""' CALIFORNIA STATE UNIVERSITY, NORTHRIDGE
advertisement

CALIFORNIA STATE UNIVERSITY, NORTHRIDGE
COST REDUCTIONS IN A
""'
COMMUNITY MENTAL HEALTH CENTER
A project submitted in partial fulfillment of the
requirements for the degree of Master of Science in
Health Services Administration
by
Carl Clarke McCraven
and
Eva Stewart Mapes
.January,
1976
The project of Carl Clarke McCraven
and Eva Stewart Mapes is approved:
California State University, Northridge
December, 1975
ii
DEDICATION
To Donald M. Hufhines, Dr. P. H.,
in appreciation of his knowledge
of the health professions and his
practical approach to education.
iii
TABLE OF CONTENTS
DEDICATION ...•..•..••... , • . • . • • . . . . . • . • . . • . • • . . . . . . .
iii
TABLE OF CONTENTS .•.. , . . • • • . • • • . . . . • • • . . . . . . • . . . •
iv
A BS TRACT • , , , , .• , . • . • • • . . . • • • • • • • . • . • • . • • . . . • • . . . . . .
viii
CHAPTER
1
2
IN TR ODU C TION . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
1
1.1
1.2
1.3
1.4
Problem . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Statement of Objectives .•.••••••••••••••.••.
Review of the Literature ••••••••••••••.••••.
Methodology . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
1
1
3
4
,SOURCES OF FUNDS . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
7
2. 1
2. 2
2. 3
7
7
9
2.4
2. 5
2. 6
2. 7
3
Short- Doyle/Medi-Cal. •••••.•.•.••..••.••.•
Short-Doyle . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
NIMH and NIAAA Grants •.•..•••••.••.••..•
Private Payors Including Insurance
Companies . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Medicare . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Social Rehabilitation Services...............
Summary of Revenue Sources -
11
12
12
1973/1974................. ... . . . . . . . . . . . .
12
ANALYSIS OF EXPENSES AND COST REDUCTION...
14
3. 1
Direct Expenses...........................
15
3. 1. 1
3. l. 2
15
Analysis of Staffing Expenses • • • • • • •
Actions Taken to Reduce
Staffing Expenses • • . . • . • • . • • . • • . •
Analysis of Rent, Taxes,
Utilities and Telephone. . • . • . . • • • .
Actions Taken to Reduce
Facility Costs. • • • • . • • • • . • • • . • • • •
30
Indirect Expenses . . . . . . . . . . . . . . . . . . . . . . . . .
30
3. 2. 1
30
3. 1. 3
3. 1. 4
3. 2
Ancillary Services.................
iv
16
17
TABLE OF CONTENTS (cont.)
3.2.2
3. 2. 3
3.2.4
37
3. 3. 1
3. 3. 2
Analysis of Allocation Methods. . . • • •
Potential Cost Reductions in
Indirect Expenses • . • . • • . • . . • • . . .
37
UTILIZATION AND DELIVERY OF SERVICES.......
39
4. 1
40
Analysis of the Center Intake System. . • . • . • • •
4. 1. 3
4. 1. 4
4.
4.
4.
4.
2
3
4
5
Analysis of Unmeasurable
Variables.. . . . . . . . . . . . . . . . . . . . . .
Conclusions of Analysis . . • . . • . . • . . •
Actions Taken.....................
Intake Department Changes. • • •
Inpatient Department Changes..
Outpatient Department Changes.
Indirect Services Changes • • • • •
......................
59
•••••. ••. ••
•••••••••••
61
64
. ... . . . . . . . .
.. . . .. .. ...
66
71
SUMMARY OF CHANGES MADE TO
INCREASE UTILIZATION.........................
74
LOSSES DUE TO INAPPROPRIATE
ADMISSIONS AND EXCESSIVE SERVICES... . • • • . • • .
81
4. 5. 5
Consultation
Education and
Information-Giving. . • .
Outreach and Follow-up •
Community Advisors
Organization . . . . . . . . .
Other Changes . . . . . . . . .
v
•
•
•
.
••.
. .•
•••
.••
..
..
••
••
45
46
46
52
53
55
56
4. 5. 3
4. 5. 4
••. •
••. •
••••
••••
38
•••
..•
•. •
..•
4. 5. 1
4. 5. 2
6
32
37
4. 1. 2
5
31
Allocation of Indirect Expenses
3. 3
4
Actions Taken to Reduce
Ancillary Costs..... • • • • . . . . • . • • •
Cost Reductions in
Dietary Expenses................
Building Services and
Maintenance Cost Savings. . . . . • . . •
TABLE OF CONTENTS (cont.)
6. 1
6. 2
7
Inpatient Admissions.......................
Delivery of Services in Excess
of Allocations...... . . . . . . . . . . . . . . . . . . . . .
82
RESULTS AND RECOMMENDATIONS..............
85
7. 1
7. 2
85
94
Results . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Recommendations . . • . • • • • • • • • • • . . . • • . • • . . .
7. 2. 1
7. 2. 2
8
Recommendations to Improve
Delivery of Services • • . . • • • . . • • . •
Recommendations to Achieve
Additional Cost Reductions... . . • • •
CONCLUSIONS... . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
81
94
96
98
TABLES
1
2
3
4
5
6
7
8
9
10
ll
12
13
14
15
16
17
18
19
20
21
Short-Doyle/Medi-Cal Allocation - 1973/1974
Short-DoyleAllocation- 1973/1974
Summary of Revenue Sources- 1973/1974
Results of Staff Cost Reduction- $
Results of Staff Cost Reductions- FTE's
Inpatient Staff - 1974
Partial Hospitalization Staff - 1974
Outpatient Staff - 1974
General and Administrative Staff - 19774
Center Administration Staff - 1974
Inpatient Staff- 1975
PartiaL Hospitalization Staff- 1975
Outpatient Staff - 197 5
General and Administrative Staff - 197 5
Center Administration Staff- 1975
Ancillary Cost per Patient Day Before Policy Changes
Ancillary Cost per Patient Day After Policy Changes
Ancillary Cost per Patient Day Before & After
Policy Changes
Racial Composition of Center Clients Compared
to Racial Composition of Catchment Area
Length of Treatment in Outpatient Department
Ethnic and Racial Makeup of Center Staff
vi
9
10
13
18
19
20
21
22
23
24
25
26
27
28
29
33
34
35
42
47
51
TABLE OF CONTENTS (cont.)
TABLES
22
23
24
25
26
27
28
29
30
31
32
33
Utilization of Services by Race Before and
After Changes
Inpatient Service
Partial Hospitalization Service (Day Treatment)
Individual Therapy and Counseling Service
Inpatient Service Comparison
Comparison of Costs for Services Provided
in 1973/1974 to Contract Allocations
Analysis of the Outpatient Department's
Performance for the Month of
November, 1973
Unit Costs for Services for Contract Years
1973/1974 and 1974/1975
Summary of Cost Reductions
Expense Budget for July 1, 1975/
June 30, 1976
Revenue Budget - July 1, 197 5/
June 30, 1976
Revenue Over Expense for July 1, 1975/
June 30, 1976
75
76
77
78
79
83
84
87
88
89
91
92
FIGURES
1
. Map of Center Catchment Area
44
99
BIBLIOGRAPHY
APPENDICES
100
109
127
Appendix A
Appendix B
Appendix C
vii
ABSTRACT
COST REDUCTIONS IN A
COMMUNITY MENTAL HEALTH CENTER
by
Carl Clarke McCraven
and
Eva Stewart Mapes
Master of Science m Health Services Administration
January,
1976
Over a twelve month period an NIMH funded community
mental health center reduced staffing costs, facility costs,
of ancillary services, and other indirect cost.
cost
During the same
period it modified its intake procedure, increased the Black and
-
Spanish surname staff percentages to be more representative of
the catchment area population, trained staff to be
to social needs of potential clients,
techniques,
mor~
sensitive
developed crisis intervention
eliminated long term psychotherapy care,
established
a workload of 4. 5 clients per day, introduced Problem Oriented
Medical Records,
estal?lished administrative review of excessive
AMA's and AWOL's,
assigned three or four outpatient staff mem-
hers to an office and set aside special offices for treatment,
viii
......................................-
~LL.,
1
eliminated so-called specialization for inpatient and outpatient
therapists,
and organized,
designed and initiated a comprehen-
sive Indirect Services Program,
including education, information,
consultation, follow-up and a community advisors organization.
ix
Chapter 1
INTRODUCTION
1. 1
Problem
Community mental health centers (CMHC 1 s) are faced
with the need to develop and implement plans for greater fiscal
responsibility more than ever before in their twelve years of
existence, 1
Few centers have been adequately prepared to meet
their fiscal responsibilities because of their limited years of
management experience, dependence upon Federal grants, local
and State governmental constraints,
program development.
and preoccupation with
In addition, CMHC 1 s are generally admin-
istered by managers with mental health clinical backgrounds
(i.e. ,
psychiatrist,
psychologist,
social worker,
etc. ) who have
little or no training and experience in needed administrative
skills.
Conceptually,
CMHC 1 s are expected to develop and
implement community mental health services, includ:j.ng emergency,
outpatient, partial hospitalization, inpatient, consultation and
1 u. S. General Accounting Office, . Comptroller General
of the United States, Report to the Congress, Need For More
Efficient Management of Community Mental Health Centers Program,
August 27, 1974, pp. 18-31.
1
2
education, while simultaneously developing sources of funding
adequate to compensate for declining grant revenue.
Centers are
also expected to develop cost effective methods for providing
adequate services.
A look at the fiscal situation today reveals
the following:
a)
CMHC' s staffing grants operating in nonpoverty areas for four or more years are
down to 30o/o, and in some instances, zero.
b)
Financial support for CMHC 1 s programs
from the State of California and Los Angeles
County is considered inadequate and has not
been increased at the inflation rate over the
past three years.
c)
Financial support for CMHC' s programs from
the State of California and Los A_ngeles County
is limited to direct services to patients on a
"unit of s ervice 11 basis.
d)
State of California and Los Angeles County
require that Federal grant monies be treated
as revenue and,
thereby, be used to reduce
unit cost for all services supported financially
by the State and County.
e)
Funds are not available from private sources
in sufficient amounts to compensate for declining revenue from Federal, State and
County governments.
f)
CMHC 1 s have not developed and implemented
operational plans to satisfactorily meet these
budgetary pressures.
1. 2
Statement of Objectives
This project represents a twelve month effort to analyze
the revenue,
expenses,
and utilization of the adult services of a
comprehensive community mental health center to determine
causes for inability to stay within budget;. to make recommendations for corrective measures,
and implement corrective
measures to obtain the following objectives:
1.
To establish an expense budget that does not
exceed revenue budget.
2.
To maintain unit costs within provisional rates
contracted between the Center and Los Angeles
County Department of Mental Health Services.
4
These objectives are to be achieved without reduction in
quality of care.
1. 3
Review of the Literature
The Medline service and the Cumulated Index Medicus
for 1966 to the present contain no references specific to the
objective of the project.
Subjects referenced in these sources
which are relevant to aspects of cost reduction are broad and
treated generally from the clinical approach.
Articles published
conce·rning cost reductions of mental health services related to
potential cost reductions due to changes in treatment methods
established over the past few decades rather than information on
the operation of community mental health centers.
1. 4
Methodology
A comprehensive community mental health center funded
by the Department of Health,
Institute of Mental Health and,
Education,
therefore,
and Welfare,
National
subject to its
programatic regulations was chosen as the subject of this
analysis.
I
The Community Mental Health Center commenced operations in January,
1966, with volunteers and received its first
National Institute of Mental Health (NIMH) staffing grant in
September,
1966.
The Center is comprised of two fiscally
5
independent agencies,
one which provides mental health services
for adults, and the other which provides mental health services
for children.
This analysis was limited to the Adult Mental
Health Services of the Center which is operated by a general
acute hospital.
The analysis comprised the following elements:
1.
Sources of Revenue
2.
Expenses
3.
Cost Allocation
4.
Utilization of Services
Instruments employed for the analysis included expense records,
personnel records,
payroll records,
revenue statements, utiliza-
tion statistical reports, Short-Doyle/Medi-Cal contracts,
reports, NIMH and NIAAA grant records,
cost
and expense records
for hospital cost centers that provided supportive services to the
Center.
Costs were found and assigned to appropriate cost
centers and,
in turn,
assig~ed
revenue producing centers.
or allocated to appropriate
Unit cost was determined from pro-
jected cost of the p::cogram for a twelve month period and
estimated utilization for the same period.
Each expense item was reviewed with particular
empha~
sis placed on personnel costs inasmuch as personnel accounts
for about 7 5% of the overall CMHC cost of operation.
(Personnel
-----
costs charged directly to Adult Mental Health Services represents
6
62o/o of the total mental health budget). Costs allocated from other-.
hospital departments were reviewed for their reasonableness.
Utilization of the Center's services was analyzed to
determine whether or not utilization could be increased.
A study
was made to determine if the Center was being utilized by the
population of its catchment area.
The writers of this project thesis had access to all of
the Center's records and authority to implement recommended
changes.
~-------------------------­
!
Chapter 2
SOURCES OF FUNDS
Most communities continue to rely on government
assistance for mental health services.
Assistance for mental
health services is provided through the following mechanisms:
Federal grants from National Institute of Mental Health (NIMH),
National Institute for Alcoholism and Alcohol Abuse (NIAAA),
and National Institute for Drug Abuse (NIDA),
Los Angeles
County Short-Doyle, Short-Doyle/Medi-Cal contracts for mental
illness, Short-Doyle contracts for Social Rehabilitation Services
for mentally ill criminal offenders, Medicare, and private payers.
2. 1
Short-Doyle/Medi-Cal
As a result of California legislation introduced by
Senator Alan Short and Assemblyman Donald Doyle, mental
health providers can provide mental health services to Medi-Cal
recipients through Medi-Cal intermediaries (Blue Cross and Blue
Shield) or can elect to provide services under contract with the
County.
Under Short-Doyle/Medi-Cal contracts quality and utiliza-
tion are controlled by County monitors rather than arbitrary
limitations on visits.
Billing is also simplified.
7
8
This Center elected to provide services to Medi-Cal
recipients under the Short-Doyle/Medi-Cal mechanism in 1972.
The contract specifies a maximum allocation for inpatient,
partial hospitalization and outpatient services and provisional
rates for each service.
