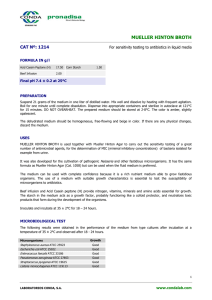
Mueller Hinton Results Introduction
advertisement

Mueller Hinton Results Introduction The choice of the proper media is important to ensure reproducibility of the performed tests. Many laboratory techniques may be used to in vitro evaluate bacterial resistance to different antimicrobial agents. Among these techniques, the disk diffusion susceptibility test is the most common, as well as the dilution tests in broth and agar. To obtain reliable and uniform results, the techniques used and the media and procedures employed must be standardized. The use of standardized culture media and careful control of all test conditions are fundamental requirements in the microbiological sensitivity testing in order to achieve satisfactory results. An antibiogram allows to in vitro subject a standard bacterial inoculum to one or different antibiotic concentrations and, after analyzing results, predict in vivo effectiveness. The interpretation of results (Sensitive, Intermediate or Resistant) is carried out on the basis of parameters previously established by a number of committees, such as The Clinical and Laboratory Standards Institute in the U.S., or The European Committee on Antimicrobial Susceptibility Testing. The standardized procedures are based on the Bauer-Kirby method. The following results are done according to The European Committee on Antimicrobial Susceptibility Testing. Routine and extended internal quality control as recommended by EUCAST. Version 5.0, 2015. http://www.eucast.org Procedure 1.- MEDIUM: the standard culture medium for the production of the antibiogram is Mueller Hinton (Cat. 1058) and Mueller Hinton II (Cat. 1055) , intended for the growth of many aerobic organisms. For fastidious organisms, such as streptococci and gonococci, 5% defibrinated blood must be added to Mueller Hinton and Muller Hinton II. Ready-to-use plates must be prepared following the data sheet instructions for each medium. 2.- PREPARATION OF MATERIAL: 4-5 colonies that show similar morphology are taken from the primary isolation medium with a flamed loop, and suspended in 4-5 ml broth: Mueller Hinton Broth (Cat. 1214), Trypticasein Soy Broth (T.S.B.) (Eur. Pharma)(Cat. 1224) or Brain Heart Infusion Broth (Cat. 1400). They are incubated at 37ºC for 2-5 hours. If there is turbidity at the end of this time, adjust the turbidity with a Mc Farland Standard Tube 0.5 (equivalent to a uniform suspension of 1.5x10 bacterial cells/ml). If the bacteria concentration is low, continue incubating for 3 more hours and adjust. 3.- INOCULATION INTO PETRI DISH: prepared bacterial suspension is homogenously mixed and streaked, turning the plate into the Mueller Hinton Petri Dish, with the help of a sterile cotton swab. Another technique is to pour several ml into the agar, distribute homogeneously and remove excess fluid. After inoculation, leave the plates unsealed for 10-15 minutes to allow for any surface moisture to be absorbed before applying the drug- impregnated discs. 4.