Heat Transfer in Living Tissue Chapter 10:
advertisement
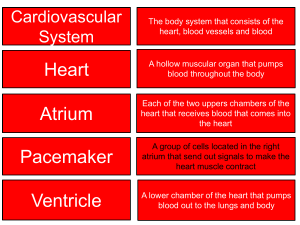
Chapter 10: Heat Transfer in Living Tissue 10.1 Introduction • Focal point: Temperature distribution in blood perfused tissue. • Applications: cryosurgery, frost bite, hyperthermia, skin burns,…. • Thermal modeling: Must account for (1) blood perfusion, (2) the vascular architecture, and (3) variation in thermal properties and blood flow rate. • Objective: Formulating a heat equation for determining temperature distribution in blood perfused tissue.. 10.2 Vascular Architecture and Blood Flow • Blood is supplied to tissues and organs through a network of arteries and capillaries. • Blood is drained from tissue and organs through a network of veins and venules. • Size of arteries and veins diminishes in the direction of blood flow through the arteries. • Note vessel names and sizes illustrated in Fig. 10.1. 10.3 Blood Temperature Variation • Blood leaves the heart through the aorta at Ta 0 . • It flows through primary arteries, arterioles and capillaries where it either adds or removes heat from tissue depending on local temperature T. • At the capillaries thermal equilibration with tissue becomes complete. • Blood returns to the heart through venules, primary veins and vena cava. • Blood mixing due to venous confluence brings its temperature back to Ta 0 . 10.4 Mathematical Modeling of Vessels-Tissue Heat Transfer • Modeling seeks to predict temperature distribution. • Assumptions are made to simplify the complexity of the process. • Pennes bioheat equation is one of earliest and simplest models (1948). • Subsequent improved models are more complex. • Five models will be presented. 10.4.1 Pennes Bioheat Equation • (a) Formulation. Assumptions: • • (1) Equilibration Site: Arterioles. capillary beds venules. (2) Blood Perfusion: Isotropic. • (3) Vascular Architecture: Local vascular geometry plays no role. • • (4) Blood Temperature: Blood reaches the capillary beds at Ta 0 and equilibrates with the local tissue at T . Conservation energy for element E& in + E& g − E& out = E& • (1.6) Energy transport by blood is treated as energy generation qb′′′ qb′′′ = ρ b cb w& b (Ta 0 − T ) • Other terms in (1.6) follow Section 1.4. Equation (1.6) lead to the Pennes bioheat equation ∇ ⋅ k∇T + ρ b cb w& b (Ta 0 − T ) + q m′′′ = ρ c • • (10.1) ∂T ∂t (10.3) The first term in (10.3) takes on different forms depending on the coordinate system. (b) Shortcomings • (1) Equilibration Site: Thermal equilibration takes place in pre-arteriole and postvenule vessels and not in the capillaries. • • (2) Blood Perfusion: Not isentropic • (3) Vascular Architecture: Not considered. • (4) Blood Temperature. Pre-arteriole blood is not at core temperature Ta 0 and vein return temperature is not equal to the local tissue temperature T. (c) Applicability: Vessel diameters > 500 μm. Equilibration length to total length Le / L > 0.3. 10.4.2 Chen-Holmes Equation • Blood equilibration with the tissue occurs prior to reaching the arterioles. • Pennes perfusion term is modified taking into consideration blood flow directionality and vascular geometry ∇ ⋅ k∇T + w& b* ρ b cb (Ta* − T ) − ρ b cb u ⋅ ∇T + ∇ ⋅ k p ∇T + q m = ρ c • • w& b* is the local blood perfusion. • Ta* ≠ Ta 0 . ∂T ∂t • The third term accounts for energy convected due to equilibrated blood. • Directionality of blood flow is described by the vector u . Assumptions and limitations: (10.4) • Mass transfer between vessels and tissue is neglected. • Thermal properties are assumed the same as those of the solid tissue. • Vessels diameter < 300 μm . • Equilibration length ratio Le / L < 0.6. • Requires detailed knowledge of the vascular network and blood perfusion. 