Billing is based on units of service pro-
vided except that the billing for any month cannot exceed onetwelfth of the maximum allocation for one year, plus unused
allocations from previous months.
All applicable Federal grant
monies and funds collected from patients and their insurance
companies must be applied to monthly billings.
The provider
must apportion grant revenue according to services provided.
For example, if grant revenue was used only to pay salaries of
personnel who provided 50o/o of the units of service, then 50o/o of
the grant revenue must be applied to reduce the Short-Doyle/
Medi-Cal billing.
menc~ng
At the end of the contract period (year com-
July 1 and ending June 30) the provider must submit a
cost report which forms the basis for settlement.
If unit cost exceeds the provisional rate,
is reimbursed accordingly,
the provider
except that reimbursement cannot
exceed the maximum allocation.
If unit cost is less than the
provisional rate the provider must reimburse the County.
The Center's Short-Doyle/Medi-Cal allocations for contract year 1973/1974 are shown in Table 1.
9
Table 1
Short-Doyle/Medi-Cal Allocation
- 1973-1974
Service
Allocation
Inpatient
$ 560, 503
Partial Hospitalization
228, 187
Outpatient
161,295
$ 949,985
Short-Doyle/Medi-Cal allocations for all services amount
to $949, 985.
The Center has not been able to utilize this alloca-
tion fully because the allocation is not in the correct proportion
to the present need,
that is, the allocations for Inpatient and
Partial Hospitalization services are too low and the allocation for
Outpatient services is too high.
In the past years over 50% of
the Outpatient allocations ($90, 000) was not used.
Approval was
requested and obtained from· Los Angeles County Department of
Mental Health Services to transfer $50,000 from the Outpatient
allocation to the Partial Hospitalization allocation.
The net effect
of this action is to increase usable allocations by $50, 000.
2. 2
Short-Doyle
As a result of Short-Doyle legislation, California counties '
also can contract with mental health providers to provide mental
health services to CoUiity residents based upon their ability to
pay.
The mechanism for determining ability to pay is the
10
11
Uniform Method of Determining the Ability to Pay" (UMDAP), as
shown in Appendix A.
The provider is obliged to charge the
patient according to UMDAP and make a reasonable effort to
collect such charges.
At the end of each month the provider bills
the County for services rendered based on the provisional rate
established for each service in the contract (same as for ShortDoyle/Medi-Cal),
except that the billing in any month cannot
exceed one-twelfth the maximum allocation for the year plus
unused allocations from the previous month.
from patients,
All funds collected
other third party payers and applicable Federal
grant revenue must be applied to reduce monthly billings.
The
same rules for applying grant revenue and preparing cost reports
at year's end discussed under Short-Doyle/Medi-Cal apply.
The Center's Short-Doyle allocations for contract year
2.
1973/1974 are shown in Table
Table 2
Short-Doyle Allocation - 1973-1974
Service
Allocation
Inpatient
$
80,878
Partial Hospitalization
41, 672
Outpatient
18,531
$ 141,081
~---------------------11
2. 3
NIMH and NIAAA Grants
Federal grants made to the Center were in the form of
staffing grants.
These grants provide revenue to the Center
based upon a percentage of each staff member's salary.
In order
to include a staff member the Center must receive prior approval
for the staff position (which generally must be a professional or
non-professional clerical position) and the maximum salary.
The
percentage for which the Center is reimbursed is based upon the
length of time the grant has been in force.
Initially the grants
are at 90% of staff salaries and benefits and decline 15% each
year until a level of 30% is reached.
They remain at 30% for
the remaining life of the grant (4-years).
Grants are awarded for
a total period of eight years.
The grant revenue received by the Center during
Los Angeles County contract year 1973/1974 was $672,000.
This
amount represents funds. from six grants awarded in different
years and utilized at various levels.
That is, all positions
approved were not filled by the Center.
The funds available to
the Center from these grants will decline approximately 15% per
year over the next three to four years.
2. 4
Private Payers Including Insurance Companies
Fees paid by patients are extremely limited due to the
12
income level of residents of the area served by the Center.
The
amount received during contract year 1973/1974 was $15,211.
Insurance payments are similarly limited for the reason stated
above and also due to the fact that most health insurance plans
do not cover mental health.
Total revenue from patients and
their insurance companies amounted to $100, 000 during the year
1973/1974.
2. 5
Medicare
Total revenue from Medicare patients was $93, 000 for
contract year 1973/1974~
2. 6
Social Rehabilitation Services
Funding through Los Angeles County Social Rehabilitation
Services Program is for outpatient services for the mentally disordered offenders (MDO).
Allocation for this program was
$180,000 for contract year 1973/1974.
2.7
Summary of Revenue Sources- 1973/1974
Total revenue sources for the Center for contract year
1973/1974 are summarized in Table 3.
Table 3
Summary of Revenue Sources - 1973/1974
Partial
Hospitalization
Services
Outpatient
Services.
(Regular)
560, 503
228, 187
161,295
-
949, 985
80,878
41,672
18, 531
141,081
403,200
134,400
134,400
-
672,000
Private
47,450
-
15, 211
-
62,661
Medicare
90,000
-
3,000
-
93,000
Inpatient
Services
Short-Doyle/Medi-Cal
Short-Doyle
· NIMH/NIAAA Grants
Social Rehabilitation
Services (MDO)
Total
~~229,48~
Outpatient
Service.s
'(MDO)
Total
-
-
180,000
180,000
404,259
332,437
180,000
2,098,727
lJJ
Chapter 3
ANALYSIS OF EXPENSES AND COST REDUCTION
Expenses for the Center are classified as direct or
indirect,
based on whether they are charged directly to the
Center or are charged indirectly, using a step-down allocation
method. 2
(Note:
Center is a division of a general hospital
which provides most non-mental health services, including
x-ray,
laboratory,
personnel,
pharmacy, maintenance, dietary,
payroll,
etc.).
The general expense categories are listed below:
1.
Employees' salaries and benefits.
2.
Rent,
3.
Ancillary medical services.
4.
Miscellaneous medical services,
taxes, utilities and telephone.
medical supplies and laundry.
5.
Building services, engineering and
maintenance.
2 A method for allocating expenses to revenue producing
departments based upon their proportionate utilization of total
resources.
14
15
6.
Dietary.
7.
General hospital administration (includes
general accounting,
collection,
roll,
· 8.
9.
10.
billing,
credit and
purchasing, personnel, pay-
and insurance.
Non-medical supplies.
Operating costs.
Grant management (includes community
outreach,
consultation and education,
data processing and reporting, and
community involvement).
3. 1
Direct Expenses
3. 1. 1
Analysis of Staffing Expenses
Employee salaries and benefits amount to 60o/o
to 65o/o of total expenses.
This amount does not include
employee salaries and benefits for housekeeping, dietary,
maintenance, payroll, personnel and certain accounting,
data processing, billing and credit/collection staff which
are included under indirect expense.
An analysis of the need for staff was made
taking into account the following considerations:
a)
Clinical staff spend 60o/o of their time
~--------------------------16
in face-to-face patient contact.
b)
Demand for services as determined
by community need and availability
of funds for services.
c)
Indirect services that must be provided by comprehensive community
mental health centers. ·
d)
Emphasis on the use of paraprofessionals.
3. I. 2
Actions Taken to Reduce Staffing Expenses.
This analysis resulted in the elimination of
certain staff positions and the substitution of paraprofessionals for unnecessary professional staff.
Most
of these staff reductions were made by attrition.
The results of the staff changes are summarized in Tables 4 and 5.
The cost reduction resulting
from staff changes represents an annual savings of
$213, 302 (see Table 4).
The net chal}ges in full time
equivalents (FTE 1 s) were a 3. 5 decrease in clinical staff
and a 0. 9 decrease in non-clinical staff (see Table 5).
17
The staff positions,
number of FTE' s and annual salaries ..
in 1974 and 1975 are presented in Tables 6 through 10
and Tables 11 through 15,
3. 1. 3
respectively.
Analysis of Rent,
Telephone.
Taxes, Utilities and
An analysis of the Center 1 s operations revealed that cost reductions amounting to $30, 000 could
be achieved by consolidating offices located elsewhere
into the main facility.
,.
r
1
~·
'
i
Table 4
Results of Staff Cost Reduction- $
Employee Salaries and Benefits
Service
1974 Actual.
Inpatient
$
474, 135
Annual Salary
Increased lOo/o
to adjust
for inflation
$
522, 648
1975 Annual
Salary
$
467,089
Cost Reduction
$
55, 559
Partial
Ho spi tali zation
210,749
231,824
188, 358
43,466
Outpatient
231,882
255,070
151,620
103,450
General and
Administrative
233,035
256,339
24 5, 512
10,827
$1,265,881
$1,052,579
$ 213,302
.
$1,147,985
......
00
19
Table 5
Results of Staff Cost Reduction - FTE's
(Full Time Equivalents - FTE' s)
Change
Clinical Staff
Psychiatrists
General Practitioner
Physician Assistant
Social Workers
Psychologists
4.5
0.8
Nurse Therapists
RN' s (other)
LVN's/LPT's
Nurse's Aides
Ward Clerks
Activity Workers
Counselors
2.0
1.0
5. 8
5. 0
0
3.0
0. 8
1.0
8. 6
6.4
8.2
5. 1
1. 5
No
1. 0
2.2
3. 1
decrease
change
increase
decrease
decrease
2. 0
10.0
7.0
1. 0 decrease
2.8 decrease
1. 5 decrease
5. 8 increase
No change
0. 5 increase
1. 3 increase
NET CHANGE
3.5 decrease
8.6
6. 5
5. 0
2.0
9. 5
5. 7
10.8
Non-Clinical Staff
Administrators
Accountants/Billing Clerks
Intake Workers
Medical Records Clerks
Secretaries
Telephone Operators
Financial Counselor
. Director of Volunteers
Director of Alcoholism
Program
Center's Share for
Center Administration
Health Educator
Office Manage·r
Receptionist
Van Drivers
1.3
5. 0
2.0
3. 0
1.5
2.0
1.0
1.0
o.
3
5. 2
3. 0
3. 0
1.3
1.5
1.0
1.0
1. 0 decrease
0. 2 increase
1. 0 increase
No change
0.2 decrease
. 0. 5 decrease
No change
No change
1.0
1.0
No change
2. 9
2.0
1.0
1.0
1.0
3. 0
0.9
1. 0
1. 0
1. 0
1. 0
0
0
0
2.0
NET CHANGE
decrease
increase
increase
increase
increase
0.9 decrease
20
Table 6
Inpatient Staff - 1974
1
FTE s
.
,
Annual Salary
(including fringe benefits)
Psychiatrists
3.0
$ 135,610
General Practitioner
0.8
29,420
Social Workers
3. 7
57, 193
Psychologists (MA)
1.0
14,627
Counselors
1.3
9,218
RN 1 s
8.6
110, 868
LVN 1 s/LPT 1 s
6. 5
55,959
Nurse 1 s Aides
5. 0
37,420
Ward Clerks
2. 0
14,370
Activity Workers
1.5
10,450
33. 5
$ 475, 135
11!.,
21
Table 7
Partial Hospitalization Staff - 1974
FTE s
1
-,.
Annual Salary
(including fringe benefits)
$
38,465
Psychiatrists
0.9
Psychologists
2.2
44,902
Social Workers
1.5
21,225
Nurse Therapist
1.0
12,609
Counselor
o. 6
5,014
Activity Workers
8.0
74,031
Van Drivers
2.0
14, 503
16. 2
$ 210,749
22
Table 8
Outpatient Staff -
FTE's
1974
Annual Salary
(including fringe benefits)
Psychiatrists
o. 6
Psychologists
4.9
86,717
Nurse Therapist
1.0
16,454
Social Workers
3.4
59, 363
Counselors
3. 8
43,246
13.7
$ 231,882
$
26, 102
23
Table 9
General and Administrative Staff - 1974
FTE's
Annual Salary
(including fringe benefits)
$
27,697
Administrators
1.3
Accountants/Billing Clerks
5. 0
45, 393
Intake Workers
2. 0
16,073
Medical Records Clerks
3. 0
21,637
Secretaries
l. 5
12,097
Telephone Operators
2. 0
15,342
Financial Counselor
l. 0
7,681
Director of Volunteers
l. 0
13,259
Director, Alcoholism
Program
1.0
22, 111
Data Analyst
1.0
11, 577
Adult Center's Share of
Center Administration
(See Table 10)
2.0
40, 168
21.7
$ 233,035
24
Table 10
Center Administration Staff - 1974
FTE's
Annual Salary
(including fringe benefits)
Administrators
2.0
Accountant
o.
3
7,957
Programmer
o.
5
5, 137
Statistical Clerk
1.0
7,286
Secretaries
2. 0
17, 571
5. 8
$ 80,336
Note:
$ 42,385
Adult Center's Share is $40,168 (2. 9 FTE's)
25
Table 11
Inpatient Staff - 1975
FTE's
Annual Salary
(including fringe benefits)
$
82,822
Psychiatrists
1.9
Family Practitioner
0.8
28,730
Social Workers
2. 5
43,912
Psychologists (MA)
1.5
2 5, 033
Counselors
2. 9
28,969
Activity Workers
2. 3
17,426
RN's
5. 8
81,907
LVN' s/LPT' s
5. 0
49,416
10. 8
78,483
Ward Clerks
2. 0
17,861
Physician Assistant
1.0
12, 530
36. 5
$ 467,089
Nurse's Aides
26
Table 12
Partial Hospitalization Staff - 1975
FTE's
Annual Salary
(including fringe benefits)
Psychiatrists
o. 6
Psychologists (Ph. D.)
