.8
12
7
1
3
5
29
17
2
7
12
35
26
5
11
14
25
18
4
8
10
10
6
21
2
9.8
5.9
20.6
2.0
3
1
6
3
7
2
15
7
13
7
27
5
9
5
19
3.5
Primary Diagnosis:
Heart & Circulatory
Cancer
Urinary incant.
Respiratory Insuf.
CVA
Decubitus
Post-op Wound
Diabetes
Musculo-skeletal
Other
33
incidence of heart and circulatory problems.
Considering
age of population distribution, it appears that there is
a great deal of similarity in the two sample groups, suggesting that sampling error is low.
For the remainder of the study, the study sample
will be examined as one unit; the total number of patients
from both offices, unless stated otherwise.
Overall study sample characteristics show strong
similarities with those of patients in a national study
in 1978 which involved 11,182 patients from 19 agencies
across the nation (25:3-7).
Table 5 shows identical percentages of male and
female distribution.
Although slightly different age
intervals are reported, both groups still had between 50
and 60 percent in the
~0
to 80 year age range.
percent more of the study sample (32%)
in the national study (29%).
Only 3
lived alone than
34
Table 5
Patient Characteristics of Sample and
National Study (1978)
Patient Characteristics
Sex:
Age:
Percent of
Sample
Percent of
National Study
(1978)
Male
34
34
Female
66 •
66
60-80 years
59
50
63-81 years
32
29
Heart and Circulatory
25
27
Neoplasms
18
13
Musculo-skeletal
19
8
Living Alone:
Primary Diagnosis:
CHAPTER IV
RESULTS OF THE STUDY
This chapter presents and discusses data obtained
from the survey questionnaire pertaining to specific questions stated in the purpose of the study.
Analysis and
discussion of the Management Advisory Committee's ratings
is also included.
Part I will look at the data for answers to the
first question.
Do home health consumers feel that they are
receiving comprehensive and quality services?
Part II will examine perceived needs and
unperceived needs, for an answer to the second question.
Are the needs of the home health consumer
being met?
Part III will present and discuss the Management
Advisory Committee's rating of
th~
data examined in Part
I and Part II.
Part I.
Quality of Care Responses
Items associated with quality of care were
structured under three main components; teaching, delivery
of services, and quality of professional staff.
associated with these components were
35
Variables
36
Teaching
Self-help encouraged
Technique
Effectiveness
Additional Information Desired
Delivery of Services
Reliability
Coordination
Time of Delivery
Quality of Professional Staff
Nurse
Home Health Aide
Physical Therapist
Occupational Therapist
Speech Therapist
Medical Social Worker
The following tables list these variables, number of
responses, frequency percentage responses and mean rating
of the sample responses by Management Advisory Committee.
Table 6 shows that 91 percent agreed that the patients
were encouraged to help themselves as much as they were
able, that 4.5 percent were undecided and that 1.5 percent
disagreed.
High quality of teaching techniques was agreed
on by 92 percent of the respondents.
were undecided or disagreed.
Less than 3 percent
A much higher percentage
Table 6
Consumer Perceptions of Patient Teaching
Questionnaire
Item #
Teaching Variables
#6
#7
#8
Self help encouraged
Technique
Effectiveness
#9
Additional Information
Diet
Treatment
Equipment
Drugs
Number
Respondents
133
137
123
Mean
Percentage Percentage Percentage Percentage
Not
Rating
Agree
Undecided
Disagree Applicable Score*
91
92.0
82.1
4.5
2.2
10.6
1.5
2.9
2.4
3.1
2.9
4.9
1.1
1.1
1.4
Percent of Sample
11
16
1
15
Yes
Yes
Yes
Yes
7.7
11.2
.7
10.5
2.2
2.3
1.5
2.0
*Ratings done by Management Advisory Committee are rated on a scale of 1-5.
v.
.....
38
(10.6) were undecided about teaching effectiveness
although the percentage who disagreed was slightly less
than for teaching techniques.
rate
(10~14
A lower consumer response
less) was also noted.
Discussion.
Wording of the question (Item 8) may
have suggested that professional staff would outline the
"course of an illness"--a procedure unlikely to be carried
out due to the unpredictable nature of many illnesses.
It is unclear how respondents rated the first three teaching variables when the health status of the patient restricted teaching efforts.
Did they rate how family mem-
bers were taught, or did they just not respond?
Two
written responses stated "patient was unable" and "patient
too sick."
A "not applicable" alternative would have been
helpful in interpretation of responses to Item 8.
Additional information was desired by a number of
respondents.
Eleven were interested in diet information,
16 in treatment, and 15 in drug information.
needed information about equipment.
One person
Cross tabulations
were made between "respondents" and "information desired"
to examine who desired what information.
Although num-
bers were too small to generalize findings to the sample
population, some interesting differences were noted
(Table 7).
Twice as many "patient" respondents (55%)
wanted additional information on diet and treatment than
Table 7
Respondent by Interest in Additional Information
Additional Information Desired
Respondent
Diet
Respondent
N
%
Treatment
%
N
%
N
Equipment
%
N
Drugs
%
N
Patient
70
49
6
55
8
50
1
100
3
20
Family
50
35
3
27.2
4
25
0
9
60
Patient & Family
17
12
1
9.09
3
18.75
0
---
2
13.33
6
4
1
9.09
1
6.25
-
--
1
6.67
1
100%
Other & Unknown
Total
143
100%
11 100%
16 100%
15 100%
w
\.0
40
did "family member" respondents.
However, three times as
many family member respondents wanted additional information about drugs than did "patient" respondents (60%).
Interest in treatment information was indicated by 11
percent of the study sample, followed closely by an interest- in drug information by over 10 percent.
Discussion.
Cross tabulations were computed for
"information desired .. by "primary diagnosis."
Since most
patients had more than one medical condition the results
were misleading and are not included.
A study done of
the general public on a group of people over the age of
45 reported that 22 percent of them would like to have
more information about diet, showing more interest in
diet information than the sample population (40:37).
Data describing delivery of service is presented in Table
8.
Ninety-one percent of the consumers felt they could
rely on staff visits most of the time, 6 percent some of
the time, and only 2 percent felt that the staff were
seldom reliable.
Adequate coordination of multiple ser-
vices was accomplished most of the time according to 75
percent of those who responded, 6.6 percent reported satisfaction some of the time and 2 percent felt that services had not been coordinated well.
Many patients do
not receive multiple services as indicated by 15.6 percent,
who reported that it was not applicable.