- ANTIBIOTIC DISC APPLICATION: Allow containers to reach room temperature before opening. Open the CONDA Antibiotic discs cartridge under the flame and discharge the disc with the trigger or flamed and cooled forceps. Press the disc gently into the agar with the help of the forceps. The space between the discs must not be narrower than 24 mm, and the distance to the edge no less than 1 cm. CONDA Special Dispenser 6x and 8x may also be used. It is preferable to deposit penicillin and cephalosporin discs no less than 10 mm from the edge of the Petri dish, with their centers at least 30 mm apart. 5.- INCUBATION: Place the Petri Dish into the incubator inversely at 37ºC for 18-24 hrs. For Staphylococcus spp., testing at temperatures above 35°C may not detect methicillin- resistant staphylococci (MRS); for N. gonorrhoeae, incubate at 36 ± 1°C. Haemophilus spp., N. gonorrhoeae, S. pneumoniae and other streptococci should be incubated in an atmosphere enriched with 5% CO2. 6.- RESULTS: The diameter of the inhibition zone is read from the underside of the disc. If Mueller Hinton with Blood has been used, inhibition areas must be read from the surface with a compass or ruler. Zones are measured to the nearest whole millimeter. The inhibition areas must be evaluated according to the Table provided by CONDA. Escherichia coli ATCC 25922 Antibiotics EUCAST Range Competitor/mm MH/mm MH-II/mm Amikacin 30 µg 19-26 20 21 22 Ampicillin 10 µg 16-22 17 18 19 Cefoxitin 30 µg 23-29 24 24 24 Chloramphenicol 30 µg 21-27 26 27 Ciprofloxacin 5 µg 30-40 35 36 35 Gentamicin 10 µg 19-26 19 19 21 Levofloxacin 5 µg 29-37 32 35 34 Moxifloxacin 5 µg 28-35 29 30 30 Nitrofurantoin 100 µg 17-23 20 20 17 Norfloxacin 10 µg 28-35 30 34 31 Ofloxacin 5 µg 29-33 30 33 30 Tigecycline 15 µg 20-27 20 24 21 Tobramycin 10 µg 18-26 17 17 20 Trimethoprimsulfamethoxazole 1,25 - 23,75 µg 23-29 23 23 24 Cefotaxime 5 µg 25-31 25 26 27 Cefpodoxime 10 µg 23-28 22 25 26 Ceftriaxone 30 µg 29-35 27 30 30 Cefuroxime 30 µg 20-26 20 24 25 Doripenem 10 µg 27-35 27 30 30 Ertapenem 10 µg 29-36 31 33 32 Imipenem 10 µg 26-32 35 32 32 Meropenem 10 µg 28-34 30 35 33 Ticarcillin 75 µg 24-30 21 26 25 Piperacillin-Tazobactan 30-6 µg 21-27 21 23 25 Cefalexin 30 µg 15-21 13 16 18 Cefadroxil 30 µg 24-20 13 15 17 Aztreonam 30 µg 28-36 29 34 34 Amoxicillin-Clavulanic acid 20-10 µg 18-24 18 21 20 Cefixime 5 µg 23-27 20 23 23 Ceftazidime 10 µg 23-29 22 26 27 Piperacillin 30 µg 21-27 23 25 25 Ampicillin-sulbactam 10-10 µg 19-24 20 22 21 Ticarcillin-clavulanic acid 75- 10 µg 24-30 25 27 30 Mecillinam 10 µg 24-30 26 26 27 Ceftibuten 30 ug 27-35 25 27 28 Pseudomonas aeruginosa ATCC 27853 Antibiotics EUCAST Range Competitor/mm MH/mm MH-II/mm Amikacin 30 µg 18-26 25 26 26 Ciprofloxacin 5 µg 25-33 35 33 33 Levofloxacin 5 µg 19-26 24 26 26 Tobramycin 10 µg 20-26 22 21 24 Cefepime 30 µg 24-30 26 29 30 Doripenem 10 µg 28-35 34 35 35 Imipenem 10 µg 20-28 28 28 28 Meropenem 10 µg 27-33 35 33 33 Piperacillin-Tazobactan 30-6 µg 23-29 30 29 29 Aztreonam 30 µg 23-29 35 29 29 Ceftazidime 10 µg 21-27 23 27 27 