1.0
23,418
Psychologists (MA)
0.4
6,644
Social Workers
o. 8
12,420
Nurse Therapist
1.0
16, 527
Counselors
o. 7
7,063
Activity Workers
7. 7
79,993
Van Drivers
3. 0
20,228
15. 2
$ 188,358
$
22,065
27
Table 13
Outpatient Staff -
FTE 1 s
1975
Annual Salary
(includes fringe benefits)
Psychiatrist
0. 5
Psychologists
2. 2
39,079
Social Workers
3. 1
49,066
Counselors
3.4
45,088
9. 2
$ 151,620
$
18, 387
28
Table 14
General and Administrative Staff - 197 5
FTE's
Annual Salary
(including fringe benefits)
$
10,028
Administrator
0. 3
Accountants/ Billing
Clerks
5. 2
54, 189
Intake Workers
3. 0
25,226
Medical Records Clerks
3. 0
25, 594
Secretaries
1.3
13,245
Telephone Operators
1.5
11,839
Financial Counselor
1.0
7, 956
Director of Volunteers
1.0
13,922
Director of Alcoholism
Program
1.0
15,479
Data Analyst
1.0
8,665
Office Manager
1.0
9,778
Health Educator
1.0
13,923
Receptionist
1.0
6,263
Adult Center's Share of
Center Administration
(see Table 15)
2. 0
29,405
23.3
$ 245, 512
29
Table 15
Center Administration Staff - 1975
(Shared equally by both Agencies)
FTE's
Annual Salary
(includes fringe benefits)
Administrators
1.7
$ 38,620
Programmer
0. 5
5, 394
Statistical Clerk
1.0
7,492
Secretaries
o. 7
7,304
3. 9
$ 58, 810
Note:
Adult Center's Share is $29,405 (2. 0 FTE's)
30
3. 1. 4
Actions Taken to Reduce Facility Costs
The administrative, accounting and billing
offices previously located in the Medical Building of the
Hospital were moved to the main facility which resulted
in an annual cost savings of $17, 000.
This amount does
not reflect savings in personnel cost as a result of the
reduction in travel time between buildings.
The Social Rehabilitation Services Program
was moved to the main facility.
This action resulted in
an annual cost savings of $13, 000.
3. 2
Indirect Expenses
3. 2. 1
Ancillary Services
Cost of ancillary services, including radiology,
laboratory and pharmacy, were analyzed from the standpoint of treatment category and length of stay.
analysis for a 3l.:day period .in July,
The
1974 revealed that
the cost per episode for mentally ill, alcohol abuse, and
drug abuse patients was $265.54, $173.00, a~d $189.44
respectively.
alcohol abuse,
The cost per patient day for mentally ill,
and drug abuse patients was $22. 36,
$36. 04 and $30. 44 respectively.
(See Table 16).
Discussions with the medical staff revealed
31
that the cost for ancillary services was due,
extent,
to tests,
procedures,
to some
and medication related to
physical rather than psychiatric problems.
3.2.2
Actions Taken to Reduce Ancillary Costs
Medical staff were requested to limit ancil-
lary services for physical problems to emergency
conditions to reduce the expenditure of mental health
funds for non-mental health conditions.
Social workers
were urged to work closely with medical staff to make
sure that conditions observed during a patient 1 s physical
examination and/ or hospitalization were followed up by a
family or general practitioner after discharge.
An analysis for the 31-day period in July,
197 5 revealed that the cost per episode for mentally ill,
alcohol abuse,
$187.43,
and drug abuse patients was $189.49,
and $154. 03 respectively.
day for mentally ill,
alcohol abuse,
The cost per patient
and drug abuse
. patients was $18. 87, $26. 27 and $26. 63 respectively.
(See Table 17).
The reduction in the utilization of ancillary
services per patient day for mentally ill, alcohol abuse,
and drug abuse patients amounts to 16o/o,
13o/o, and 27o/o
32
respectively.
(See Table 18).
Based on our current division of services
which is SO% mentally ill,
drug abuse,
25% alcohol abuse,
and 25%
the cost reduction due to the reduction in
ancillary services, amounts to $23, 000 per year.
An additional cost reduction is anticipated as
a result of a policy change requiring a single view chest
x-ray as a condition for admission rather than a two
view chest x-ray which currently is required.
This
change will result in a cost reduction of $6, 000 per year.
3.2.3.
Cost Reductions in Dietary Expenses
A study of dietary practices revealed that
center staff members were served meals along with
patients although staff did not pay for their meals as
required of other hospital employees.
changed.
This practice was
Two members of the nursing staff were re-
quired to take meals with patients at each meal.
Meal
tickets were issued to these staff members at no cost to
them.
All other staff personnel were required to pur-
chase meal tickets or eat elsewhere.
This change
resulted in an estimated cost reduction of $10,000.
Table 16
Ancillary Cost Per Patient Day Before Policy Changes (July,
1974)
Diagnosis
Mentally
Ill
Drug
Detox.
24
285
11. 9
Number of Admissions
Number of Patient Days
Average Length of Stay
Alcohol
Detox.
All
Combined
5
24
4.80
18
112
6.22
47
421
8.96
Cost per Admission:
Pharmacy
Laboratory
Radiology
Other
Total
$ 148.29
47.88
29. 79
39. 58
$
$ 265. 54
69.61
68.83
24:83
26. 17
84.20
25.20
43.20
20.40
$
111. 34
53,49
29.32
32.40
$ 189.44
$ 173.00
$
126,55
$
Cost per Patient Day:
Pharmacy
Laboratory
·Radiology
Other
Total
$
12.49
4.03
2. 51
3. 33
$
11. 19
11. 06
3. 99
4.20
$
17. 54
5, 25
9.00
4.25
$
12.43
5. 97
3.27
3, 62
$
22.36
$
30.44
$
36.04
$
2 5. 29
(.N
(.N
I
~
/
Table 17
Ancillary Cost Per Patient Day After Policy Change - (July, 1975)
(Adjusted to July, 1974 charges which were 1 O% lower than July, 197 5)
Diagnosis
Mentally
Ill
Number of Admissions
Number of Patient Days
Average Length Stay
Drug
Detox.
25
251
Alcohol
Detox.
42
243
5.78
1 o. 0
All
Combined
15
107
7. 13
82
601
7.33
Cost per Admission:
Pharmacy
Laboratory
Radiology
Other
$ 111. 97
Total
$
53.92
11. 82
11. 78
62. 16
66.05
20.67
5. 15
$ 189.49
$ 154. 03
$ 187.43
$ 170.95
$
$
10.74
11.42
3. 57
. 89
$
13. 82
8. 08
1. 49
2.88
$
11.46
8.30
2.20
1. 36
$
26.63
$
26.27
$
23. 33
$
98.60
57.63
10.61
20. 59
$
84.01
60.81
16. 13
10.00
Cost per Patient Day:
Pharmacy
Laboratory
Radiology
Other
11. 15
5. 37
1. 17
.
Total
1. 17
$
18.87
w
~
i
~
Table 18
Ancillary Cost Per Patient Day Before and After Policy Change
Before (July, 1974)
Mentally Ill
Average Length
of Stay
Patient-Days
11. 9
Cost
_$_
Before (July, 197 5)
Average Length
of Stay
Patient-Days
10.0
Cost
_$_
Adjusted to
July, 1974
Charges 1
Pharmacy
Laboratory
Radiology
Other
12.49
4.03
2. 51
3. 33
12.27
5. 91
1. 29
1. 29
11. 15
s. 37
1. 17
1. 17
Total
22. 36
20.76
18. 87
Drug Detox.
6,22
11. 19
11. 06
3. 99
4.20
11.
12.
3.
.
82
56
93
98
10.74
11.42
3. 57
. 89
Total
30.44
29.29
26.63
(continued next page)
'
16%
5. 78
Pharmacy
Laboratory
Radiology
Other
.
Percent
Decrease
13%
w
U1
Table 18 (continued)
Before (July, 1974)
Alcohol Detox.
Average Length
of Stay
Patient-Days
4.80
Cost
_ $_
Before (July, 197 5)
Average Length
of Stay
Patient-Days
7. 13
Cost
_$_
Adjusted to
July, 1971
Charges
Pharmacy
Laboratory
Radiology
Other
17. 54
5. 25
9. 00
4.25
15. 20
8.89
1. 64
3. 17
13.82
8.08
1. 49
2.88
Total
36.04
28.90
26.27
All Combined
Percent
Decrease
27o/o
7.33
8.96
Pharmacy
Laboratory
Radiology
Other
12.43
5. 97
3. 27
3.62
12.61
9. 13
2.42
1. 50
11.46
8.30
2.20
1. 36
Total
25.29
25. 66
23. 33
1 Charges in July, 1974 were 10% lower than in July,
1975.
(J.l
0"
37
3.2.4
Building SerVices and Maintenance
Cost Savings
Moving the Social Rehabilitation Services
(MDO) Program to the main facility resulted in an annual
cost reduction of $6, 000, inasmuch as the total cost of
these services could be spread over that program as well
as Inpatient, Partial Hospitalization,
and Outpatient ser-
vices.
3. 3
Allocation of Indirect Expenses
3. 3. 1
Analysis of Allocation Methods
Allocation of indirect expenses between mental
health services and other hospital departments were made
based upon Medicare and Medi-Cal cost reports utilizing
step-down methods.
While this approach is in keeping
with acceptable accounting practices it is not equitable to
the Center because (a) mental health services currently
represent a high percentage· of total inpatient services
(28o/o),
causing cost allocations which were based on
occupancy to be unfairly high,
(b) mental health services
are provided in a separate building that results in major
direct costs to the Center,
(c) the hospital requires high
operating engineering costs on a 24-hour basis which are
not necessary for the Center,
and (d) certain services
38
were billed to the Center which are being provided by
staff whose time is charged to the Center (i.e., nursing,
administration, medical records,
and portions of billing
and general administration.).
3. 3. 2
Potential Cost Reductions in
Indirect Expenses
It is not possible to accurately estimate,
this time,
the cost reduction that will result,
believed to be in the. area of $2 50, 000.
but it is
Savings in
nursing administration, medical records and general
administration will amount to $150, 000.
at
Chapter 4
UTILIZATION AND DELIVERY OF SERVICES
Increased utilization is desirable not only for the obvious
reason that more people are served but because fixed cost is
spread over a larger number of units of service.
Utilization is dependent upon demands for services which
are related to a variety of factors including:
Community need.
Community awareness of mental
health services.
Center's acceptance by the community.
Center's relationship with referral agencies.
Center's outreach program.
Center's community involvement.
Accessibility of services.
Response of staff to clients on first
contact.
A program was developed and implemented to address
these factors and increase utilization.
This program included
ways to increase the ability of the Center to deliver services.
39
40
The program and the analysis upon which it was based are described in the following paragraphs.
4. 1
Analysis of the Center Intake System
The Intake Department includes the following areas:
Reception
PBX
Financial Counseling
Intake Office
Clerical
Clerical
Clerical
Clerical/Clinical
All clients who use the services of the Center are
processed through the Intake Department before treatment begins.
By observation at the beginning of the analysis, it appeared that
clients were being screened out, utilization was low, and few
minority clients were visible.
Follow-up telephone calls were made to approximately
thirty potential clients who contacted the Center in ·1974 by telephone or on a walk-in basis.
These individuals had been on a
waiting list for a minimum of one· month to a maximum of three
months.
None of the individuals made a second contact or were
interested in receiving services when the follow-up calls were
made.
A demographic analysis,
as shown in Table 19, of the
population currently receiving treatment at the Center provided
the following profile of clients:
1.
Most clients (79o/o) were white.
41
2.
The percentages of Spanish surname and black
clients did not reflect the percentages of those
groups in the population served by the Center.
3.
Only 57o/o of the clients served lived within the
catchment area.
Ideally,
almost all clients
should reside in the catchment area.
4.
Most referrals (64o/o) were made by
11
sel£11 •
No
significant number of referrals came from other
types of agencies except 7% from hospitals and
physicians.
This figure should have been much
higher because the Center is part of a general
hospital.
Records of another agency similar to
the Center indicated that 37o/o of referrals were
made by
11
sel£11 and significant percentages of
referrals came from appropriate categories of
other agencies such as schools, Department of
Social Services, and legal agencies related to
law enforcement and the Courts.
5.
Monthly income below $500 was reported by
4 5% of the clients.
Thirty-one percent of
clients reported no income from employment.
42
Table 19
Racial Composition of Center Clients Compared
to Racial Composition of Catchment Area
Percent of Center
Clients - June, 1974
Percent of
Catchment Area
Population
White
79%
58%
Spanish Surname
11%
22%
Black
9%
18%
Other
1%
2o/o
Racial Group
Community mental health centers are expected by NIMH
to serve all segments of the population equally.
utilization of services relative to race,
age,
Disproportionate
sex and economic
status indicates that potential patients are not being served.
A demographic study of social stress indices and
physical health indices was made by the staff Health E_ducator,
using Health Department and U.S.
Census Bureau information.
The two kinds of indices were combined on the assumption that
mental illness .is related to physical health problems and social
stress.
The statistics from this study were collected and presented according to census tracts in the Center's catchment
43
area.
3
As a result, it is now possible to determine whether
the census tracts having residents at greatest risk to mental
illness are being served by the Center.
The ranking of census
tracts in descending order of stress and the admissions for
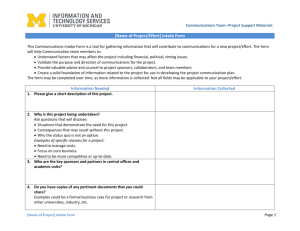
treatment from each census tract are shown in Figure 1.
Referring to Figure 1, for example, the number to the
left of the slash mark indicates the ranking of census tracts
with residents at greatest risk (stress) in descending order
(i.e. ,
census tract number 10 is at lowest risk and census
tract number 21 is at highest risk).
The number to the right
of the slash mark indicates the percent of patients admitted for
treatment in October,
197 5 by the Center who reside in the
indicated census tract (no patients were admitted from census
tract number 10 which has a stress rank number ,of 33 and 2%
of the patients were admitted from census tract number 21 which
has a stress rank number of 1).
The Center is giving high
priority to outreach for the eleven census tracts at greatest
risk which are numbers 21,
20,
14,
12, 24,
13,
23,
16,
32 and 30.
3 See Paragraph 4. 5, Indirect Services Changes.
18,
I'
f
~census
Tract
Number
Ranking
Percent of
Patients
Admitted
34'!'
.\
?.4/0. 5
·:'census tr·act numbers are coclcd.
') /0
12/i
'•.
50. S P";·ce11t of the pati<."n\9 arlmitte<i. for t.·entn•"nt d•~ring October, 1975 were from
the Catchment A .•·ea design;.t.,d by Natinnal Jn~l\tute of Mental Health and 49.5 p<:r('c·nt ·,vc re fron1 outside the Catchn1f'nt .,\rca.
1 'J,i<.: n 1~ 1
,.
t\1ap of Centt:r C:.tf.'·lntwnt (sr:rvi,-:l') Area showing desct!nding r?nk of
stress fnc;tor and jH:~1·ccnt of pc.lticnts admitted during October, 1975.
~
~
45
4. 1. 2
Analysis of Unmeasurable Variables
Several significant variables affect utilization
which can be measured.
even documented.