This probably
Table 8
Consumer Perceptions of Delivery of Services
Item #
Delivery of Service
Variables
Number
Respondents
Percentage
Response
Percentage
Response
Percentage
Response
Percentage
Response
most of
time
some of
time
seldom
not
applicable
Mean
Rating
Score*
#10
Reliability
136
91.2
5.9
2.2
7.1
1.6
#11
Coordination
122
75.4
6.6
2.5
15.6
2.1
#12
Inconvenient Hours
10
Yes
1.7
*Ratings done by Management Advisory Committee are rated on a scale of 1-5.
*'"
1--'
42
accounted for a lower response rate.
One respondent who
rated coordination of services negatively wrote that the
"patient was critically ill" and too tired for physical
therapy visits.
Ten people felt that the staff arrived
at inconvenient hours.
A high level of satisfaction with professional
staff was expressed (Table 9).
Professional nurses were
rated "very good" by 96.2 percent, satisfactory by 3.8
percent, and no one considered them unsatisfactory.
Discussion.
High ratings of professional staff
are consistent with those found in studies by Schutz
(40:113).
The quality of Horne Health Aide was agreed to be
very good by 79.1 percent.
The same percentage (10.4) of
respondents felt that quality was "satisfactory" as those
who felt that quality was "unsatisfactory."
Discussion.
Dissatisfaction is a result of unrnet
expectations (24:153).
There were respondents whore-
ported that they expected housekeeping, shopping and
transportation services; perhaps services they expected
of a Horne Health Aide.
One respondent wrote disparagingly
of a Horne Health Aide but an investigation revealed that
he was referring to a homemaker-chore person from
another agency.
Table 9
Consumer Perceptions of Quality of Professional Staff
Questionnaire
Item #
#12
Quality of
Professional
Staff Variables
Number
Respondents
Percentage
Response
Percentage
Response
Percentage
Response
Mean
Rating
Score*
N
very
good
satisf.
unsat.
104
96.2
3.8
--
Home Health Aide
67
79.1
10.4
Physical Therapist
46
91.3
8.7
Occupational
Therapist
3
67.0
--
33.0
2.9
Speech Therapist
5
--
---
1.2
13.1
2.4
Nurse
Medical Social
Worker
32
100.
65.6
31.2
10.4
--
1
1.8
1
* Ratings done by Management Advisory Committee are rated on a scale of 1-5.
*""
w
44
Physical therapists were also perceived to be
"very good" (91.3%) with 8.7 percent seeing them as "satisfactory" and no one giving them an unsatisfactory rating.
High ratings again are consistent with literature
cited above (40:113).
Only 2 percent of the sample received Occupational
Therapy and 3.5 percent Speech Therapy.
One consumer
rated the quality of the Occupational Therapist "unsatisfactory.
n
Medical social workers were rated "-very good"- by
65.6 percent of those who had received services, while
31.2 percent felt that their performance was only satisfactory and 3 percent were dissatisfied.
Discussion.
Again higher levels of expectation
may be related to levels of satisfaction (24:153).
response rate to this question was noted.
A low
Although 39
respondents indicated that they had received medical
social services only 32 rated this item.
Patients' rec-
ords indicate that 69 patients in the sample had actually
received their services.
This lack of awareness could be
due to the fact that in some cases only one visit was made.
It is possible also that the person receiving the visit
was different than the person responding to the questionna,ire.
45
Part II.
Consumer Needs Responses
Consumer needs were structured under two main
categories, Health Education Needs (consumer awareness of
services) and Supportive Service Needs (consumer needs}.
Variables analyzed were
Health Education Needs:
Needed more information before discharge
(Item 2, Part III)
Knew why eligible for services (Item 4)
Knew reimbursement source (Item 5}
Expected services not available (Item 7)
Supportive Service Needs:
Transportation (Item 16)
Psychological help (Item 16)
Housekeeping (Item 16)
Shopping (Item 16)
More visits (Item 16)
Willingness to attend group support
meetings (Item 18)
Table 10 presents data on the variables associated
with Health Education Needs.
Fifty-three percent felt
that they would have been helped by "having a better
understanding" about home health services at time of
discharge.
Table 10
Health Education Needs
Questionnaire
Item #
Health Education Variables
N
Percentage
Response
Yes
Percentage
Response
No
#2
Needed more information before
discharge
77
#4
Knew why eligible for services
134
87.3
12.7
1.8
#5
Knew reimbursement source
140
77.8
22.2
2.1
94
18.1
81.9
2.2
#17
Expected services not available
53
Mean
Rating
Score*
1.9
* Ratings done by Management Advisory Committee are rated on a scale of 1-5.
.j::.
0"\
47
Discussion.
Since many of the patients are
readmissions and already are aware of services, one might
suspect that more than 53 percent of first time patients
need to know more about potential services.
A poignant
message was written by one respondent.
Wish I knew of Horne Health Services.
I found
out about it on my mother's last day in hospital
and nurse found me crying.
I did not want my
mother sent to a convalescent hospital.
To the question regarding eligibility, 12.7
percent of the respondents did not respond or responded
incorrectly.
As long as one appropriate criteria for
eligibility was identified, no penalty was assessed for
also checking secondary services such as social services
or occupational therapy.
An even larger 22.2 percent of
respondents did not accurately know how horne health services were paid for.
The largest misconception occurred
among the elderly who were eligible for Medicare A and B
and Medi-Cal.
Medi-Cal was credited with providing reirn-
bursernent much more frequently than it actually does.
Inappropriate expectations (services expected
for which horne health agencies are not reimbursed) were
held by 18.1 percent of those who responded to Item 17.
Table 11 shows the relationship between
respondents and lack of awareness of horne health services.
Half of those who wanted more information about horne
health services were the patients themselves (50%).
A
Table ll
Relationship of Survey Respondents to Health Education Needs
Understand
Home Health
Respondent
Did not know
eligibility
Did not know
Reimbursement
N
%
N
%
N
%
Patient
70
49
24
50
9
53
14
45
ll
65
Family
50
35
18
38
6
35
10
31
3
17
Patient & Family
17
12
4
8
2
12
5
16
2
12
6
6
2
4
-
--
2
6
l
6
143
100
48
100
17
100
31
100
17
Unknown
N
Faulty
Expectations
%
N
%
100
,j::..
00
49
slightly larger percentage (53%) did not know why they
were eligible for home care and a slightly smaller percentage (45%) did not know how services were paid.
The
biggest difference in respondent awareness was that 65%
of those who expected services that are not covered, were
"patient" respondents.