10.4.3 Three-Temperature Model for Peripheral Tissue • Three temperature variables are assigned: arterial Ta , venous Tv and tissue T . • Three vascular layers were identified: deep layer, intermediate and cutaneous layer. • Deep layer: Countercurrent artery-vein pairs that are thermally significant. • Intermediate layer: Modeled as a porous media • Cutaneous layer: Below skin. Independently supplied by countercurrent artery-vein vessels called cutaneous plexus. • Divided into two regions; (i) upper region with negligible blood effect and (ii) a lower region governed by Pennes equation. • This model is governed by seven equations: three in the deep layer, two in the intermediate and two in the cutaneous. • It accounts for the vascular geometry and blood flow directionality. • Detailed vascular data. • Require numerical integration • Detailed formulation of all equations will not be presented. A simplified form will be detailed in the next section.\ • The heat equations for the cutaneous layer for the one-dimensional case are: Lower region: d 2T1 dx 2 + ρ b cb w& cb Upper region: k (Tc 0 − T1 ) = 0 d 2T2 dx 2 =0 (10.5) (10.6) 10.4.4 Weinbaum-Jiji Simplified Bioheat Equation for Peripheral Tissue • The three deep tissue equations of the three-temperature model are combined into a single equation. • Conservation of energy accounts for: • • (1) Conduction through tissue, (2) conduction between vessel pairs and tissue, (3) energy transport by blood bleed-off between vessels and tissue. (a) Assumptions. • (1) Bleed-off from artery is equal to flow to vein. • (2) Bleed-off leaves artery at Ta and enters vein at the venous temperature Tv . • (3) artery and vein have the same radius. • (4) No axial conduction through vessels. • (5) Equilibration length ratio Le / L << 1 . • (6) Tissue temperature T is approximated by T ≈ (Ta + Tv ) / 2 • (10.7) (b) Formulation. Energy conservation for artery, vein and tissue for one-dimensional case (blood vessels and temperature gradient are in the same direction) gives ρc • ∂T ∂ = (k eff ∂T ) + q m′′′ ∂x ∂t ∂ x (10.8) k eff is the effective conductivity, defined as n ⎡ ⎤ k eff = k ⎢1 + 2 (π ρ b cb a 2 u ) 2 ⎥ ⎣ k σ ⎦ (10.9) σ = shape factor, for vessels at uniform surface temperatures with center to center spacing l , it is π σ= (10.10) cosh(l / 2a ) • k eff represents the effects of (1) vascular geometry and (2) blood perfusion. • These two effects are separated by rewriting (10.9). The variables a, σ , n and u depend on the vascular geometry. Conservation of mass and vascular geometry relate blood velocity u to inlet velocity u o . Thus ⎤ ⎡ ( 2 ρ b cb a o u o ) 2 (10.11) k eff = k ⎢1 + V (ξ )⎥ 2 kb ⎦⎥ ⎣⎢ • V (ξ ) = dimensionless vascular geometry function, independent of blood flow ξ = x / L = dimensionless distance L = tissue layer thickness u o = blood velocity at the inlet to the tissue layer at x = 0 • The coefficient (2 ρ b cb ao u o / k b ) is independent of the vascular geometry. It • 2 ρ b cb a o u o . kb The second term in (10.11) represents the enhancement in conductivity. • (10.12) into (10.11) represents the inlet Peclet number Peo = k eff = k [1 + Peo2 V (ξ )] (10.13) • The two regions of the cutaneous layer shown are governed by (10.5) and (10.6). • Eq. (10.5) is rewritten in terms of the Peclet number Pe0 . Blood perfusion rate w& b in the tissue layer is given by w& b = π no a o2 u o L (10.14) no = number of arteries entering the tissue layer per unit area.. (10.12) into (10.14) w& b = π no a o k b Peo 2 Lρ b c b (10.15) Define R as R= L1 w& cb L w& b (10.16) L1 = thickness of the cutaneous layer. (10.15) and (10.16) into (10.5) d 2T1 dx • 2 + π no a o k b 2kL1 RPe0 (Tc 0 − T1 ) = 0 (10.17) (c) Limitation and Applicability. • Eq. (10.8) gives accurate predictions for vessels smaller than 200 μm in dia. and equilibration length ratio Le / L < 0.3 . Experiments on the rat spinotrapezius muscle showed that (10.8) is valid for Le / L < 0.2 . • Eq. (10.8) is based on vascular architecture of peripheral tissues less than 2 cm thick. It does not apply to deeper layers and to skeletal muscles. 10.4. 