Others cannot be measured or
For example, negative attitudes of
Intake staff toward racial minorities, alcoholics, and
drug abusers,
the chronically ill,
or the poor, some-
times are manifested in subtle ways during intake procedures.
In many cases,
potential clients in these cate-
gories have special needs for expert financial counseling
and encouragement to utilize professional services which
Intake staff may not be qualified or trained to fulfill.
In such instances,
these -clients fail to return for ser-
vices.
Professional staff may have treatment
preferences for certain types of mental health problems,
and varying degrees of .willingness to meet needs of all
potential clients.
Work patterns o~ all staff, including professional and para-professional,
appeared to be geared to
low utilization •. Informal systems had developed which
were very difficult to understand, but which seemed to
link the professional staff and the intake staff together
in decisions on whom to treat and when to treat them.
4h
4. l. 3
Conclusions of Analysis
Subjective observation and objective analysis
indicated a major change of the entire Intake Department
was needed.
The following objective was isolated from
the information collected:
To increase the responsiveness of the mental
health center to the mental health care needs
specific to its catchment area,
to be
measured by a 32o/o increase in a period of
eight months in clients who live in eleven
high mental illness risk census tracts.
This objective was programmed into the
Intake Department using Management by Objective Principles.
(See Appendix B).
Final assessment of these
proposed changes in the Intake Department will be made
in June,
4. 1. 4
1976.
Actions Taken
The general mode of the Center's treatment
of mental health problems was examined by reviewing the
average length of time spent in treatment in a sampling
of cases.
An unbiased sample of ninety-two active out-
patient cases was obtained by selecting each case at the
47
beginning, middle,
and the end of each page of a listing
of active cases.
The results from an analysis of this sample are
shown in Table 20.
Table 20
Length of Treatment
In Outpatient Department
Percent of Cases
%
22
6
Length of Treatment
Months
0 - 3
3 - 6
14
6 - 12
29
12 - 18
19
18 - 24
10
Over 24
Referring to Table 20, it is seen that 58% of the
cases sampled were over twelve months in duration and
lOo/o_over twenty-four months.
In an effort to extend the resources of the Center
to a larger number of people and to increase the number
of units of service delivered,
the general mode of treat-
ment was changed from a long term psycho-therapeutic
48
approach to one of crisis intervention which focuses on
the presenting situational problem.
Long term care was
discouraged.
The crisis intervention approach to mental health
problems dictates immediate response to the first contact made by the client and focuses on the set of circumstances which provoked the client to seek care.
Long-term psycho-analysis was discouraged in favor of
immediate, intensive treatment to enable the client to
solve immediate situational problems and formulate
short term goals.
4
The crisis intervention approach dictates the average number of visits per episode.
after an episode of 6-8 visits,
determine
t~e
Each case is reviewed
except for follow-up to
status of the client after an agreed upon
.
5
length of time.
If further care is indicated a new treatment plan is
4
"Program Models for Emergency Mental Health Services, 11 Course No. IX-21, offered by the Center for Training
in Community Psychiatry, 1974, Howard J. Parad, D. S. W.,
Coordinator.
5
Martin Strickler and Jean Allgeyer, 11 The Crisis Groups:
A New Application of Crisis Theory, 11 . Social Work, Vol.. 12, #3
(July, 1967}, 28-32.
49
made in consultation with other staff.
New treatment
plans are designed which may include referral to
another agency for specialized services.
In any case,
continuation of treatment beyond the crisis episode
must be oriented to specific problems and goals, with
regular review and consultation.
The traditional medical record keeping system is
being changed to a psychiatric adaptation of the Problem
Oriente.d Medical Records sy_stem.
In addition to pro-
viding better medical records, it is expected that use of
this system will assist therapists in focusing all treatment plans precisely on the problem presented.
6
Problem Oriented Medical Records procedures do
not permit entries in the chart which are unrelated to a
stated problem.
Several inservice training sessions were conducted
for the staff on the socio-economic, health, and mental
health needs of the catchment area population to develop
6 Lucy D. Ozarin, ''PSRO' s and Mental Hospitals; a Report,"
Administration in Mental Health, Department of Health, Education,
and Welfare, Alcohol, Drug Abuse, and Mental Health Administration, Public Health Service Publication No. (ADM) 7 5-192, Spring,
1975, pp. 19-22.
50
awareness of the necessity for increasing the Center's
ability to deliver services to more people.
Units of service delivered by each therapist was
monitored.
A goal of 4. 5 individual units of service per
day per therapist was established as an acceptable work
load.
Working hours of therapists were managed to pro-
vide evening hours for working clients.
Therapists· were required to work full eight-hour
days,
excluding lunch,
rather than the seven and one-half
hours which had become the norm.
"Compensatory time",
a method by which therapists
were doing paper work or seeing patients after hours to
accumulate large blocks of time off,
was abolished.
Instead,
to be taken at will,
therapists were assigned to work
evenings to see patients needing evening hours.
This
policy change made it possible for administrative s1:aff to
do accurate planning and staffing.
To increase group therapy skills of all clinical
staff, inservice training in group therapy was provided.
Group therapy is encouraged to extend the Center's
resources to a larger number of clients.
At the
beginning of this study 7 5o/o of all therapy was provided
on an individual basis and 25o/o was done in groups.
At
...-----------------------51
the present time the percentage of group units of service
has increased to 3 5o/o.
Continuous emphasis is being
placed on group therapy until a goal of 50% is reached.
I
I·..
l
:{r
.·~
The ethnic makeup of the staff was not representative of the area served.
The staff was 82% white,
9% black and 9% Spanish surnamed. In addition, none
of the clinical staff were black or Spanish surnamed
. (.:
:;/
'
except for three black licensed psychiatric technicians
(LPT' s) on the nursing staff.
.
I
Through affirmative action and by incorporating
Social Rehabilitation Services into the main facility,
the
ethnic makeup of the Center staff is more representative
of the area served.
Currently the ethnic makeup is as shown in
Table 21.
Table 21
Ethnic and Racial Makeup of Center Staff,
October, 1975
White
Spanish
Surname
Black
Total
65%
14%
21%
Clinical
69%
12%
19%
Non- Clinical
59%
15%
26%
52
4. 2
Intake Department Changes
A registered nurse was hired to supervise the Intake
Department.
This was done to assist Administration in sepa-
rating clinical judgment from other considerations in the
decision to admit or refuse to admit a client.
Two clinical staff members were assigned daily to the
Intake Office to do initial evaluations on new applicants for
service.
This was done to eliminate the waiting list on which
potential clients had been
plac~d
for as long as three months.
The Intake Office was moved out of the Inpatient area
to prevent screening out of clients and to curtail unofficial
consultations on admissions between Intake and Inpatient staff.
A new policy was developed to separate the clinical decisions
made by the Medical Director from other considerations for
admission.
The personnel responsible for non-clinical decisions
were specified, as were any non- clinical conditions under which
patients may be refused,
Any counseling done at the time of intake was restricted
to the two clinical staff members assigned to intake duty for
the day.
Other intake staff were instructed to process the
client in a friendly,
efficient manner,
and to ask only the
questions necessary to provide the documentation required for
forms used by clinical staff.
Certain intake personnel were
53
transferred to other areas because they preferred to do
counseling as para-professionals rather than be restricted to
the new intake procedures.
The record keeping system in the Intake Office was
examined.
A file which contained unofficial information about
patient's previous hospitalizations was removed on the assumption that it was used as a screening device.
Meetings were held between various referring agencies
and administration and staff members of the Center to remove
any barriers that interfered with referrals of patients to the
Center.
4. 3
Inpatient Department Changes
It was determined that some inpatients were being re-
fused on the basis of sex as related to physical arrangement of
rooms.
Inpatient rooms have two beds each with adjoining baths
which permits mixing of patients.
This is a problem with drug
and mentally ill patients who are physically well and active.
To
avoid mixing sexes several patients must be shifted to different
beds to admit new patients when the department is close to
capacity.
Resistance from nursing staff is natural.
Staff was
instructed to use time freely to shift patients to accommodate
new patients so that all beds are utilized according to demand.
54
A regular daily discharge time was determined to assist
staff in planning for utilization of empty beds.
The previous
system had allowed patients to be discharged at their convenience at any time during the day,
often resulting in denial
of a bed to a new patient.
Disciplinary discharges, incidences of patients departing
against medical advice (AMA),
or being absent without leave
(AWOL) were investigated by spot-checks of incidents.
Nursing
staff have recently been required to write an incident report
to Administration for every such incident that occurs to make
it possible to determine if the departure of the patient is
related to negative attitudes of any staff member or whether
staff members make a reasonable effort to prevent the early
departure of the patient.
Planned discharge of each patient, while required by
existing policy and procedures, was emphasized.
Each inpatient
during the course of a stay is a recipient of a treatment plan
which includes the participation of an individual therapist, a
group therapist, members of the nursing staff, the psychiatrist,
and activity therapists.
A treatment plan is developed with the'
participation of these staff members.
integral part of the above.
Discharge planning is an
It was determined by supervisory
staff that treatment planning activities needed strengthening and
55
coordinating to make certain that each inpatient receives complete and continuous care and follow-up after discharge.
A chief social worker was assigned to the Inpatient
Department to assume responsibility for treatment planning and
continuity of care for each inpatient.
This person also was
given responsibility for referral of the inpatients to outpatient
care following hospitalization.
4. 4
Outpatient Department Changes
Staff who had been assigned to separate services (men-
tally ill, alcohol and drug) were relieved from those assignments and asked to respond to requests for services in all
categories.
This was done to provide staff promptly where
demand is greatest and to prevent wasted staff time in departments at times when demand ·is low.
Specialization was dis-
couraged to provtde flexibility of staff.
All therapists had individual offices in which they treated
patients and executed necessary paper work and did charting
behind closed doors.
To keep therapists circulating and to
increase space available for patient treatment, therapists were
assigned three to an office.
The remaining offices were desig-.
nated as therapy rooms and assigned as needed by the receptionist.
This change assisted in the prevention of specialization
by therapists,
since assignment of therapists to patients is
56
increasingly made on an
11
as needed11 basis, to all departments.
Isolation of therapists was reduced and greater interchange
between staff resulted.
The change may have a relationship to
the increase in productivity.
(See Table 25).
Therapists were
instructed to indicate on the master appointment book which
hours are filled,
rather than which hours are open.
This
makes it simpler to determine if the therapist has a client at
any particular hour.
If the therapist has no client it is assumed
that the therapist is free to see any patient in any department
which needs therapy.
This system assists in preventing lost
therapy time and in maintaining the flow of therapists through
all departments according to demand.
4. 5
Indirect Services Changes
All indirect services (activities related to patient care
other than therapy or counseling) were organized into a formal
program.
The Indirect Community Services Program was
designed to extend services of the Center beyond treatment of
illness in the Center to early crisis intervention and prevention
of chronic illness in the community.
The components of the Indirect Community Services
Program are:
57
Consultation
Education and Information
Outreach and Follow-up
Community Advisors' Organization
The program was based on the assessment of the community's mental health needs which combined socio-economic
problems with physical health problems on the assumption that
both contribute to mental health care needs.
Indices used were:
deaths,
syphilis,
Live births, infant deaths, fetal
gonorrhea,
TB,
hepatitis,
childhood diseases,
percent of families with income less than . 50 of the poverty
level,
percent of persons over twenty-five with no schooling,
percent of unemployed males over sixteen,
and percent of
housing units lacking plumbing.
Center staff studied the census tracts from its catchment
area and compared them with the entire health region (60 census
tracts) and found that the top eleven socio-economic stress
areas (high unemployment,
educational level,
those eleven,
poor transportation, below average
etc. ) are in the Center's catchment area.
Of
six are in close proximity to the Center.
In addition,
the study revealed the following health con-
ditions existing in the Center's catchment area:
58
The highest number of live births occurred in
two census tracts.
Two tracts rank first and fourth in infant deaths.
Two tracts rank first and fifth in fetal deaths.
Two tracts have the two highest gonorrhea rates.
Five tracts have the top five rates of syphilis.
Four tracts rank
•
1, 2, 3, and 5 in TB deaths.
The top three rates of hepatitis are in the
catchment area.
The health indices and socio-economic data were combined to develop the stress scale shown in Figure 1.
The Consultation, Education and Information Programs
were designed from recom:rhendations and requirements of the
United States Department of Health, Education,
and Welfare
Public Health Service and the National Institute of Mental Health.
Center staff, including department heads,
the health educator,
and .a psychiatrist assisted in the development of the final form
of the program.
The program has been approved and is being
used as a guideline by the health educator and other staff
responsible for Consultation and Education.
Community men tal health is the responsibility of the
'
59
Center and the purpose for which Centers were funded.
The
Consultation and Education and Information Programs provide
means to join together all of the agencies and organizations in
the community having resources to provide for the needs of its
members. 7
Such a network provides an alternative to long
term hospitalization outside of the community and can reduce
the incidence and severity of mental illness.
The long term
goal of Consultation and Education is to help a community to
improve the health of its members, prevent mental illness, and
promote mental health.
4. 5. 1
8
Consultation
When consultation is provided for a profes-
sional in regard to an individual patient for the purpose
of diagnosis,
treatment and/ or disposition, the consulta-
tion is case oriented.
7 Consulta.tion is defined as a voluntary relationship
between professionals for the purpose of exchanging information or collaborating to solve an existing or potential problem.
Consultation encompasses education as needed to help an
individual or an organization to increase skills and knowledge
to assist a patient or potential patients.
8
National Institute of Mental Health, Consultation and
Education, A Service of the Community Mental Health Center,
U.S. Department of Health, Education, and Welfare Public
Health Service, Public Health Service Publication No. 1478,
1966.
60
Consultation directed toward improvement of
program related to community mental health is called
program oriented consultation.
Consultation may be directed toward program
administration,
planning and development of programs
to be used by the agency in the community,
rather than
toward the agency program itself.
Consultation directed toward development of the
skills of the professional receiving the consultation,
even though a case of the professional is under discussion, is called Staff Development and/or Continued
Education because the main objective is not directed
toward disposition of the case.
Consultation for Center staff is not included in
consultations under Indirect Services.
Recipients of consultation are categorized by NIMH
as follows:
1.
State and local law enforcement and
correctional agencies.
2.
Facilities and organizations concerned
with
3.
alcoholism~
Facilities and organizations concerned
with drug abuse.
61
4.
Facilities and organizations concerned
with family planning.
5.
Mental health facilities not affiliated
with the Center.