Needs for supportive services were perceived and
unmet as indicated by 83 responses from the study sample.
Some consumers perceived need for more than one supportive
service (Table 12).
The most prevalent need was perceived
for more visits (16.8%).
Other needs were housekeeping
(14.7%), transportation (11.9%), shopping (8.4%) and
psychological help (6.3%).
Discussion.
Stringent regulations regarding
criteria_ for visit reimbursement, limit the agency from
providing additional visits.
(It was observed that the
agency provided visits, free of charge, when needs were
urgent and patient did not meet the eligibility requirement for reimbursement.)
Housekeeping, transportation,
shopping and psychological help are also services for
which home health agencies are not reimbursed.
Studies show that lifestyle and needs are highly
related (40:153).
Living arrangements of patients were
cross tabulated with supportive services needs (Table 13).
Of those who needed more visits, 42 percent live alone.
Table 12
Supportive Service Needs
Questionnaire
Item #
Supportive Services Needed
#16
Transportation
#16
Psychological Help
#16
Number
Responses
Percent
of
Sample
Mean
Rating
Scores*
17
11.9
2.0
9
6.3
1.8
Housekeeping
21
14.7
1.9
#16
Shopping
12
8.4
1.7
#16
More visits
24
16.8
1.8
Total Services Needed
83
* Ratings by Management Adivisory Committee are rated on a scale of 1 to 5.
1 - - -
very acceptable
-
- - -
5
unacceptable
U1
0
Table 13
Relationship of Living Arrangement with Supportive Service Needs
Living
Arrangement
N
%
Needed
Transp.
Needed
Hskpg.
N
%
N
%
Needed
More
Visits
N
Needed
Psych.
Help
Needed
Shopping
%
N
%
N
%
Alone
37
26
8
47
9
43
10
42
2
22
6
50
Older
52
36
5
29
7
33
6
25
4
44
5
42
Younger
27
19
3
18
4
19
6
25
-
--
1
8
Deceased
23
16
1
4
1
5
2
8
3
33
4
3
0
143
100
17
100
21
100
24
100
9
100
12
100
Unknown
Total
U1
1-'
52
Those who lived alone also expressed the greatest
percentage of need for transportation (47%) and housekeeping {43%) and shopping (50%).
Age and sex were examined
for their relationship to needs.
frequencies.
Table 14 presents raw
Age and sex refer to the patient's charac-
teristics but we do not know whether patient and/or family
expressed the need, hence the data is of little value.
Although the sample numbers are small, they
follow patterns similar to those in studies reported by
Schutz; the greatest needs are expressed by sick elderly
without a social support system (lived alone)
(40:124).
Only 9 people expressed need for psychological
counseling, but one-third of these were from families
where the patient was deceased (Table 15).
A willingness to attend group family meetings was
interpreted as a consumer need.
Of those responding,
42.3 percent said they would attend meetings (Table 16),
and 54 percent of this group were the patients themselves (Table 17).
Discussion.
Underlying needs which motivated
respondents to agree to attend meetings could be
Psycho-social needs - Group support
Educational - to learn more about care of patient
Informational - to exchange ideas about common
problems
Table 14
Relationship of Age by Sex by Supportive Service Needs
Needed
Transportation
Needed
Housekeeping
Needed
Psychological
Help
Male
Female
Male
Male
Under 40
-
-
-
2
-
-
-
-
-
40 - 60
1
2
3
-
-
1
3
-
2
60 - 80
4
5
2
10
3
3
1
10
2
3
80+
1
4
1
3
1
1
3
7
1
3
Totals by Sex
6
11
6
15
4
5
7
17
5
7
Age
Female
Female
Needed
More
Visits
Male
Needed
Shopping
Female
Male Female
1
Totals f0r
Both Sexes
17
21
9
24
12
Ul
w
54
Table 15
Needed Psychological Counseling by
Living Arrangements
Living Arrangement
N
%
Needed
Psychological
Counseling
N
%
Alone
37
26
2
22.2
With Older Person
52
37
4
44.4
With Younger Person
27
19
Patient Deceased
23
16
3
33.3
4
2
Unknown
Total
143
100%
9
100%
Table 16
Interest in Attending Group Support Meetings
Questionnaire
Item
#18
Would attend group
support meetings
Number
Responses
Yes
97
41
Percentage N0
Response
42.3
47
Percentage Unde- Percentage RM~~n
Response cided Response S~o~~~
48.5
8
8.2
2.2
*Ratings done by Management Advisory Committee and rated on a scale of 1 to 5.
1
very acceptable
5
unacceptable
U1
(Jl
Table 17
Identification of Respondent Interested in Group Meetings
Would Attend Group Meetings
Respondent
%
N
% of Responses
N
Patient
70
49.0
22
53.7
Family
50
35
16
39
Patient and Family
17
11.9
Other
2
1.4
Unknown
4
2.8
Totals
143
100%
3
7.3
0
41
100%
Ul
~
57
I
Problem solving - to assist with problems
Although some dissatisfaction with services was
expressed and many needs were unfulfilled, an overall
positive attitude toward home health services in general
was indicated.
Responses to Item 15 showed that 96.7 per-
cent of those who responded agreed that the advantages of
receiving health care services at home outweighed the disadvantages while only 3.3 percent disagreed.
Part III.
Rating· of Consumer Responses by Management
Advisory Committee
To obtain a broader based, more objective
interpretation of the data the Management Advisory Committee was asked to rate the mean frequency percentages
of the variables in the study using the second instrument
(Appendix C).
Table 18 lists the Committee's mean rating
scores to 26 variables, the range of rating scores and
their rank.
The variables are ranked from highest mean
rating score (least acceptable) to lowest mean rating
(most acceptable)
(5 - - - - - (least acceptable)
- - - - 1).
most acceptable)
A rating of 2, or more, on a variable was selected
arbitrarily as a criteria for further examination of that
variable.
Ratings on teaching variables (1-7} ranged
from 1.1 to 2.3 with a mean rating of 1.7.