Ticarcillin-clavulanic acid 75-10 µg 20-28 20 28 28 Antibiotics EUCAST Range Competitor/mm MH/mm MH-II/mm Amikacin 30 µg 18-24 20 20 21 Ampicillin 2 µg 15-21 17 19 16 Cefoxitin 30 µg 24-30 25 25 27 Chloramphenicol 30 µg 20-28 23 23 21 Ciprofloxacin 5 µg 21-27 20 22 21 Clindamycin 2 µg 23-29 28 27 26 Erythromycin 15 µg 23-29 20 24 25 Fusidic Acid 10 µg 26-32 26 26 26 Gentamicin 10 µg 19-25 19 20 19 Levofloxacin 5 µg 23-29 30 28 27 Linezolid 10 µg 21-27 25 24 22 Minocycline 30 µg 23-29 22 24 23 Moxifloxacin 5 µg 25-31 30 30 26 Mupirocin 200 µg 31-37 31 34 Nitrofurantoin 100 µg 17-23 17 17 20 Norfloxacin 10 µg 18-24 24 24 23 Ofloxacin 5 µg 21-27 24 25 25 Quinupristin-dalfopristin 15 µg 21-27 21 23 21 Rifampicin 5 µg 30-36 30 30 30 Tetracycline 30 µg 23-31 20 25 25 Tigecycline 15 µg 19-25 17 20 20 Tobramycin 10 µg 20-26 20 20 23 Trimethoprimsulfamethoxazole 1,25 - 23,75 µg 26-32 25 26 26 Staphylococcus aureus ATCC 29213 Haemophilus influenzae Haemophilus influenzae NCTC 8468 Antibiotics EUCAST Range Competitor/mm MH/mm MH-II/mm Chloramphenicol 30 µg 30-38 28 28 30 Ciprofloxacin 5 µg 31-39 35 35 34 Erythromycin 15 µg 12-18 14 15 15 Levofloxacin 5 µg 32-38 36 36 34 Minocycline 30 µg 27-33 30 33 32 Moxifloxacin 5 µg 29-35 34 35 34 Ofloxacin 5 µg 30-36 32 34 32 Rifampicin 5 µg 20-26 23 25 26 Tetracycline 30 µg 28-34 32 34 34 Trimethoprimsulfamethoxazole 1,25-23,75 µg 26-34 10 26 26 Cefaclor 30 µg 24-30 38 30 30 Cefepime 30 µg 29-35 32 34 33 Cefotaxime 5 µg 29-35 24 29 29 Cefpodoxime 10 µg 28-34 30 32 33 Ceftriaxone 30 µg 33-41 28 33 34 Cefuroxime 30 µg 35-31 35 31 31 Doripenem 10 µg 26-32 36 32 32 Ertapenem 10 µg 27-33 30 33 33 Imipenem 10 µg 25-31 40 31 31 Meropenem 10 µg 28-34 35 34 34 Telithromycin 15 µg 15-21 30 21 21 Amoxicillin-Clavulanic acid 2-1 µg 17-23 35 23 23 Cefixime 5 µg 27-33 17 27 27 Antibiotics EUCAST Range Competitor/mm MH/mm MH-II/mm Nitrofurantoin 100 µg 18-24 17 20 20 Tigecycline 15 µg 20-26 20 25 22 Imipenem 10 µg 24-30 25 30 30 Teicoplanin 30 µg 15-21 16 21 21 Enterococcus faecalis ATCC 29212 Streptococcus pneumoniae ATCC 49619 Antibiotics EUCAST Range Competitor/mm MH/mm MH-II/mm Chloramphenicol 30 µg 24-30 29 30 30 Ciprofloxacin 5 µg 22-28 28 28 28 Clindamycin 2 µg 22-28 23 24 24 Erythromycin 15 µg 26-32 27 29 29 Levofloxacin 5 µg 21-27 25 26 26 Linezolid 10 µg 23-29 27 28 28 Minocycline 30 µg 25-31 25 26 26 Moxifloxacin 5 µg 24-30 27 30 30 Nitrofurantoin 100 µg 25-31 26 28 28 Norfloxacin 10 µg 18-24 24 24 26 Ofloxacin 5 µg 18-24 21 21 21 Rifampicin 5 µg 26-32 28 30 30 Tetracycline 30 µg 28-34 29 32 33 Tigecycline 15 µg 24-30 23 24 24 Trimethoprimsulfamethoxazole 1,25-23,75 µg 20-26 30 25 26 Cefaclor 30 µg 25-31 33 30 30 Cefepime 30 µg 31-37 41 35 35 Cefotaxime 5 µg 28-34 35 32 32 Cefpodoxime 10 µg 29-35 36 33 33 Ceftriaxone 30 µg 32-38 36 38 38 Cefuroxime 30 µg 28-34 36 33 32 Doripenem 10 µg 31-37 32 31 32 Ertapenem 10 µg 28-34 33 30 30 Imipenem 10 µg 34-42 39 40 40 Meropenem 10 µg 30-38 36 34 34 Oxacillin 1 µg 8-14 9 10 10 Teicoplanin 30 µg 18-24 19 22 22 Telithromycin 15 µg 27-33 31 31 31