6.
Health services delivery system.
7.
Public welfare agencies.
8.
Facilities and agencies for the aged.
9.
Facilities and organizations concerned
with children (other than schools).
10.
Schools.
a)
b)
c)
11.
Public primary
Public secondard
All other (including Head Start,
universities, private, parochial
and professional schools).
VA facility or other organization concerned with Veteran care, e. g., Twice
Born Men,
etc.
12.
General public.
13.
Other.
4. 5. 2
Education and Information-Giving
Education is a knowledge building activity.
The following definition has been agreed upon by department heads,
staff:
the health educator, and other professional
62
Education services are planned and coordinated
activities integrating facts,
concepts, values,
and skills which promote responsible
decision
making regarding the use of mental health
services.
A distinction has been made between education and
information giving.
Indirect community services in-
cludes information giving as a subdivision of education.
Information giving is treated separately because, by
itself, it does not accomplish the purpose of education
as defined above.
Education is to be performed by clinical staff in
some of the following settings:
Lectures
Seminars
Programs sponsored by the Center with
the assistance of the Advisors.
Other
activities include teaching classes in
junior high and high schools based on a
pilot education program conducted for
students and teachers by our Alcoholism
Health Educator at a local high school in
1974-75,
63
Training provided for school nurses,
counselors,
and PTA leaders in
alcoholism and drug abuse education
and in recognition of the need of
children and families for mental health
services.
Training provided for police department
personnel in suicide prevention and
family problems.
Teacher organizations provided with
education services in the form of leetures on clinical subjects.
Education provided on request to
organizations and agencies.
It is anti-
cipated that the information giving
program will increase requests to
Golden State for education services.
Information giving is to be done by Center staff,
Community Advisors,
para-professional staff, and by
professional mental health staff in conjunction with
education services.
Local businesses, legal agencies,
social agencies
64
and all organizations are to be identified from the
telephone directory,
chamber of commerce list of
organizations and churches and Information and
Referral Service (INFO).
Information is to be provided in person or by
mail to the following local resources or
11
care-givers"
and to others as needs are identified:
Beauty schools, beauty shops,
and
cosmetology conventions.
Bars
Churches
Parole Officers
Judges
Local hotels having residents
Apartments and motels having residents.
A relationship is to be established with the local
school for developmentally disabled children.
has children up to age 18.
The school
Consultation and education is
to be provided to the health education/learning rehabilitation staff at the school, including program design for
sex education.
4. 5. 3
Outreach and Follow.,.up
Outreach is encompassed in the education and
65
information giving activities in the form of case finding
and referral development through contacts with other
agencies and organizations.
Outreach is to be done by the alcoholism counselors and members of the mentally disordered offenders
program staff (MDO).
An outreach program for senior citizens and
residents from board and care homes in the catchment
area is to be developed by a committee, including a
staff member from administration, medical staff, nursing
department and partial hospitalization department.
(A
program which provides a visit to one board and care
home each week by clinical staff for consultation on
resident patients is already under way).
Follow-up is coordinated in the Intake Office.
Present plans include adding a mental health worker to
the Intake staff to develop a better system of documentation of follow-up activities and to insure that all patients
are contacted within a month after the last outpatient
visit and disposition of the case has been made.
The Intake workers currently follow-up on all contacts which do not result in the caller becoming a client.
Clients who are discharged from one service and
66
referred to another within the Center receive a follow-up
contact to insure .continuity of care.
Clients referred to other agencies receive appointments made directly by the Intake Office.
In an effort to improve relations and communications
with referring agencies, intake and administrative personnel participated in a six-week seminar conducted by
the Center for Training in Community Psychiatry and
sponsored by Los Angeles County.
Participants included
professional staff from California Services Section,
Metropolitan State Hospital,
Departure Center,
Camarillo State Hospital
the County Hospital and all major
public and private mental health facilities in the area of
the Center.
The topic was continuity of care.
The
objective of the seminar was to develop understanding
between mental health facilities about the faults in the
mental health system which allow clients to "fall through
the cracks".
The result has been better communication
between agencies about clients who are being referred
because the professionals have become acquainted with
each other.
4. 5. 4
Community Advisors Organization
A review was made of the literature on
67
community participation in health care since the 1960 1 s.
A position paper was developed and presented for adoption by the Centerr s Board of Directors to become the
basis for the development of a Community Advisors
Organization.
The Community Advisors organizational structure
was based on the requirements of the Center• s Constitution and By-laws as mandated by the National Institute
of Mental Health.
An analysis of the Center Intake statistics was
made to determine the census tracts in the catchment
area from which the Center receives the least patients.
The Advisor program development and the recruitment
of members has been designed to meet the needs indicated by the previously described demographic analysis
of the patients served in the Center.
Advisors were
selected from census tracts served by the Center to
reflect demographic makeup of the catchment area.
The Community Advisors were organized and have
been meeting regularly since October,
1974, one or two•
times monthly.
Currently the group has seventeen members and is
growing rapidly as a result of community contacts being
68
made by its members and Center staff.
Four Committees have been formed as follows:
Policy and Program Review
Community Communication
Monitoring and Evaluation
Alcoholism
The Committees were formed to address the basic
objectives adopted by the Advisors when the group was
organized.
1.
The objectives are as follows:
To assure that policy decisions are based
on awareness of the needs of the community through participation.
2.
To provide two-way communication with
the community served.
3.
To monitor the effectiveness of the services from the point of view of the
consumers.
The Committee for Policy and Program Review
addresses itself to assuring that the community has
representation in policy making and program design,
to fulfill objective No.
1 above.
The Committee has
studied material provided by Center staff on financial
structure and grants.
A summary has been prepared
for use in workshops to be conducted by the Advisors
for new members and,
eventually,
the community.
The Committee for Community Communication is
developing audiences for mental health,
alcohol,
and
drug abuse education programs in the community which
will be conducted by the staff with the help of the
Advisors.
The Committee has been assigned the task
of designing mechanisms for determining the kinds of
services and education programs desired by community
organizations,
churches and schools,
and the general
community.
The Monitoring and Evaluation Committee is in the
process of evaluating food services, intake practices and
procedures,
Center services,
and consumer satisfaction.
They have designed forms suitable for use in interviews
with personnel and professional staff,
and for use by
Advisors when sampling food.
Interviews and observations currently are being
conducted in each of the
by teams of Advisors.
departm~nts
of Adult Services
A team has completed food sur- •
veys and comparisons between employee food and patient
food served in the hospital and in the Center's Inpatient
and Partial Hospitalization Departments.
70
Advisors visited another community mental health
center in a neighboring area to compare the Center's
food service with the food service of another center.
The data collected in the food surveys were discussed in Advisors' meetings and recorded in the
minutes in the form of suggested areas for improvement.
All of the suggestions for improvement of food service
were feasible and are being implemented.
The Committee for Alcoholism serves as volunteers
and special Advisors to the Center's Alcoholism Program.
Aside from committee work,
the Advisors' main
activities have been directed toward increasing the size
of its membership so that additional committees can be
formed.
Other committees being considered are drug
abuse, volunteers,
recreation.
speakers bureau,
youth,
arts and
Other committees are to be activated
according to interest as membership increases.
Staff involvement with the Advisors has included
the following activities:
1.
Assistance to committee members in
information gathering and clarification
of written materials,
policies, and
71
structure of the organization.
2.
Technical assistance as provided by
administrative staff and the Alcoholism
Program Health Educator.
3.
Secretarial tasks,
keeping,
such as minute
mailing, typing,
telephoning,
and coordination of meeting facilities.
4.
Telephoning community organizations
and individuals to increase membership.
4. 5. 5
Other Changes
The Administrative Staff undertook public
relations and referral development activities such as:
Ombudsman duties for patients with
problems in g.ll categories, inside and
outside the Center.
This includes inter-
face with public social services agencies
to obtain food stamps and Medi-Cal cards,
medical care,
and problems between
patients and board and care home operators.
Improvement of the physical appearance of
72
the Center and food service to patients.
Communication and liaison between departments of the acute general hospital and the
Center,
particularly for emergency patients.
Formal calls on all agencies which refer
patients for mental health care, including
schools,
colleges,
hospitals, the
univer~ity
and
community services centers, and
the health department.
Better communication was developed between the Center and the Los Angeles
County Department of Mental Health Services
contract monitors and administrators.
This
was necessary to enable the County representatives to better understand the problems,
needs,
and goals of the Center.
Financial
constraints from opposing directions
between the State,
County and the Federal
Government concerning the management of
grants and contract requirements require
detailed explanation to monitors.
Expectations
73
for services and fiscal allocations to the
Center depend on a clear understanding
between all parties concerned of the
Center's capabilities.
The Administrative staff adopted a style
of participatory management to the extent
possible.
This includes regular scheduled
meetings between supervisory staff and
administration and an "open door" policy
to all levels of staff during each working
day.
The "open door" policy extends to patients
as well as staff in an effort to provide a
total therapeutic environment to the extent
possible.
------------------
--------------
__
.......
__ ----
Chapter 5
SUMMARY OF CHANGES
MADE TO INCREASE UTILIZATION
Over the past twelve months the Center has modified its
intake procedure, increased the black and Spanish surnamed
staff percentage to be more representative of the catchment
area population, trained staff to be more sensitive to social
needs of potential clients, developed crisis intervention techniques,
eliminated long term psychotherapy care,
established
a workload of 4. 5 clients per day (based on individual therapy),
introduced Problem Oriented Medical Records,
established
administrative review of excessive AMA 1 s and AWOL's, as signed
three or four outpatient staff members to an office and set
aside special offices for treatment,
eliminated so- called special-
ization for Inpatient and Outpatient therapists, and organized,
designed,
and initiated a comprehensive Indirect Services
Program, including education, information,
up,
consultation, follow-
and a community advisors organization.
The utilization of the Center was analyzed before and
after the implementation of the changes stated above.
sults are presented in Tables 22 through 26.
74
The re-
75
Table 22
Utilization of Services by Race
Before and After Changes
Race
Before Changes
June, 1974
After Changes
October, 1975
White
79%
66%
58o/o
Black
9%
18o/o
18%
llo/o
15o/o
22o/o
lo/o
1 o/o
2o/o
Spanish
Surname
Other
-~--------------
-"-------~
---- -......
---~-
. ----------
___ .. _
Goal
76
Table 23
Inpatient Service
Monthly Average Patient-Days per Calendar Day
for July, 1974 through June, 1975
77
...
Table 24
Partial Hospitalization Service (Day Treatment)
Monthly Average Patient-Day per Operating Day
(excludes weekend days and holidays)
for July, 1974 through May, 1975
Average
Patient-Days
Per Day
Month
Increase or
(Decrease)
Number of
Patient-Days
Re: July, 1974
Increase or
(Decrease)
Percent of
Patient-Days
Re: July, 1974
July
1974
42
Aug.
1974
37
( 5)
(11.9)
Sept.
1974
48
6
14.3
Oct.
1974
36
(6)
( 14. 3)
Nov.
1974
38
(4)
(9. 5)
Dec.
1974
42
0
Jan.
1975
36
(6)
( 14. 3)
Feb.
1975
56
14
33.3
Mar.
1975
47
5
11. 9
Apr.
1975
59
17
40. 5
May
1975
54
12
28.6
0
78
Table 25
Individual Therapy and Counseling Service
Monthly Average Units per Operating Day
(excludes weekend days and holidays)
for July, 1974 through May, 1975
Average
Units
Per Day
Month
Increase or
(Decrease)
Number of
Units
Re: July, 1974
Increase or
(Decrease)
Percent of
Units
Re: July, 1974
July
1974
23.41
Aug.
1974
20.03
(3. 38)
(14. 4)
Sept.
1974
27.66
4.25
18. 2
Oct.
1974
22.31
( 1. 10)
(4. 7)
Nov.
1974
26. 38
2. 97
12. 7
Dec.
1974
24.22
• 81
3. 5
Jan.
1975
22.03
( 1. 38)
( 5. 9)
Feb.
1975
35. 69
12.28
52.4
Mar.
1975
33. 78
10.37
44.3
Apr.
1975
35. 25
11.84
50.6
May
1975
33. 53
10. 12
43.2
79
Table 26
Inpatient Service Comparison
Comparison of Monthly Average Patient-Days
per Calendar Day for Contract Year - 1974/1975
to Contract Year 1973/74
Month
Average
Patient-Days
Per Day
1973/1974
Average
Patient-Days
Per Day
1974/1975
Ratio in
Percent}
of Average
Patient-Days
74/75 to
73/74
July
21. 68
17.81
82%
August
23.84
16.87
71 o/o
September
23. 10
18. 50
80o/o
October
24.64
18.29
74%
November
23.63
18.93
80%
December
21. 71
15. 39
71 o/o
January
23.45
20.39
87%
February
25. 89
20.21
78%
March
25. 52
21. 35
84%
April
21. 37
21.97
103%
May
21. 71
23.39
108o/o
June
18. 33
30.47
166%
80
It is seen in Table 22 that there has been a significant
change in the percent of Spanish surname and Black clients.
Referring to Tables 23,
24 and 25, it is shown that
utilization of services increased markedly from July, 1974 to
June, 1975.
For instance, inpatient services in June,
1975 were
31. 3% greater than in July, 1974; partial hospitalization services
in May, 1975 were 28.6% greater than in July, 1974; and individual therapy and counseling services in May, 1975 were 43.2%
greater than in July, 1974.
Table 26 which compares monthly utilization of inpatient
services between 1974/75 and 1973/74,
shows a distinct trend
toward increased utilization from the beginning of the contract
year (July,
1974) to the end of the contract year (June, 1975),
relative to the same period for 1973-1974.
For example, utilization for the first half of 1974/75
(July- through December) was 76% of the utilization for the same
period in 1973/1974.
On the other hand, utilization for the
second half of 1974/197 5 was 104% of utilization for that period
in 1973/1974.
This demonstrates clearly that the increases in
utilization shown in Tables 23,
or seasonal fluctuations.
24 and 25 are not due to monthly
Chapter 6
LOSSES DUE TO INAPPROPRIATE ADMISSIONS
AND EXCESSIVE SERVICES
Losses occur primarily in three ways:
Inappropriate
admissions, providing services in excess of Short-Doyle and
Short-Doyle/Medi-Cal allocations,
and providing services to
private clients who are either unable and/ or unwilling to pay.
6 •. 1
Inpatient admissions for services under Short-Doyle
must be approved by Los Angeles County Department of Mental
Health Services.