Interest in
additional information about treatment, diet and drugs
'
Table 18
Management Advisory Committee Rating of Consumer Responses to
Selected Variables
Variables
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
Teaching
Self-help encouraged
Teaching techniques
Teaching effectiveness
More information desired Diet
Treatment
Equipment
Drugs
Deliver~ of Services
Dependability of visit
Coordination of visits
Time of visits
Qualit~ of Professional
Performance
Professional Nurse
Home Health Aide
Physical Therapy
Occupational Therapy
Speech Therapy
Medical Social Service
Consumer Awareness Level
Better understanding of
Home Health Services
Knew eligibility
Knew reimbursement source
Unrealistic expectations
Su~~ort Services Needed
Transportation
Psychological help
Housekeeping
Shopping
More frequent visits
~1eet other patients • fami 1i es
Mean
Staff Rating
Score*
Range
1 - 5
Rank
1.1
1.1
1.4
2.2
2.3
1.5
2
1-2
1-2
1-2
1-4
1-4
1-3
1-5
23
23
21
4
3
19
9
1.5
2.1
1.7
1-3
1-3
1-3
19
7
17
1
1.8
1
2.9
1.2
2.4
1
1-3
1
1-5
1-2
1-5
25
13
25
1
22
2
1.9
1.8
2.1
2.2
1-3
1-5
1-5
1-5
11
2
1.8
1.9
1.7
1.8
2.2
1-5
1-4
1-4
1-4
1-3
1-3
13
8
5
10
13
11
17
13
5
*Ratings done by Management Advisory Committee are rated on a scale of
5
1
1-5.
unacceptable
very acceptable
59
received the highest ratings (least acceptable) in this
category with ratings of 2 or more.
Ratings on delivery of service variables (7-10)
ranged from 1.5 to 2.1 with a mean rating of 1.7.
Coordi-
nation of visits was rated least acceptable with a score
of 2.1.
The quality of professional performance variables
(11-16) were rated from 1 to 2.9 with a mean rating of
1.72.
Professional performances characterized by mean
scores over 2 were those of the Occupational Therapist
(ranked least acceptable) and Medical Social Worker
(ranked second).
Discussion.
Advisory committee appeared to be
least satisfied with consumer perceptions to these "quality of care" variables beginning with the least acceptable
1.
Quality of Occupational Therapist
2.
Quality of Medical Social Worker
3.
Desired information on treatment
4.
Desired information on diet
Variables 17 through 20 related to consumer
awareness assessment and had ratings from 1.8 to 2.2
with a mean rating score of 2.0.
Satisfaction with con-
sumer responses to these variables was lowest for
1.
Expected services not available (5th)
2.
Awareness of reimbursement source (8th)
60
Both had ratings over 2.
Discussion.
A wide range in staff rating on
these variables was shown by a rating range from 1-5
(highest to lowest) on three of the four variables.
Ratings on responses to variables 21 to 26
ranged from 1.7 to 2.2 with a mean rating of 1.9.
Areas
of need receiving scores of 2 or more were
1.
Willingness to meet with other families (5th)
2.
Need for transportation (lOth)
Overall mean rating scores were computed for each
of the categories discussed (Table 19).
The category
receiving the least acceptable rating from the Management
Advisory Committee was "Health Education Needs" with a
score of 2.00.
Table 19
Mean Rating Scores of Variable Categories
by Management Advisory Committee
Variable Categories
Mean
Rating
Score
Teaching
1.66
Delivery of Services
1.77
Quality of Professional
1. 72
Health Education Needs
2.00
Supporting Services Needs
1.90
CHAPTER V
SUMMARY, CONCLUSIONS, AND RECOMMENDATIONS
This chapter presents a summary of the data
analysis and consequent conclusions reached by the researcher.
It also includes recommendations for future
studies.
Summary
Responses Concerning Perceptions of Quality of
Care (Part I).
The data revealed that a very high per-
centage of health care consumers reported positive attitudes toward health care services provided in the home.
Variables reporting teaching performance were also rated
highly.
An interest in obtaining additional information
about diet, treatment, equipment and drugs was expressed
by 43 responses (more than one response could be supplied
by a respondent).
Treatment and drug information was of
most interest (12%).
While the patients themselves were
twice as likely to want treatment or diet information,
surprisingly three times as many family members registered
an interest in drug information.
A high percentage of
respondents reported that they could rely on staff visits
61
62
most of the time, a slightly smaller percent felt that
services were coordinated effectively and approximately
7 percent indicated that services were received at inconvenient hours.
An extremely high percentage (over 90%) rated the
quality of the Professional Nurse, Physical Therapist and
Speech Therapist "very good."
Home Health Aides received
the next highest percentage (79.1%) of positive responses
and Medical Social Workers received the lowest percentage,
with two-thirds of the respondents rating them very good.
Only 3 patients had received Occupational Therapy and one
reported unsatisfactory quality.
Responses Concerning Needs of Consumers (Part II).
Responses to health services awareness questions
suggeste~
directly or indirectly, that a lack of correct or comprehensive knowledge of home health services existed.
Over
one-third related that they would have been helped by
knowing more about home health services before going home
from the hospital.
Between 12 and 22 percent of the sam-
ple were unable to correctly identify how services were
paid, or to identify at least one criteria for eligibility
for services or they expected services which are not
covered by insurance plans.
Needs for a wide range of supportive services
were expressed.
Those most often reported, listed in
63
order of most services needed, were more visits, housekeeping, transportation, shopping and psychological help.
Females who lived alone reported the largest number of
needs.
A surprising 42.3 percent said they would attend
family group sharing meetings although motivation (underlying needs) for attending was not identified.
Ratings by the Management Advisory Committee gave
the highest acceptability rating (1.7) to variables associated with patient teaching, quality of professional performance came next with 1.7 and delivery of services was
rated least acceptable of the quality of care variables.
All of the components of quality of care were rated more
acceptable tham the consumer needs components.
Health
education needs were rated lowest in acceptability with
a score of 2.
Additional Considerations Regarding Consumer
Response Ratings.
Responses receiving a mean rating
score of 2.0 or more will be discussed in order of ranking beginning with the least acceptable.
A ranking of 1
is the most acceptable ranking and a ranking of 5 the
least acceptable.
1.
Quality of Occupational Therapist (2.9).
Only three people in the sample had received their services and one had rated services unsatisfactory.
An
'
'
64
occupational therapist was dismissed just prior to this
study, and patients receiving this individual's services
may have been represented in the sample.
2.
(2.4).
Quality of Medical Social Service Worker
Prior to the study there had been a turnover in
the Medical Social Service staff--again study sample patients may have received services from this person.
3.
(2.3).
More information desired about treatment
The need for a more standardized teaching format,
for nurses and/or consumers had been recognized.
During
the last six months instructional material has been developed to standardize and document teaching done by the
agency nurse for selected medical conditions.
Patient
teaching tools, including handout and taped cassettes,
have been developed also.
4.
More diet information desired (2.2).
While
this study was being conducted, a staff In-Service Education class was being conducted on diabetic care--a registered dietician taught the "diet" portion.