5 The s-Vessel Tissue Cylinder Model • Motivation: Address shortcomings of other models • (a) The Basic Vascular Unit. • Different types of skeletal muscles have significant common arrangements shown in Fig. 10.10 • SAV = main supply artery and vein. • P = primary pairs. • s = secondary pairs. • t = terminal arterioles and venules • c = capillary beds. • • • • Vessel size decreases progressively from SAV to c. • Blood flow in the SAV, P, t and s vessels is countercurrent. • Each countercurrent s pair is surrounded by a cylindrical tissue. • The tissue cylinder is a repetitive unit found in most skeletal muscles. It is used to formulate a bioheat equation for aggregate of all cylinders comprising the muscle. (b) Assumptions. • (1) Bleed-off blood in vessels leaving the s artery is equal to that returning to the vein and is uniformly distributed along each pair. • (2) Negligible axial conduction. • (3) Radii of the s vessels do not vary along tissue cylinder • (4) Negligible changes in temperature between the inlet to the P vessels and the inlet to the tissue cylinder. • (5) Temperature field in the tissue cylinder is based on pure radial conduction with a heat-source pair representing the s vessels. • (6) The outer surface of the cylinder is at uniform temperature T local . (c) Formulation. • The s vessels are not in thermal equilibrium with tissue temperature. • Three temperature variables are introduced: arterial Ta , venous Tv and tissue T . • Three equations for the temperature field in the s vessels and tissue cylinder were formulated. • Solution to the Navier-Stokes equations gives the two-dimensional velocity field. • Tab 0 = bulk temperature of the artery at x = 0. • Tlocal = temperature of the artery, vein and tissue at x = L . (d) Solution. • • • Analytic solution to the three equations for the artery, vein and tissue temperatures were obtained. Solution gives Tvb 0 , the outlet bulk temperature of the vein at x = 0. Results for the special case: equal size blood vessels symmetrically positioned relative to the center of the cylinder, i.e., l a = l v ( Fig. 10.11). The dimensionless artery-vein temperature difference, ΔT ∗ at x = 0 is given by T −T A ΔT = ab 0 vb0 = 1 + 11 + Tab 0 − T local A12 ∗ where 2 A11 2 A12 −1 (10.18) l a2 ⎤ 11 ⎫⎪ 1 ⎧⎪ ⎡ A11 = − ⎨ln ⎢ R(1 − 2 )⎥ + ⎬ 4 ⎪⎩ ⎣⎢ R ⎦⎥ 24 ⎪⎭ A12 = (10.19) 2 l 2 cos φ l a4 ⎤ 1 ⎡R + 4⎥ ln ⎢ 1− a 2 4 ⎢l R R ⎥⎦ ⎣ (10.20) φ , l a and l are defined in Fig. 11. • (e) Modification of Pennes Perfusion Term. Conservation of energy to the blood at x = 0 gives the total energy qb delivered by the blood to the tissue cylinder qb = ρ b cb π a a2 u a (Tab0 − Tvb0 ) • (10.21) Using (10.18), equation (10.21) becomes qb = ρ b cb π a a2 u a ΔT ∗ (Tab0 − Tlocal ) Dividing by the volume of the cylinder π a a2 u a = ρ b cb ΔT ∗ (Tab 0 − Tlocal ) 2 2 πR L πR L qb (10.22) Volumetric energy generation due to blood flow qb′′′ is qb qb′′′ = π R2L Volumetric blood flow per unit tissue volume w& b (10.23) π a a2 u a w& b = π R2L (10.24) Eqs.(10.23) and (10.24) into (10.22) gives qb′′′ = ρ b cb w& b ΔT ∗ (Tab0 − Tlocal ) (10.25) Since R >> l , Tlocal ≈ T. Eq. (10.25) becomes qb′′′ = ρ b cb w& b ΔT ∗ (Tab0 − T ) • • (10.26) Equation (10.26) replaces eq. (10.1) used in the formulation of the Pennes equation. It differs from. (10.1) in two respects: • (1) Artery supply temperature is not set equal to the body core temperature. • (2) It includes the ΔT ∗ factor. Using eq.(10.26) in the Pennes equation (10.3) gives ∇ ⋅ k∇T + ρ b cb w& b ΔT ∗ (Tab 0 − T ) + q m′′′ = ρ c ∂T ∂t (10.27) • Note the following: • (1) The dimensionless factor ΔT ∗ is a correction coefficient. It it depends only on the vascular geometry of the tissue cylinder and is independent of blood flow. • (2) A closed-form solution is obtained for the determination of ΔT ∗ . Its value for most muscle tissues ranges from 0.6 to 0.8. • (3) The model determines the venous return temperature and accounts for contribution of countercurrent heat exchange in the thermally significant vessels. • (4) The artery temperature Tab0 in eq. (10.27) is unknown. It is approximated by the body core temperature in the Pennes bioheat equation. • Equations (10.5) and (10.6) apply to the cutaneous layer of peripheral tissue, (10.23) applies to the region below the cutaneous layer.