Clients for services under Short-Doyle/Medi-Cal
must present Medi-Cal cards at time of admission.
If Short-Doyle
patients are not approved by the Los Angeles County Department
of Mental Health Services the agency cannot bill for inpatient
services provided.
If current Medi-Cal cards are not presented
and copies retained, billing may be disallowed by auditors
although it was previously paid by the County based on data presented by the agency when the bill was submitted.
For prior years
this agency had permitted admissions based on eligibility as
determined by Los Angeles County Department of Public Social
Services.
The client was, under these circumstances, expected
to bring their card in when it was received from the State
81
82
Department of Health.
Often the State requested information that the
eligible Medi-Cal recipient was unwilling to provide.
11
so- called"
Often the
Medi-Cal eligible recipients did not bring their Medi-Cal cards
in after they had received them.
This problem was the cause of
several hundred thousand dollars loss per year.
A policy was
finally instituted that requires all applicants for Short-Doyle/
Medi-Cal inpatient services to present current Medi-Cal cards as
a condition for admission.
Admission to outpatient and partial
hospitalization services has not become a problem thus far but
it is being carefully monitored.
6. 2
Delivery of Services in Excess of Allocations
Contracts have specified allocations for inpatient, out-
patient,
and partial hospitalization services for both Short-Doyle
and Short-Doyle/Medi-Cal.
If an agency's total costs are below
-
the allocations the agency can collect such cost from the County.
On the other hand, if _the total cost for providing services is
above the allocation the amount that the cost exceeds the allocation represents a loss.
\
These types of losses are being kept under control by
providing management with better and more timely utilization
data so that contract allocations are not exceeded.
83
During the contract year 1973/1974 the Center provided
services in excess of contract allocations which resulted in
major budget overruns and losses to the Center.
These losses
for 1973/1974 are shown in Table 27.
Table 27
Comparison of Costs for Services
Provided in 1973/1974 to ContractAllocations
Cost of
Services
Allocation
for Services
Loss
1,291,958
747,166
Partial
Hospitalization
321,308
326,731
0
Outpatient
113, 639
163,310
0
Inpatient
544,792
$ 544,792
The Outpatient Department was analyzed for therapist
performance,
November,
reporting of patients seen,
1973.
and billing for
The results are shown in Table 28.
Referring
to Table· 28 it is seen that therapists provided an average of
2. 8 units of service per day which is 62% below the current
goal of 4. 5 units per day.
Further the table shows that only 486
units were billed to Short-Doyle and Short-Doyle/Medi-Cal.
Since collections for private patients amounts to only $2, 000 to
84
$3, 000 per month, it is clear that the bulk of units provided in
excess of 486 units represent a loss to the Center.
Table 28
Analysis of the Outpatient Department• s Performance
for the Month of November, 1973
Number of therapists
30
Number of full-time equivalent
therapists
26
Percent of therapist time ·spent
face-to-face with patients
35%
Number of clients per day per
therapist
2.8
Number of equivalent individual
units of service delivered
Average number of units billed
per Short-Doyle, Short-Doyle/
Medi-Cal 73/74 Contract
486
Maximum number of units billed
in any month per Short-Doyle,
Short-Doyle/Medi-Cal 1973/1974
Contract
768
·>!<Equivalent individual units represents
the total number of indivi.dual units
plus one-half the number of group
units.
Chapter 7
RESULTS AND RECOMMENDATIONS
7·. 1
Results
Unit costs for 1974/197 5 were compared to unit costs
for 1973/1974.
Unit cost, in this instance,
cost for a unit of service (i. e.,
represents actual
patient-day for inpatient ser-
vices and partial hospitalization services; and unit for individual
therapy and group therapy session).
It is calculated by adding
all expenses related to the service and dividing the resulting
amount by the total units of service.
The values referred to
here were taken from annual cost reports prepared by the
Center and submitted to the Los Angeles County Department of
Health Services as a condition for final settlement.
The results are shown in Table 29.
significant reduction in unit cost; however,
Table 29 shows a
the unit cost con-
tinued to exceed the provisional rate for all services.
It is
believed unit cost for 197 5/1976 will be within the provisional
rates which are $135.00 for inpatient days,
$39.00 for partial
hospitalization days, $32. 00 for individual therapy sessions,
$16.00 for group therapy sessions,
and $11.00 for medication
reviews for all mentally ill patients except mentally disordered
85
86
.
offenders (MDO) for which individual therapy is $24. 00 and group
therapy is $12. 00 per unit.
Provisional rate is an estimate of
unit cost agreed to by the Los Angeles County Department of
Health Services and the Center.
Costs were reduced $538, 302.
Of this amount
$288, 302 was due to a reduction in expenses and $250, 000 was
due to establishing an equitable method of allocating indirect
expenses between the Center and the Hospital.
(See Table 30).
An expense budget was established for 1975/1976 which
is expected to stay within the estimated revenue budget for the
same period.
The expense and revenue budgets are shown in
Tables 31 and 32.
Revenue over expense is shown in Table 33.
Adequate staff is being provided to meet demands for
service so long as expense budget limits are not exceeded.
It
is the intent of the Center to provide the maximum number of
units within budgetary limits in order to reduce unit cost by
spreading fixed costs over a greater number of units.
Quality of care has not been reduced as a result of any
actions taken to reduce unit cost or to meet budget requirements.
As a matter of fact,
-~
there is evidence that quality may have
increased, as indicated by the following indirect indices of
quality.
87
Table 29
Unit Costs for Services for Contract
Years 1973/1974 and 1974/1975
74/75
Provisional
Rate
Service
73/74>:~
74/75>:~
Inpatient Day
$227.01
$147.73
$130.00
Partial Hospitalization Day
50. 34
38.43
38.00
Individual Therapy
Session
39. 11
34.24
32.00
Group Therapy
Session
19. 57
17.45
16. 00
Medication Review
13.04
12. 57
10.00
*Taken from 1973/1974 and 1974/1975 Cost Reports
submitted to Los Angeles County Department of
Mental Health in accordance with Short-Doyle,
Short-Doyle/Medi-Cal Contract.
88
Table 30
Summary of Cost Reductions
Cost Reductions Due to Savings
1.
Employee Salaries and Benefits
2.
Rent, Taxes, Utilities and
Telephone
$ 213, 302
Relocation of Administration &
Accounting
17,000
Relocation of Social R ehabilitation Services
13, 000
3.
Ancillary Services
23,000
4.
Dietary
10,000
5.
Building Services, Engineering, and
Maintenance as a result of consolidation of offices
6,000
Single-view chest x-ray
6,000
6.
Subtotal
$ 288, 302
Cost Reductions Due to Method of Allocating
7.
250,000
Indirect Services
Total
$ 538, 302
Table- 31
Expense Budget for July 1, 1975/June 30, 1976
Inpatient
1.
2.
3.
Employee Salaries
& Benefits
Rent, utilities, taxes
& telephone
Outpatient
Regular
Subtotal
Outpatient
MDO
Total
$663,547
$233, 109
$157,189
$1, 0 53, 845
$140,864
$1,194,709
86,847
34,982
9,284
131, 113
12,364
143,477
105,876
105,876
105, 876
Misc. medical services,
22,233
supplies & laundry
22,233
22,233
100,717
100,717
Ancillary Services:
Radiology
Laboratory
X-ray
Other
4.
Partial
Hasp.
13,055
44, 571
38,250
10,000
5.
Dietary
69,696
31,021
6.
Building services and
maintenance
39,927
15, 724
8,985
(continued next page)
.
'
64,636
11, 9 50
76, 586
00
...!)
Table 31 (continued)
Inpatient
7.
General hospital
administration,
including general
accounting, billing,
credit & collections,
purchasing, personnel & insurance
8.
10.
Outpatient
~ular
Subtotal
Outpatient
MDO
Total
71,630
28,210
16, 120.
115, 960
21,440
137,400
3,428
10,284
3,428
17, 140
4,559
21,699
Operating costs
20,255
26,613
9, 312
56, 180
18,000
74, 180
Grant management,
including community
outreach, consultation & education, data
processing and reporting, and community involvement
14,932
5, 881
3, 360
24, 173
4,469
28,642
$1,098,371
$385,824
$207,678
$1,691,873
$213,646
$1,905, 519
Non-medical
supplies
9.
Partial
Hasp.
...0
0
'·
.
'
Table 32
Revenue Budget - July 1, 1975/June 30,
1976
Partial
Hosp.
Outpatient
Regular
560,503
$289,473
$ 61, 29 5>:<
80,878
21,672
38, 531
141,081
$216,000
Grant Revenue
(NIMH &: NIAAA)
260, 104
82,609
55, 70 5
398,418
24,958
Medicare
104,025
50,000
12,000
166,025
166,025
48,000
48,000
48,000
104,025
104,025
7,400
20,000
20,000
$222,931
$1,788,820
Inpatient
Short-Doyle/Medi-Cal
Short-Doyle
$
Private Payments
(Supplementary to
Short-Doyle)
Private Payments
Other Income
Total
104,025
12,600
$1,122,135
$443,754
Subtotal
$
Outpatient
MDO
911,271
Total
$
$240,958
911,271
423,376
$2,029,778
>:<If the current trend continues,, the Center will use only
$61,295 of its total allocation of $111,295.
....0
I-'
Table 33
Revenue Over Expense for July 1, 1975/June 30, 1976
Partial
Hosp.
'Inpatient
Outpatient
MDO
Outpatient
Regular
Budgeted Revenue
$ 1, 122, 135
$ 443,754
$ 222,931
$ 240,958
Budgeted Expense
1,098,371
358,824
207,678
213,646
Revenue over
Expense
$
23,764
$
57' 930
$
15,253 .
$
27, 312
Revenue over expense does not represent surplus funds to the Center for most revenue
source categories, inasmuch as Short-Doyle (including MDO), Short-Doyle/Medi-Cal,
and Medicare are reimbursed on the basis of cost.
-.o
N
93
1.
Patients are seen within 24-hours after calling
the Center.
2.
According to evaluations performed by the
Los Angeles County Department of Mental Health
Services, the Center's performance, as determined by the reduction of patients' global scores,
has been comparable to other contract community
mental health centers operating in the County.
A "Client Episode Outcome Summary" form is
included in Appendix C.
3.
The evaluation of the Center's medical records
by the State was above average.
4.
The evaluation of the Center's staffing level and
procedures by the State was satisfactory.
{This
evaluation is designed to determine only whether
or not centers meet minimum State criteria).
5.
Medical records were upgraded to
in~lude
a
Problem Oriented Medical Records system.
6.
Indirect services, including follow-up, were expanded to include all components required by NIMH.
94
7.
Greater coordination between Inpatient, Partial
Hospitalization,
and Outpatient services was
implemented thereby improving continuity of
care.
8.
The Inpatient program was improved by establishment of a more structured rehabilitation
program.
9.
Physical facilities were improved as a result
of expenditure of funds for painting, maintenance,
and furniture,
and the donation of paintings and
plants by friends of the Center.
7.2
Recommendations
While the Center's fiscal operation has been improved by
the actions discussed in the. paper,
there remain a number of
actions which have the potential for producing further reductions
in unit cost, increasing the capabilities of the Center to meet
dema:nds for services and improving quality of care and responsiveness to the needs of residents of the catchment area.
7. 2. 1
Recommendations to Improve
Delivery of Services
In order to increase the Center's capability to
meet demands for services and improve responsiveness
to the catchment area, it is recommended that the
95
Center:·
a)
Make an effort to increase its Short-Doyle
allocation by requesting more County funds
and/ or trading Short-Doyle/Medi-Cal funds
for Short-Doyle funds with other contract
agencies.
The Center has an insufficient
Short-Doyle allocation in relationship to
its Short-Doyle/Medi-Cal allocation.
b)
Develop a plan for obtaining United Way
(United Crusade) funds on a regular basis.
The Center does not currently receive
United Way funds although it is located in
a low-income area.
c)
Take action to obtain poverty area status.
'Qnder NIMH and NIAAA grant funding,
poverty status of the Center 1 s catchment
area would result in an increase in grant
revenue of 300%.
d)
Take action to obtain Los Angeles County
contract for both inpatient (detoxification)
and outpatient alcoholism and alcohol abuse
96
services.
e)
Conduct several fund raising events each
year.
f)
Develop programs to increase Medicare
patient utilization.
This could be achieved
by developing a geriatric service with an
outreach element geared to the elderly.
g)
Develop a special outreach program to
reach Spanish surnamed populations.
h)
Lobby for legislation similar to Senate
Bill No.
90 of Colorado which requires
the inclusion of mental health services in
health insurance plans which operate in
the state.
i)
With regard to Short-Doyle clients, develop
and implement an improved procedure for
(a) determining client's ability to pay, and
(b) collecting fees for services from clients.
7. 2. 2
Recommendations to Achieve
Additional Cost Reductions
In order to achieve additional cost reductions
it is recommended that the Center:
97
1.
Develop a more extensive volunteer
program.
2.
Develop internship programs for administrative personnel, nursing personnel,
and
other clinical personnel.
3.
Analyze the telephone system and investigate the potential advantages of extended
dialing telephone lines.
4.
Review the advantages of operating a
dietary department within the Center
rather than continuing to contract for
dietary services from the hospital.
5.
Install a dictaphone system for Outpatient
therapists.
6.
Provide Outpatient therapists with clerical
support for the handling of forms and
other clerical work associated with the
Outpatient services.
Chapter 8
CONCLUSIONS
A properly managed community mental health center can
maintain unit cost within reasonable provisional rates, maintain
its expense budget at or below its revenue budget and meet
minimal mental health needs of the community.
The success of the facility will be dependent upon its
Short-Doyle and Short-Doyle/Medi-Cal allocation and/or grant
revenue.
It also can be stated that community mental health
centers cannot survive without the support of local and federal
funding.
While physical health services are covered extensively
by employer insurance programs,
such coverage for mental
health services in communities served by this Center are grossly
(
inadequate.
98
BIBLIOGRAPHY
Brugess, John H.
"Who Has the Administrative Skills in
Mental Health, 11 Public Administration, March/ April,
1974, 164-167.
Center for Training in Community Psychiatry. "Program
Models for Emergency Mental Health Services, 11 Course
No. IX- 21, Howard J. Par ad, D. S. W., Coordinator,
1974.
Controller General of the United States. Report to the
Congress, Need For More Efficient Management of
Community Mental Health Centers Program, August 27,
1974, 18-31.