Actually a
dilemma exists because registered nurses are not legally
permitted to teach "diets," but only to reinforce what
has already been taught by the dieticians.
Dietician
teaching in the home is usually not covered by third party
payments.
Diet teaching is usually done in hospital when
the patient is often sick and under stress and the
I
'
65
dietician has less opportunity to understand family
habits, lifestyle and environmental conditions.
The pa-
tient may have difficulty complying with a diet where
these factors have not been considered.
5.
Unrealistic expectations (2.2).
When patients
expect services which the agency cannot provide or for
which they do not receive reimbursement, they are more
likely to be dissatisfied with services.
Factors associ-
ated with unrealistic expectations include misinformation
regarding potential services available, communication
problems caused by diminished vision, hearing or memory
function and confusion of the Home Health Aide role with
that of a Homemaker Chore Person.
(Homemaker Chore Per-
sons may be reimbursed by Medi-Cal but not by Medicare.}
6.
Meet with other patients' families (2.2).
A
surprisingly large number of respondents said they would
attend group meetings.
It was noted that a large number
who responded were the patients themselves.
Financial
reimbursement is not available to research and develop a
program which would bring together patients and/or families with common problems.
7.
Coordination of visits (2.1).
Regulations,
imposed since this study, require the nurse to regularly
supervise the Home Health Aide as she provides services
in the home.
This means that their visits will overlap
66
on the same day instead of being given on alternate days.
Services cannot be spaced as conveniently
for patients
as they were at the time of the study.
8.
Knew reimbursement source (2.1).
Health
education and promotion could reduce unrealistic expectations, increase awareness of reimbursement sources and
eligibility requirements, and increase overall knowledge
about Home Health Services.
Again insurance plans usually
do not reimburse separate charges for health education
services, but consider these services as part of other
covered provider services.
More plans reimburse for
health education services in hospital inpatient and outpatient settings than for non-hospital settings such as
physicians' offices, home care programs and skilled nursing facilities according to a survey done by Blue Cross
and Blue Shield Associations in 1980.
By using a Health
Education student trainee, consumer health education
classes have been initiated recently in a local community
senior center.
9.
More information desired on drugs (2).
The
physician who prescribes the drugs should be responsible
for providing a clear and comprehensive description which
should include their use, effect on patient and side
effects that may occur.
Nurse responsibilities include,
67
knowing what drugs are being used, to observe and
encourage compliance, and to monitor for side effects.
10.
Transportation (2).
Transportation is not
a service provided by home health agencies.
They do pro-
vide resource information regarding transportation to the
consumer.
A community resource guide was updated recently
and is distributed to all agency consumers.
Limitations and Weaknesses
of the Study
Related to attitudinal surveys
1.
Reluctance to express dissatisfaction
2.
Reluctance of older people to admit needing
help
3.
Function of who sponsors the research
4.
Exclusion of data collection on socio-economic
and psychological factors (all affect
attitudes)
5.
( 29 :285)
People report quality of care they receive
themselves higher than the quality of care
they think that others receive (44)
Related to Instrument and its Implementation
1.
Degree of reliability
2.
Complexity of patient and family-centered
interdisciplinary independent variables-difficult to interpret
68
3.
Amount of time between services received and
completion of questionnaire
4.
Language barriers to non-English speaking
population
5.
Inability to collect more data on nonrespondent perceptions
Conclusions
On the basis of the data presented in this study,
ratings of the data by health professionals, and a review
of the literature the following conclusions appear
warranted:
1.
A large proportion of horne health care
consumers who have received services from National InHorne Health Services feel they are receiving comprehensive
and quality services.
2.
Many supportive service needs, as perceived
by the horne health care consumers are not being met by
existing services available in the study area.
(These
services are not provider reimbursed.)
3.
Many consumers and potential consumers are
unaware of the potential services available to them from
a horne health care agency.
4.
The percentage of consumers who reported
they would attend family group support meetings was
larger then expected.
69
5.
Comprehensive empirical up-to-date data on
perceptions of the elderly health care consumer are very
scanty.
6.
Methodologies for collecting and assessing
quality of care data in a home setting are lacking.
7.
Based on personal discussion and observation,
most of the above conclusions represent already held beliefs and assumptions held by agency staff personnel ana
many recommendations which follow are already being discussed or implemented.
This study provided objective
support to their beliefs.
Recommendations
On the basis of this study these recommendations
are suggested:
1.
An expansion of the study be undertaken to
determine the extent and true nature of perceived needs
before planning strategies are modified.
The following questions need to be explored:
a.
Are the elderly able to assess their own
needs?
b.
What is the extent and degree of need?
c.
Should programs be planned to fill this
need?
d.
Why are they not able to use available
resources?
70
1) Were the services not available
geographically?
2) Were they unaware of resources or
unable to initiate resource
acquisitions?
3) Were there financial limitations?
4) Were there physical limitations?
5) Were they inhibited by cultural or
generational beliefs?
2.
A comprehensive health education and health
promotion curriculum related to Home Health Care Services
should be developed for use in community settings.
The
encouragement of patient responsibility for his own
health including evaluation of services received, should
be one of the goals of such a program.
Modification of
the curriculum for use by the individual consumer in the
home, in the doctor's office, or in the hospital setting
should be considered.
3.
An expansion of the study to include an in-
depth investigation of the interests and common problems
of consumers who would attend family group support meetings.
Based on results of the investigation, the develop-
ment and implementation of a family support group program
should be attempted.
71
.I
4.
If a similar study should be conducted,
patients' perceptions of home health services should be
collected as soon as possible after services are received
to obtain more accurately remembered data and increase
the chances of locating the patient.
If a mailed ques-
tionnaire approach is contemplated, a telephone verification of patients' health status and address would increase
the response rate of the sample.
5.
Organization of a task force made up of
representatives of areawide Home Health Agencies to
develop a standardized instrument or procedure to be used
to obtain consumer perceptions of care on an on-going
basis should be explored.
BIBLIOGRAPHY
1.
Aaker, David A. & George A. Day, ed., Consumerism:
Search for the Consumer Interest, 2d. ed., New
York: The Free Press, 1974.
2.
American Hospital Association, A Patient's Bill of
Rights, House of Delegates of the American
Hospital Association, No. SOm-11/73-3493,
Chicago, 1972.
3.
Atchley, Robert D., The Social Forces in Later Life:
An Introduction to Social Gerontology, Miami
University, Oxford, Ohio, 1972.
4.