Ozarin, Lucy D.
"PSROs and Mental Hospitals; A Report, 11
Administration in Mental Health, Department of Health,
Education, and Welfare, Alcohol, Drug Abuse, and
Mental Health Administration, Public Health Service
Publication No. (ADM) 75-192, Spring, 1975, 19-22.
National Institute of Mental Health. Consultation and Education,
A Service of the Community Mental Health Center, U.S.
Department of Health, Education, and Welfare Public
Health Service, Public Health Service Publication No. 14 78,
1966.
Silber, Stanley C., ed. Multiple Source Funding and
Management of Community Mental Health Facilities, DHEW
Publication No. (ADM) 74-66, 1973, 29-32.
Strickler, Martin and Jean Allgeyer. 11 The Crisis Groups:
A New Application of Crisis Theory, 11 Social Work,
Vol. 12, #3 (July, 1967), 28-32.
Van Buskirk, David. ''Training and Treatment Costs in a
Community Mental Health Center, 11 Administration in
Mental Health, Summer, 1974, 28-36.
99
APPENDIX A
Selected sections of Los Angeles County
Department of Mental Health Services
"Uniform Method of Determining Ability
to Pay. 11 (UMDAP).
STATE OF CALIFORNIA
DEPARTMENT OF HEALTH
UNIFORM METHOD OF DETERMINING ABILITY TO PAY
FOR
COMMUNITY MENTAL HEALTH SERVICES
(Revised July 1, 1973)
100
101
State of California-Health and Welfare Agency
DEPARTMENT OF MENTAL HYGIENE
744 P Street
Sacramento 95814
June 1, 1973
Pursuant to the provisions of Sections 5717 and 5718
and other applicable sections of the Welfare and Institutions
Code,
the ability of patients, their estates, or responsible
relative to pay for services received from a Community Mental
Health Service under a County Short/Doyle Plan, other than in
a qtate hospital,
shall be determined by a local mental health
service pursuant to the provisions set forth in the Department's
Uniform Method of Determining Ability to Pay for Community
Mental Services as revised.
IN WITNESS WHEREOF I have fixed my hand and seal
as Director of Mental Hygiene this 1st day of June,
1973.
Andrew G. Robertson
Director of Mental Hygiene
102
QUESTIONS REGARDING OPERATION OF THIS
PLAN MAY BE DIRECTED. TO THE LOCAL
PROGRAM SERVICES SECTION OR THE PATIENT
BENEFITS AND ACCOUNTS SECTION, ROOM 650,
744
11
P 11 STREET, SACRAMENTO,
CALIFORNIA
95814, TELEPHONE AREA CODE 916 - 445-0625,
ATSS NUMBER 485-0625.
103
UNIFORM ME TROD OF DETERMINING ABILITY TO PAY
TABLE OF CONTENTS
PAGE
SECTION
1
1.
POLICY
2.
INTRODUCTION
2-3
3.
HOW THE PLAN WORKS
4-5
4.
PROCEDURES
5.
4. 1
General Procedures
4.2
Operational Procedures
4. 2. 1
Payor Financial Information
Form
4.2.2
As set Determinations
4.2.3
Allowable Deductions From
Income
4.2.4
Not~ce
of Patient Liability
4.3
Redetermination Procedure
4.4
Review Procedure
6-7
7
7-9
10
10-11
11
11-12
12
DEFINITIONS
EXHIBITS
(A)
Payor Financial Information
Form and Instructions
17-19
(B)
Monthly Charge Schedules
20-24
(C)
Income Conversion Chart
25
(D)
Suggested Letter of Charge
Explanation
26
104
1.
STATEMENT OF POLICY
It is the policy of the Department of Health that
mental health services supplied by the Department of
Health and Community Mental Health Programs shall be
charged for in accordance with the Department's
Uniform Method of Determining Ability to Pay.
That no
person shall be denied service because of ability or inability to pay.
That the amount to be paid in each
individual case shall not exceed the cost of services
received.
That each patient has the right to request
a review of any charge determination in accordance with
policies established by the Director of Health.
105
2.
INTRODUCTION
2. 1
Authority
The Welfare and Institutions Code vests the Director
of Health with the responsibility for determining the liability of Short/Doyle patients.
Section 5718 allows the
Director of Health to delegate this responsibility to the
counties.
If he elects to delegate,
the law requires he also
establish and maintain the policies and procedures for
making such determinations.
To fulfill these legal require-
ments, A Uniform Determination of Ability to Pay Plan, has
been devised.
The Plan will be provided to each county
delegated the responsibility by the Director of Health so
they may comply with the law.
The Plan was developed from the coordinated efforts
of the Department of Mental Hygiene Fee Collection Policy
Committee,
the Fiscal Subcommittee of theJ Conference of
Local Mental Health Directors,
and numerous knowledgable
State, County and Federal employees.
2. 2
Objectives
The objectives of the Plan are:
1.
To provide an equitable and uniform method of
106
determining ability to pay for Short/Doyle services
provided to a family unit.
2.
To standardize maximum charges consistent with
ability to pay.
3.
To develop a plan whereby there is a potential
source of revenue from every patient treated.
4.
To provide a method of determination that is easily
understood,
simple to employ, and adaptable to a
wide variety of operational settings.
5.
To recognize and provide for regional variances
within the State of the basic economic factors used
to develop the method.
6.
To provide a uniform procedure for review of charge
determination when requested by the patient.
107
3.
HOW THE PLAN WORKS
l.
An amount will be charged based on family size,
income assets and allowable deductions, exclusive
of third-party liable sources, but in no case will
the amount charged exceed the cost of the service.
2.
To achieve equity in determining amounts to be
charged a Monthly Charge Schedule is employed.
The charge schedule takes into consideration income,
family size, and average expenditures by family
size and geo-economic areas of the State.
3.
To achieve simplicity of operation two basic documents are used to determine ability to pay; a Payor
Financial Information Form and a Monthly Charge
Schedule which is related to a specific geo-economic
area.
4.
The Payor Financial Information Form when properly
completed contains the economic factors - Incomeassets-allowable deductions- size of family-necessary
to determine the charge by easy referral to the
applicable Monthly Charge Schedule.
108
How the Plan Works (continued)
5.
The Monthly Charge Schedules reflect variations in
the cost of living by family size and income by
geo-economic areas· of the State.
on the U.S.
They are based
Bureau of Labor Statistics Consumer
Price Index.
6.
Policies and procedures have been established to
provide for the review of ability determinations on
petition of the patient as well as annually for the
purpose of up-dating the determinations to current
conditions which may or may not have changed
during the previous year.
7.
Current Bureau of Labor Statistics reports were
used to develop the monthly charge schedules.
These reports take into consideration variances in
geo-economic factors affecting income and living
expenses by family size.
Each county has been
assigned a charge schedule applicable to its geoecon:omic index as reported by the Bureau of Labor
Statistics.
These schedules will be adjusted periodi-
cally in accordance with changes in the cost of living.
APPENDIX B
APPLICATION OF MBO PRINCI:PLES TO THE INTAKE
DEPARTMENT OF A COMMUNITY MENTAL HEALTH
CENTER.
Length of Time:
Eight Months.
Budget:
$20,000 Per Year.
\
Purpose:
To increase the responsiveness of the Center to the
mental health care needs specific to its service area,
to be mea:sured by a 32% increase in clients who live
in eleven high mental illness risk census tracts.
109
110
Application of a Management by Objectives System
to the Intake Department of a Community Mental
Health Center
Top Management
Board of Directors
Goals of the Community Mental Health Center
To· serve the mental health care needs of all races
and cultures of people, at all levels of risk for
mental illness, in the service area of the center.
Administrator
Mission Statement:
Administrator
To increase the utilization of the community mental
health center by all residents of the Center's service area who need mental health services, with an
increase of 32% (from 18% to SO%) of residents
from the eleven census tracts a:t highest risk for
mental illness, by effective reorganization of the
Intake Department, in cooperation and consultation
with the Board of Directors and the Community
Advisors.
111
First Line
Supervisor
Mission Statement:
Intake Supervisor
To increase the responsiveness of the Intake Department personnel to specific needs of the community
residents at greatest risk to mental illness by costeffective management of Intake procedures; to provide
training and community orientation to professionals
who will perform intake evaluation at first contact;
to provide evaluation for all contacts on an immediate
basis; to assume responsibility for implementing the
missions of the Board of Directors and Administrator
on a day-to-day basis in the Intake Department.
PRIMARY FACTORS TO CONSIDER
Type of Effort
A specific increase of clients from a designated
area in the Center's service area is to be achieved.
Time
An increase of thirty-two percent of clients who
live in a designated area is to be achieved in
eight months.
112
Major Recipient of Effort·
Residents in the Center's service area who need
mental 'health services.
Primary Work Factors
Human skills.
Items. Which Affect Primary Work Factors
Past attitudes,
procedures, experiences.
Attitude of community residents.
Extent of need for training of personnel.
Work patterns of professionals affected
by increased work load.
Significant Environmental Variables Which
Affect Measurement of Success of Project
Seasonal fluctuation in mental health facility
population.
It rises in January and lowers
in summer.
Ability of residents to financially qualify for
care.
Resources to pay for services, i.e., :M;edi-cal
Medicare,
private insurance and indigent care.
113
Space available in Center.
Personnel/ client ratio.
Objectives of the Administrator
To inform the Center personnel,
clinical and
non-clinical, of the need and reasons for
reorganization of the Intake Department and
obtain concurrence by November 15,
197 5
within the current budget.
To hire and orient an Intake Supervisor to
begin work by December 1, 1975,, at a cost
of $10, 000 per year.
To provide initial evaluation of clients by
professional intake therapists on an immediate
basis beginning January 1, 1976,
within the
current budget.
To install a dictation system for the use of
Intake Therapists in the Intake Department by
January 1, 1976,
at
a
cost of $4, 200 per year.
To hire a "floating" parafes siona1 counselor to
assist Intake Therapists,
as needed, by
114
January 1,
197.6, at a cost of no more than
$4, 800 per year.
To establish bi-monthly policy evaluation and
revision meetings between representatives of
Intake,
Clinical Staff,
Board of Directors and
Community Advisors, Accounting and Administration, beginning January 15, 1976,~ to continue on a permanent monthly basis after
1976~
April 30,
within the current budget.
To prepare, with Intake Supervisor and policymakers,
a final evaluation of the level of
utilization of the Center by residents of the
specific high- risk census tracts based upon
data collected for bi-monthly reports, by June 30,
-
1976~
within the current budget.
Objectives of the Intake Supervisor
To design,
supervise, and coordinate the
implementation of a one year clinical and
sociological inservice training program for
Intake personnel, including Therapists, PBX,
Receptionists, Volunteers and Financial Coun-
.
selors, using appropriate community mental
115
health care consultants, in one month, beginning
December 1, with training to begin January 1,
t.
1976, at a cost of $1, 000.
To prepare, in cooperation with the Administrator,
staff,
and policy makers,
a format for bi-monthly
Intake policy evaluation and revision meetings,
using appropriate data on client intake to be
presented with list of current problems, at least
I
~
three working days before the first meeting on
January 15,
1976, within the current budget.
To report to Administration on a weekly basis on
client flow,
space needs,
personnel needs, and
productivity, beginning January 7, 1976,
within the
current budget.
To supervise the PBX, Reception, Financial
Counseling, Intake Therapists (except clinical
matters}, and Medical Transc-ribing personnel, in
weekly meetings on an ongoing basis, beginning
December 1,
1975, within the current budget.
To develop and implement a system for determination of availability of therapists not on Intake. duty
116
to provide clinical backup for Intake Therapists
within one month beginning January 1,
1976,
within the current budget.
..
To evaluate and revise the permanent Intake
Policy and Procedure Manual and forms in
consultation with the Medical Directory, on an
ongoing basis, beginning May 31,
197,6, within
the current budget.
To design and implement two inservice training
sessions for personnel who work in 24-hour
emergency units in other locations,
to begin
March 1, 1976,; within the current budget.
To consult with Intake Supervisors and personnel
at other locations on evaluation of training needs,
beginning May 1,
1976, within. the· current budget.
To assist administration and policy makers in
final evaluation of the level of utilization of the
Center by high":'risk census tracts based upon
data collected for bimonthly reports, by June 30,
197'6, within the current budget.
117
PROGRAMMING AND SCHEDULING
Objectives of the Administrator
Working'
Days
Objective 1.
Inform all Center personnel of reorganization
and gain concurrence.
a)
Prepare presentation
b)
Meeting one: presentation
c)
Meeting two: feedback and questions
d)
Summarize feedback in writing for inclusion
in program
Total time -
5
10 .
15 consecutive days
Objective 2.
Hire and orient Intake Supervisor
a)
Hire Intake Supervisor
10
b)
Orientation
10
c)
Assumes position·
Total time - 20 consecutive days
Objective 3.
To provide professional intake evaluation of
clients on an immediate basis.
a)
b)
Develop daily 1 - 5 schedule for therapist
intake duty, with therapists
10
Change :weekly group meeting and administration meeting schedules to mornings
only
10
118
Objectives of the Administrator (continued)
c)
d)
Working
Days
Change psychiatrists' meeting schedules
to free their time for evaluations for
admission to inpatient service
10
Implement new schedule
Complete January l
Total time - 30 days (10 concurrent days)
Objective 4.
To install a dictation system.
a)
Hire medical transcriber part-time
b)
Purchase dictaphone
c)
Arrange location for transcriber
d)
Implement system
Complete January 1
10
5
Total time - 20 days (10 concurrent days)
Objective 5.
To hire "floating" para-professional part-time.
a)
Hire para-professional
b)
Train and orient para-professional
c)
Assume position
Complete January 1
Total time - 20 consecutive days
Objective 6.
To establish regular bimonthly Intake policy evaluation. and revision •
.
5
15
'.
119
Objectives of the Administrator (continued)
a)
Working
Days
Prepare and distribute memorandum
detailing objectives of reorganization
5
Hold initial meeting with principles
who have policyinaking positions
1
c)
Review and refine data to be collected
5
d)
First regular meeting
e)
Subsequent bimonthly meetings
b)
Complete January 15
Total time - 11 consecutive days
Objective 7.