Bengston, Vern L., Patricia L. Kasschau and
Pauline K. Ragan, Handbook of the Psychology of
Aging, edited by James E. Birren and K. Warner
Schaie, Van Nostrand Reinhold Company, New York,
1977.
5.
Birren, James E. and K. Warner Schaie, Handbook of
the Psychology o-f Aging, Van Nostrand Reinhold
Company, New York, 1977.
6.
Bloom, Martin, Edna Duchon, Gertrude Frires, Helen
Hanson, Georgine Hurd, and Vivian South,
"Interviewing the Ill Aged," The Gerontologist,
Part 1, pp. 292-299, Winter 1971.
7.
Botwinick, Jack, Aging and Behavior, 2d ed., New
York: Springer Publishing Company, 1978.
8.
Boyd, Harper W., Ralph Westfall, and Stanley F.
Stasch, Marketing Research Text and Cases, 4th
ed., Homewood: Richard E. Irwin, Inc., 1977.
9.
Brickner, Philip W., Home Health Care for the Aged,
New York: Appleton-Century-Crofts, 1978.
10.
Claubaugh, Maurice F., Jr., "An Investigation of the
Role of Consumer Alienation on Consumer Dissatisfaction and Compliant Behavior," Proceedings 25th
Annual Conference of the American Council on
Consumer Interests, April, 1979.
72
73
11.
Department of Health, Education and Welfare Grant
#HSA 77-88(P), A Prospectus for a National Home
Care Policy, April 1977.
12.
Greene, Richard, M.D., Assuring Quality in Medical
Care, Ballinger Publishing Company, Cambridge,
Mass., 1976.
13.
Griffith, Elsie, "Administrative Perspective on
People Power - Community Health Viewpoint,"
People Power, National League for Nursing,
Pub. No. 20-1623, 1976.
14.
Gross, Deborah Ann, Patients• Perceptions Toward
Medical Care, Thesis Project, June 1978.
15.
Hochbaum, G. M., "Consumer Participation in Health
Planning Toward Conceptual Clarification," The
Consumer and the Health Care System, edited by
Rosen, Metsch and Levey, 1977.
16.
Home Health Review, Journal of the National
Association of Home Agencies, 2:1, January 1979.
17.
Hyman, Herbert Harvey, Health Planning: A
Systematic Approach, Aspen Systems Corporation,
Germantown, 1976.
18.
Institute of Medicine, Aging and Medical Education,
Report of a Study by a Committee of the Institute
of Medicine, National Academy of Sciences,
Washington, D.C., 1978.
19.
Institute of Medicine, Assessing Qualit¥ in Health
Care: An Evaluation, Report of a Study, National
Academy of Sciences, Washington, D.C., November,
1976.
20.
Isaac, Stephen and William B. Michael, Handbook in
Research and Evaluation, San Diego: Edits
Publishers, 1977.
21.
Journal of the National Association of Home Health
Agencies, Suite 200, 426 "C" Street, N.E.,
Washington, D.C., 1979.
22.
King, Stanley H., Perceptions of Illness and Medical
Practice, New York: Russell Sage Foundation,
1962.
74
23.
Kerlinger, Fred N., Foundations of Behavioral
Research, 2d. ed., New York: Holt, Reinhart
and Winston, Inc., 1964.
24.
Kotler, Philip, Marketing for Nonprofit
Organizations, New Jersey: Prentice-Hall, Inc.,
1974.
25.
Levenson, Goldie, "Use of Patient Statistics for
Program Planning," National League for Nursing,
Pub. No. 21-1794, New York, 1979.
26.
Levin, Tom, American Health: Professional Privilege
vs. Public Need, Praeger Publishing, 1976.
27.
McDaniel, James W., Physical Disability and Human
Behavior, Second Edition, Pergamon Press,
New York, 1976.
28.
McFarland, Ross A., "The Sensory and Perceptual
Processes in Aging," Theory and Methods of
Research on Aging, edited by K. Warner Schaie,
Ph.D., West Virginia University, Morgantown, 1968.
29.
McKinlay, John B. and Diana B. Dutton, "SocialPsychological Factors Affecting Health Service
Utilization," edited by Selma J. Mushkin, Prodest,
New York, 1974.
30.
Miller, Delbert C., Handbook of Research Design and
Social Measurement, 3d. ed., New York: David
McKay Company, Inc., 1977.
31.
Noelker, Linda and Zev Harel, "Aged Excluded from
Home Health Care," The Gerontologist, Vol. 18,
No. l, 1978.
32.
Novello, Dorothy Jean, "The Consumer's Role in
Health Care," Consumerism and Health Care, compiled by National League for Nursing, Publication
No. 52-1727, 1978.
33.
Parlow, Jack, and Arthur I. Rothman, "ATSIM: A
Scale to Measure Attitudes Toward Psychosocial
Factors in Health Care," Journal of Medical
Education, 49:385-87, April, 1974.
34.
Parten, Mildred, Surveys, Polls, and Samples:
Practical Procedures, Cooper Square Publishers,
Inc., New York, 1966.
75
35.
Reeves, Philip N., David F. Bergwell and Nina B.
Woodside, Introduction to Health Planning,
Information Resources Press, Washington, D.C.,
1979.
36.
Richmond, Julius B., "Health Promotion and Disease
Prevention in Old Age," Aging, pp. 11-15,
October 1978.
37.
Rooke, M. Leigh, and C. Ray Wingrove, Benefaction or
Bondage? Sound Policy and the Aged, University
Press of America, Washington, D.C., 1980.
38.
Rosen, Harry, Samuel Levey and Jonathan M. Metsch,
editors of The Consumer and the Health Care Syste~
Spectrum Publications, Inc., New York, 1977.
39.
Schmidt, Mary Gwyne, "Interviewing the 'Old Old',"
The Gerontologist, December, 1975.
40.
Schutz, Howard G., Pamela C. Baird and Glenn Hawkes,
Lifestyles and Consumer Behavior of Older
Americans, New York, Praeger Publishing, 1979.
41.
Shanas, Ethel, Medical Care Among Those Aged 65 and
Over, Health Information Foundation, University ·
of Chicago, 1960.
42.
Shrifter, Norman, "The Physician and Home Health
Care- Costs are Less and Patients Feel Better,"
Los Angeles County Medical Association Physician,
pp. 23-26, October 6, 1980.
43.
Siemiatycki, Jack, "A Comparison of Mail, Telephone
and Home Interview Strategies for Household
Health Surveys," American Journal of Public
Health, 69:3:238:245, March, 1979.
44.
Snyder, Mary K. and John E. Ware, Jr., Differences
in Satisfaction With Health Care Services as a
Function of Recipient: Self or Others, The Rand
Corporation, Santa Monica, CA, 1975.
45.
Strauss, Anselm L., Chronic Illness and the Quality
of Life, The C. v. Mosby Company, St. Louis, 1975.
46.
Thompson, John D., Applied Health Services Research,
D. C. Heath and Company, Lexington, Massachusetts,
1977.
76
47.
Towles, Bonnie, "Consumer Involvement in Health
Offices," Evaluation in Health Services Delivery,
Proceedings of an Engineering Conference, South
Berwick, Maine, Aug. 19-24, 1973.
48.
u.s.
49.
u.s.
50.
u.s.
51.
u.s.
52.
u.s.
53.
U.S. Department of Health, Education and Welfare,
Health Resources Administration, ~orking With
Older People, Volume II. Biological and Sociological Aspects of Aging, Public Health Service
Publication No. 1459-Vol. II, Washington, D.C.,
1974.
54.
U.S. Department of Health, Education and Welfare,
Task Force on Research and Evaluation, IntraDepartmental Panel for Health Education of the
Public, u.s. Department of Health, Education and
Welfare, Public Health Service, Center for
Disease Control, March 4, 1976.
Congress - PL 93641.
Department of Commerce, Bureau of the Census:
Current Population Reports: Social and Economic
Characteristics of the Metropolitan and Nonmetropolitan Population, 1974 and 1970. Washington, D.C., u.s. Government Printing Office,
Series P/23, No. 55, 1975.
Department of Health, Education and Welfare,
Administrators Handbook for the Structure,
Operation, and Expansion of Home Health Agencies
by National League for Nursing, Health Services
Administration, Bureau of Community Health
Services, HSA contract Number 76-116, 1977.
Department of Health, Education and Welfare,
Your Medicare Handbook, DHEW Publication No.
(SSA) 74-10050, Washington, D.C., 1975.
Department of Health, Education and Welfare,
Assessment Approaches; Concepts and Methods.
Alcohol, Drug Abuse & Mental Health Administration, A Working Manual of Sample Program Evaluation Techniques for Community Mental Health
Centers, P.H.S. Publication No. (ADM) 77-472,
printed 1977.
77
55.
Ware, John E., Jr., Mary K. Snyder and W. Russell
Wright, "Some Issues in the Measurement of
Practical Satisfaction with Health Care Services,"
The Rand Corporation, Santa Monica, CA, November,
1977.
56.
Western Regional Health Forum, "Making the Health
Care System More Accountable," National Health
Council, New York, N.Y., 1974.
57.
Wiseman, Frederick, "Methodological Bias in Public
Opinion Surveys," Public Opinion Quarterly,
36:105-108, 1972.
58.
Weinerman, Richard E., "Patients' Perception of
Group Medical Care," American Journal of Public
Health, LIV, No. 6, 880-889, June, 1964.
59.
Wilson, Cindy c., The Perceived Need for Home Health
Care of the Elderly as Stated by Both the Elderly
and Health Professionals, Ann Arbor, MI,
University Microfilms International, 1979.
60.
Wolfe, Samuel, "Consumerism and Health Care,"
Public Administration Review, p. 528, September/
October, 1971.
61.
Yaffe, Richard and David Zalkind, Editors,
Evaluation in Health Services Delivery, Proceedings of an Engineering Foundation Conference,
Engineering Foundation Conferences, New York,
N.Y., 1973.
'j
APPENDIXES
78
79
APPENDIX A
NATIONAL IN-HOME
HEALTH SERVICES
6850 VAN NUYS BOULEVARD • VAN NUYS. CALIFORNIA 91405 • (213) 988-7575 • (213) 873-5555
BRANCH OFFICE
432 SOUTH SAN VICENTE BOULEVARD • LOS ANGELES. CAUFORNIA 90048 • (213) 855-1344
Dear Patient and/or Family:
We need your help!
The staff at National In-Horne Health Services is concerned with
providing the best possible care to its patients and the community.
Your_participation in a patient survey will assist us in evaluating
and planning future services for you and your fellow patients.
The enclosed questionnaire has been designed to answer some of
the questions that we have about how you, the patient,
family)
(and or
feel about the services which you have received from us in
the past year.
It would be greatly appreciated if you would complete these forms
and return them to us within a week in the enclosed self-addressed,
stamped envelope.
All information will be kept confidential; sign-
ing your name is optional.
If you have questions, please call me
at 988-7575 or 873-5555.
Thanks for your help.
Charlotte Laubach, R.N., B.S.
80
APPENDIX B
This form is being completed by:
1.
patient
II
patient & family
family
1
other
I
1
I
At time of discharge from hospital:
I had been visited by someone from the
National In-Home Health Services staff
Yes I~
All necessary equipment was available at home
Yes
Noli
I
No I
I
If no,what was missing?
2.
Preparation for going home from hospital could have been
improved by:
Earlier notification of discharge
Yes
I
I
No
I
I
Better understanding of how to care for myself
at home
Yes
I
I
No
I
j
Better understanding of home health services
Yes
I
No
0
Yes
I
No
I
Other
(please specify)
3.
4.
Have you ever received services from another home
health agency?
I was eligible for in-home health services because I needed:
check appropriate answers)
Services of RN/LVN
c=J
Physical Therapy
Occupational Therapy I
I
c=J
(Please
Social Services
Speech Therapy
I
c:J
t=J
Other
(please specify)
5.
Home health services were paid for by:
Medicare
County Agency
6.
D
D
Medi-Cal
I
·
Private Insurance
Private Pay
I
I
Other
c=J
National In-Home Health Services staff encouraged me to be involved in
caring for myself as much as I was able.
(Please check appropriate answer)
Agree
7.
(Please check appropriate answer)
0
Undecided I
I
Disagree
I::=J
Teaching and explanation was done in a clear unhurried manner with
adequate time provided to understand and practice.
(Please check
appropriate answer)
Agree
I:::::=:J
Undecided
i:::::=:J
Disagree
II
81
8.
Following teaching I had a better understanding of my illness and
what to expect in the course of it. (please check appropriate
answer)
I:=J
Agree
9.
Undecided
0
Disagree
I would have liked more information about my:
appropriate answers)
Diet
0
Treatment
D
Equipment
0
(please check
0
Drugs
I
I
Other
(please specify)
10.
I knew approximately when to expect a visit from the staff and was
notified if time of visit had to be changed.