To prepare final evaluation of program.
a)
b)
Meet with Intake Supervisor and policymakers to present evaluation from point
of view of management
1
Receive written report from supervisor
9 days
later
Complete June 30
Total time -
15 consecutive days
120
PROGRAMMING AND SCHEDULING
Objectives of the Intake Supervisor
Working
Days
Objective I.
a)
Obtain outside consultation
10
b)
Consult with administration staff
10
c)
Develop outline and schedule for
weekly speakers and evaluation of
results
10
d)
Begin training
Complete January 1
Total time - 30 days (20 consecutive days)
Objective 2.
To prepare format for bimonthly evaluation and
revision of policy, in cooperation with supervision.
a)
b)
Intake planning meeting with principal
policymakers, administration, staff and
data clerk
1
Compilation of results of meeting, preparation of initial policy" and procedure manual
9
c)
First regular meeting
d)
Subsequent bimonthly meetings
Complete January 15
Total time - 10 consecutive days
121
Objectives of the Intake Supervisor (continued)
Working
Days
Objective 3.
To report to Administration on weekly
basis on client flow, etc.
a)
b)
Prepare reporting format summarizing changes which occur as a result
of increased client load
20
Begin reporting
Complete January 31
Total time - 20 consecutive days
Objective 4.
To supervise PBX, Reception, Financial
Counseling, Intake Therapists (except in
clinical matters), and Medical Transcribing
personnel, on a weekly basis.
a)
b)
c)
d)
Prepare format for meetings which
provide opportunity to learn of problems
on a current basis
20
Prepare format to collect Intake personnel attitude and evaluation program
20
Prepare a summary of appropriate
information on policy and procedure
changes which occur as a result of
increased client load
20
Begin meeting
Complete January 31
Total time - 60 days (20 consecutive days)
122
Objectives of the Intake Supervisor (continued)
Working
Days
Objective 5.
To develop system for backup therapy.
a)
Meet with administration and supervision
b)
Consult with outside professionals
c)
Implement system January 1
Complete January 1,
1
19
1976
Total time -20 consecutive days
Objective 6.
To evaluate and revise permanent Intake
policy and procedure manual and forms
Complete June 30,
1976
Total time - 20 consecutive days
Objective 7.
To design and implement inservice training,
24-hour personnel
a)
Consult outside professionals
b)
Coordinate logistics with supervisors
in other locations; establish schedule
for two sessions
c)
Design course
d)
Begin training
Complete March 1·, 1976
Total time - 45 days (40 consecutive days)
20
5
20
123
Objectives of the Intake Supervisor (continued)
Working
Days
Objective 8.
To consult on a regular basis with Intake
supervisors at other locations on training
needs.
a)
Evaluate training needs of Center after
3 month's experience, in writing.
b)
Interview Intake supervisors at other
locations using written evaluation of
Center needs for comparison monthly.
c)
Begin consulting
Complete May l,
197 6
Total time - 20 consecutive days
Objective 9.
To prepare final evaluation of program.
a)
Meet with all Intake personnel
l
b)
Meet with Adminisfration and policymakers
1
c)
Collect data from bimonthly reports
d)
Compile written report
e)
Present to Administrator
Complete June 30,-1976
Total time - 15 consecutive days
12
1
124
SCHEDULE - INTAKE SUPER VISOR'S TASKS
EVE~T
Nov
15
Dec
15
Jan
15
Feb
15
Mar
15
Apr
15
}..!ay
15
_-:me
15
-----~--~~--,r-~.r~~r-~~-~~=---~-~--r-~~-~~=---~~~~
I
1 a
-=------+---!
...:l_b=--....:d=-----t----r·.,_.~~·--~--lo.-------:r-----+-----+----f-----l
Z a-c
9 b-e
3 a-b
4a
"1
~---------+---------+-----------+--------+---------~-----4
~4_b~------+-------r-~·~~~~~~~------~------4-------4-------~----~
....
4 c-d
---~~
--~--~~----+-------4-----~-----4----4
5 a-c
·~-·1
---r----+---?1, ~~-+-~
. - - ! - - - - + - - - t - - - - - : - - __
-=-6
.
j
"1 :
..:.7_a;;;.__ _ _-+----4-----:--··- ., .....____,. -.......------'-----+----+-----+---+
I
7b
I
~--.~.~-------+------~-----+----4
j
7 c
8 a-c
9 c-d
..
.
125
SCHEDULE - ADMINISTRATOR '5 TASKS
EVENT
. ---·
'
1 a-d
z a-c
,
15
.... -
'
Jan
15
Dec
Nov
15
Feb
15
Mar
15
Apr
15
May
15
.
~··~
... ._L,-,.._,_,
!'
!
3 -a
t
3b
'
.
3c
'
4a
'i
~
'
4b
i
4 c-d
.i
.:·
~
5 a
5 b-e
~
·;
-·
I
.
!:
------ '
'
,
6 a
'
!.
I
·'·
7b
!
_j
f1
6 b
6 c-7a
1
'
tl
j
'
I
I
·I
i
j
I
I
;I
'i.
126
BUDGET
The program will be implemented through reorganization of
present staff time,
rather than addition of new staff, with
the following exceptions:
Yearly Cost
Intake Supervisor
$
10,000
Medical Transcriber, part-time
4,000
Para-professional, part-time
4,800
Consultants for training programs
1, 000
200
Dictation machine
Total Yearly Cost
$
20,000
APPENDIX C
CLIENT EPISODE OUTCOME SUMMARY
COMMON
PROBLEM
DEFINITIONS
OEPR:SSJON:- Aepo'~'§: ot s~l;)'"!Ctl\18 le~lirtgs and concerns and
auoc ... r~d wHh the dev~:,.:,,,....~ -.yr1tome.
psvcho~.:ull
dysfunctions that may be
12
2
Af'J)( 1ZTY - ?~-:oorts -.. ' :;u:.. :;.!c~·ve ~~~··!"' . J1 and .::.,:,ncrJr rs. ar.c p~·,cnou~·. suJiC.';•Cal dysfunction' that
may t:.o! as:.OCI.:J\x.l ..... un :l~e J.nJuC:•.Jo;, phco.c. or c:.~ess•v'l!-<:lJmp·.. ls,;a sync.;~:orncs.
3
INA??;tOl'RIATE AFFECT, APPEARAI~CE, OR cEHAVIOR- Appcardnce, phy•ical behav•or,atacts
v.hic.h wouid be consi~o:~~~d oJ;J or inappnJiJfldte t., most untrain~ persons.
4
NEGATIVISM-OSSTINANCY -Refusal to answ..- que.tions or cooperate: withholding information.
15
18
21
5 AGITATION-EXCITEI,:ENT - O•ert siqns of ago:ation or excitement; (e.g., inability to sit still, pacing,
handwringing, acceleraHd speech. hyperac:~rvity).
·
24
6 MOTOR RETARDATION-LACK OF EMOTION- Visible <igns of retardation in speech and movem..,t,
a tent!encv to ignore the surrounc:ngs and
flatteni~~
of affect or qenerall~ck of emotional expression..
27
7
SPEECH DISORDERS - lrr~a""'ent on the form or organiza:ion of spei!Ch (e.g., blocks, rambles, is
inc:oharent, stutters, ''babytatKs''}.
30
8 SUSPICION-PERSECUTION-HALLUCINATIONS- Distrustfulness: feelings of having been mistreated,
taken advantage of, ~ricKed, or ptJshed around; ideas of reference; various paranoid delusions; auditory
hallucinations which mock, threaten, or command.
33
9 GRANDIOSITY - Inflated appraisal of his wort~. contacts, power, or knowledge: boasting: sensati•mal
plans; delusions of power, status, k.nowledg1f: _or contact; and hallucinations ¥IIIith a grandiose connotation.
36
10 SUICIOE·SELF-MUTILATION- Suicidal thoughts, preoccupation, threats, gestures or
thoughts or acts of self~mutilation.
i'
a~empu.
and
39
11 SOMATIC CONCERN-PHYSICAL PROBLEM - Real or
ima~ined
phys.cal <omplaint 0< disability;
conversion reaction; somatic delusion or hallucinations, hypochondrtasis; or body image con<:l'!rn.
42
12 DAILY ROUTio'-IE-LEISUR!: tiME IMPAIRMENT- The ;mpact o! psyc;,ooatnologv on dady rouune,
on car!Y'in,J rhr:J~gh ~;f-a:J(.;clm:~J o:- exoected talks. and on usualletsure t1me or recreatiooat activities
(e.s ... .:::Hiculty i:1 ari~ir; ;r; :-·~ mcrning, ;'!t"!:ing d·~'!iSed, and tra·,eling).
13 REPORTED OVERT .>.NGER - Reported or
o~<etved
45
overt anser or belligerence: shouting. tempe<
tantr~ms.
48
14 DISORIENTATION-Me10n 'f !'.~PAIRMENT - Visible signs of disorientation as to time, place, and
perSCii':s, and ltr.OJirme~: in r~ent or remote me~cry.
51
15 SOCI.!t.L lSCC.ATION - L.3;..:< of friencs. avoidaf'\C! of contact or involvement w1th O[hers. and fee4tngs
of iso:l<.ion.
rej~tion, :;~ :11~.::>r:-:f.::t
with pe'Jple.
54
16 MATLirtAT!O'\:AL PR03LE •• !S- Failurl! to ·acr.l!ve age appropnate interpersoNll or famii·t relationships; andior age appro;>r,ate a\lat):ive behavior te.;.. work, school).
57,
17 OE!'-Ji..l.L CF ILLNESS- 1'--~ e'(:e.,t !O ..·.n.ch tt-~ patient deniet. despite :~e I!V:Cence, thar "'''liS current·
svmp:-.Jms t-:-1we i;;vct- ;;·:~·-c : ::-.~.Clnce. ~ndt he :s. ill cr neeas psychiatr.::. helD-, or that t-.e n~s to
cnan.;e his atti~~o.;- •r. :;;..,e ~::-.;:;;;!c ;Nay,
18 ANTISOCIAL OR ILLEGAL ACTSin
min~r
L1·i~g:
or sa"illUS illeplor delinquent
60!
steal.cg; swindling: conning; ccmmission of or involvement
~cts..
63~
· 19 ALCOHOL ABUSE - The degree to wr.•ch use of alcohof is excessive, ce>mpulsive, causes physical
sy:npt·.:ms or alteration in m'=!od or behavior. or irnerferes with performar.ce of expected dally routine
ortiu:,~.
65
20 DRUG ABuse - E"c~ssive self-medication ana habituation or addiction to narcottc:s. batbitu..tes.
stimul3nts. or conscious~e'SS'-altering substances..
69
21 DANGER TO OTHERS- !--las m3de serious threJ:s of violence or actual assaults agaimt other penonJ
(violence 3qainst property not included); child abuse.
72i
22 IMPULSE CO~TROL - L..:a::i-.s se•f-disc.ip!.nP: r~'"'nses to 1t1m~..;li ellceed :imi~; ot elltpect~ beh3\'ior;
respo:-:.A.H to s;:;muli a~~ w;~:tuut regard to conse-.. .Jences; or itr'pu•s.n to comm1: dehnquent or l11egal
acts.
175
23 SEXUAL PROBLEMS~ Sex role confusion; eng<>~ in sexual ben;roior whicn is defined as unar:<:eQtable
by seif, family. or socie!y..
178
24 PROLONGED EXPOSURE TO POOR ENVIRO'<MENTAL CONDITIO~;s - Such as lonq-tetm disturbe-J family relatio1·!~•P!, chrvntc dysfunct.c:-: '":g or ab~nc~ cf a sit;nificanc othet"; ps--.,.c.hOsocia!
depriv..naon.
·
81
25 SITUATIONAL CRISIS- A dec·ease in ability to cope woth actual or threatenod loss related to self·
image, role mas.:ery or r~lationship with a signihcant other.
84
26 HOUSEKEEPER ROLE- A:lmissoon of doing a p~or job as a hou<ek.eeper, no p!easure or sarost.>euon
in an-. ~'!:u•.-ct lo)t huus~- .Jkf rJt.:tles: m<l ... ked d•scor-•.:trt or \.hfficu:t'f' with. or refus.:JI c:o carry r;.ut. one or
t1'Vlre ~1C.pec: ..•d .._ou':ieh-:'d ta-.k~. ·
87
21 WAGE EARXEii-:R=-o=L-::E:-~-i"'~-o"'i-n-te_r_es_t_o_r_sa_t_os-fac-,-.o-n-in_o_n-e'"'s-,o-b_;_d_r-ea_d_o"'l_o_n_e-_s_w_o_r_k_:f~a-ol_u_r_e-to-mee--t-+----;=­
task stJnd;srds. need 1 cr constant ~upef'll•s•on: ;>!ycf'\opathoiQ9Y incerlere-s wHn work; ex~sive Job
ch:..n~t!i; or hsr.~·n•J orh:-~1! t{J .~...iH·tirnc. tc•nf;tJfJ:--.. or u.:.n~~~nt ~""~''' hec.J .. ~ •lf t.J'!iychopatt •. ·1,:~
90
Poor mottv::.!H:tn; avo•Uance \if ciVdtl.s:.;le eAtrJcurnculd" act•-.•ues:
rn•::w~~ t.:IJs~c:.: :Jiff1cu ;y drJ'".'I ho"'eV'WO~k or a~.~nments; po.Jf -Jradus, ru~tod ~or exr,ns.~ help, or,
28 STUDENT OR TRAir...EE ROLE -
~~r.nfln.. t ~~:r, r.- -..:hc:rr. ..•· u~n ···':::'-:--''-:'-;~'t..-:::--n._-:-::-:-------:-----:----------:----+----t9=3'21J "•ATt RO•-t ".'ARIT,:\.L PF'1ALC~S- Alh.•r.:t•: 'JtQ l~>,~i'n''' t.:·~•v eJtf..~t1cnct.'d ur expre"":.m; many
quarrel"; littte or nu se"wl .::cuvnv: few shJred fr,~,ds or S<X;Ja! .~C!Ivlllct.
-~-~--~---------------~------:-:---------------:--·--:-------t-----1·9~1
~h,ld·t.:..J•• l.nks; reclutfiOil com~t.lefal'J:fl! h,•tg to
~.- --
30 PARENT HOLE - lr'.H •l•lV 10 .;..arry our •mrtO'~Jnt
m.m.... ~ ch•ltl, moJrb•d ~"·.us ul t:h•IJ ue1nq •nauh."f.t ~· •II.
"---------=--------------··cu~iiU~_~!~"f2 7'£
•;*"
cu~~
----J.---_,,. ,_
c. ,,.J., ...
l/\ii\)H'--1,'\TI' ...-:--;.....
.J
.'J.
--------