(please check
appropriate answer)
c:J
Most of the time
ll.
c:J
Some of the time
I
I
Seldom
0
The quality of care I received at horne was (check only those
services which you received)
by:
Satisfacto=::l
Unsatisfactorv
D
Professional Nurse
0
I
Horne Health Aide
I:=J
I:=J
I=:J
Physical Therapy
r:l
I=:J
I
Occupational Therapy
D
D
l_j
Speech Therapy
I
C:J
I
Medical Social Service
D
l_j
II
Advantages of horne care included:
Convenience for family
Financial savings
14.
c:J
Seldom
multiple services were provided there was sufficient spacing
so that I was not overtired when staff arrived.
(please check
appropriate answer)
Very Good
13.
c:J
~fuen
Most of the time
12.
Some of the time
0
c:J
I
Relaxing atmosphere for patient
Family companionship
I::J
D
Other
I::J
Staff visits at inconvenient hours
List others
I
(please check appropriate answers)
Worry regarding medical condition of patient
c:J
I
(please check appropriate answers)
Disadvantages of home care included:
Financial hardship
I
I
I
82
15.
Advantages of horne care outweighed the disadvantages:
check appropriate answer)
Agree
16.
0
0
Disagree
0
What services did you need but not receive during horne convalescence?
(please check appropriate answers)
Transportation
Shopping
0
c:J
Psychological Help
I
I
Housekeeping
More Frequent Nursing/Therapy Visits
Community Referrals
17.
Undecided
(please
0
0
C::l
List others
Did you expect the agency to provide any of the above
Yes
c:J
No
If yes, please specify
18.
As a family member, if you had the opportunity to meet with other
patient's families, to share problems and experiences, would you
Yes
come?
19.
Were you given enough notice before discharge
from the agency?
Not applicable
Yes
c:J
I::=J
No I
D
NoQ
Additional comments and/or recommendations are welcomed
I
c:J
83
APPENDIX C
March 30, 1981
Dear
Many months ago you suggested information which you were
interested in obtaining from the patient and/or families who
have received services from National In-Home Health Services.
You also provided valuable input and feedback in the construction and revision of a questionnaire to acquire this data.
I am asking for your help again with the evaluation of
the questionnaire responses in terms of their level of acceptance with you, as a staff member.
Enclosed is a copy of the demographic data of the sample
tested, which appears to be representative of the patient population as a whole. I recognize that the variables associated
with the responses are complex and difficult to assess, but
would appreciate your overall rating of each response.
Thanks for your help.
Sincerely,
Charlotte Laubach
Enclosure
84
Responses are given in percentages, based on the number of responses reported.
Please rate each response on a continuum scale from 1
5.
1
3
4
2
5
very acceptab 1e
totally unacceptable
Please evaluate the responses independently from other staff members.
A.
Consumer Ratings on Components of Quality Health Care Services
No. of
Responses
Teaching:
1.
National In-Home Health Services staff encouraged me to
be involved in caring for myself as much as I was able.
agree 91.0 undecided 4.5
2.
B.
133
undecided 2.2
disagree 2.9
NA 2.9
137
Following teaching I had a better understanding of my
illness and what to expect in the course of it.
agree 82.1
4.
1.5 NA 3.1
Teaching and explanation was done in a clear unhurried
manner with adequate time provided to understand and
practice.
agree 92.0
3.
disagree
undecided 10.6
disagree 2.4 NA 4.9
123
I would have liked more information about my:
5.
Diet
26.8
11
6.
Treatment
39.0
16
7.
Equipment
2.4
1
8.
Drugs
36.6
15
Delivery of Services:
9.
I knew approximately when to expect a visit from the
staff and was notified if time of visit had to be
changed.
most of the time 91.2 some of the time 5.9
10.
seldom 2.2
NA 7.1
136
When multiple services were provided there was sufficient
spacing so that I was not overtired when staff arrived.
most of the time 75.4 some of the time 6.6 seldom 2.5
NA 15.6
122
Staff
Rating
1 - 5
85
- 2 No. of
Responses
11.
Disadvantages of home care included:
Staff visits at inconvenient hours - positive Responses
C.
10
Quality of Professional Performance:
The quality of care I received at home was:
D.
Satisf.
12.
Profession a 1 Nurse
96.2
3.8
13.
Home Health Aide
79.1
10.4
14.
Physical Therapy
91.3
8.7
15.
Occupational Therapy
67.0
16.
Speech Therapy
17.
Medical Social Service
Unsatisf.
104
10.4
67
46
33.0
100
3
5
65.6
31.2
3.1
32
Consumer Awareness of Home Health Services:
18.
Preparation for going home from hospital could have been
improved by better understanding of home health services.
yes
19.
20.
no
37.7
77
87.3
no
12.7
134
Correct response given to reimbursement source
yes
21.
62.3
Correct response given to eligibility requirement
yes
77.8
no
22.2
140
Expected services for which agency does not receive
reimbursement
yes
E.
Very Good
18.1
no
81.9
94
11.9
17
6.3
9
14.7
21
8.4
12
16.8
24
Needs Assessment:
22.
Transportation
23.
Psychological Help
24.
Housekeeping
25.
Shopping
26.
More frequent therapy visits
Staff
Rating
86
- 3 -
No. of
Responses
27.
Staff
Rating
As a family member, if you had the opportunity to
meet with other patient's families, to share
problems and experiences, would you come?
yes 42.3
no 48.5
undecided 8.2
NA 1.0
97
Conments and suggestions regarding this survey and its imp 1i cations for program
modification and/or future planning would be helpful to this study and greatly
appreciated.
Thank you.
87
DEMOGRAPHIC DATA:
Number of Questions in study
from Valley office
from Los Angeles office
143
102
41
Respondent to questionnaire:
Patient
Family
Patient and Family
Other
50.4%
36.0%
12.2%
1.4%
Age:
under 40 yrs.
40 - 60 yrs.
60 - 80 yrs.
over 80
2.1%
9.2%
58.5%
30.3%
Sex:
male
female
33.8%
65.5%
Lifestyle:
26.4%
37.1%
19.3%
16.4%
Living alone
Over 65 living with spouse
Living with younger generation
Deceased
Secondary Diagnosis:
Primary Diagnosis:
Heart Disease
Cancer
Urinary Incontinence
Resperatory Insufficiency
C.V.A.
Post-op. wound care
Diabetes
Ortho-Fx-neuro muscular
Other
24.5
18.2
3.5
7.7
9.8
9.1
4.9
18.9
17.5
9.8
2.8
1.4
3.5
9.8
7.0
44.1