CHAPTER 42 Questions 1. Myelin can cause neuronal growth inhibition.
advertisement
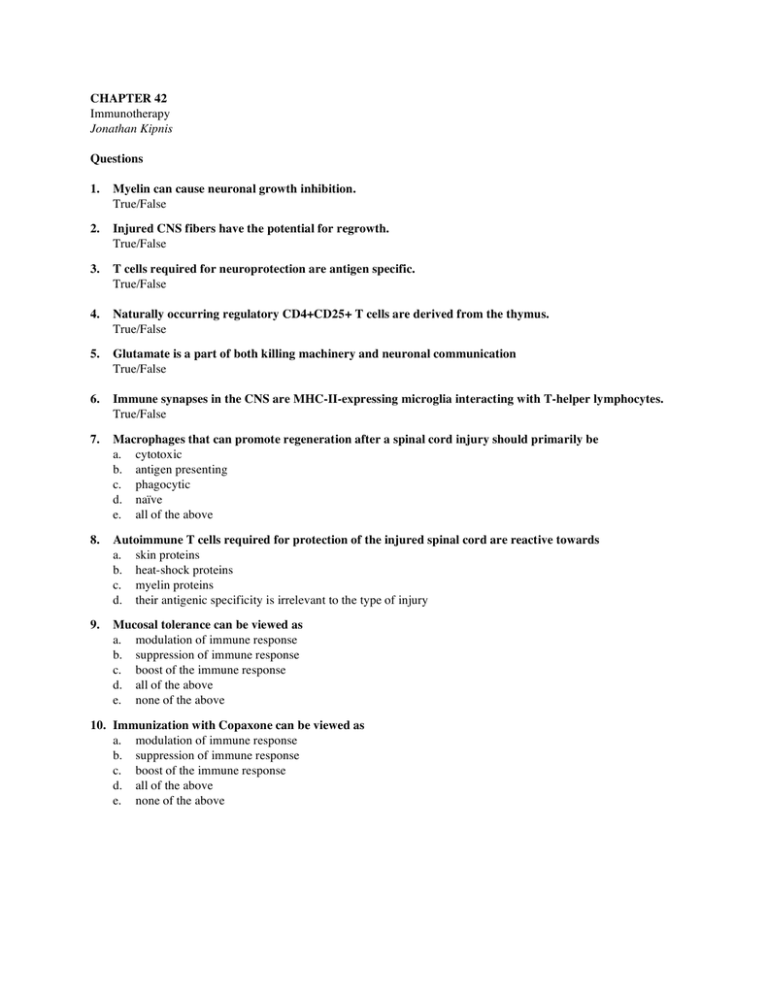
CHAPTER 42 Immunotherapy Jonathan Kipnis Questions 1. Myelin can cause neuronal growth inhibition. True/False 2. Injured CNS fibers have the potential for regrowth. True/False 3. T cells required for neuroprotection are antigen specific. True/False 4. Naturally occurring regulatory CD4+CD25+ T cells are derived from the thymus. True/False 5. Glutamate is a part of both killing machinery and neuronal communication True/False 6. Immune synapses in the CNS are MHC-II-expressing microglia interacting with T-helper lymphocytes. True/False 7. Macrophages that can promote regeneration after a spinal cord injury should primarily be a. cytotoxic b. antigen presenting c. phagocytic d. naïve e. all of the above 8. Autoimmune T cells required for protection of the injured spinal cord are reactive towards a. skin proteins b. heat-shock proteins c. myelin proteins d. their antigenic specificity is irrelevant to the type of injury 9. Mucosal tolerance can be viewed as a. modulation of immune response b. suppression of immune response c. boost of the immune response d. all of the above e. none of the above 10. Immunization with Copaxone can be viewed as a. modulation of immune response b. suppression of immune response c. boost of the immune response d. all of the above e. none of the above 42. Immunotherapy Jonathan Kipnis 2 11. Spinal cord injury is associated with a. axonal regrowth b. inhibition of axonal regrowth c. axonal sprouting d. none of the above 12. Neuroprotection induced by CsA under certain neurodegenerative conditions can be attributed solely to a. suppression of the immune response b. activation of the immune response c. induction of growth factors d. direct effect on glial cells e. none of the above 13. The role of immune cells in the CNS – is it destructive or protective? What are benefits of immune boost following injury and what are the possible devastating side effects of such therapy? 14. What is immune modulation and how it could be achieved? 15. Immune suppression is neuroprotective under certain circumstances whereas neurodestructive under others. How this apparent dichotomy could be resolved? 16. What is the evolutionary benefit from having a complex network of autoimmune and regulatory T cells? 17. Does the presence of BBB favors in favor or not of the role of immune system in post-injury recovery? 42. Immunotherapy Jonathan Kipnis 3 Answers 1. True 2. True 3. True 4. True 5. True 6. True 7. c 8. c 9. d 10. a 11. b 12. e 13. The role of immune cells in the CNS – is it destructive or protective? What are benefits of immune boost following injury and what are the possible devastating side effects of such therapy? Immune system involvement in the central nervous system (CNS) can be both protective and destructive. The outcome of the neuro-immune interaction depends on the context (i.e. in healthy or injured tissue), the nature of initiation of the immune response, its regulation, and successful resolution. Injured CNS will benefit from a well-controlled T cell immune response shortly after injury, but this response needs to be halted before the onset of deleterious side effects. The mechanism by which T cells regulate plasticity is as yet unknown, but in the healthy CNS, T cells assist in the maintenance of neuronal plasticity. Depletion of T cells in the periphery impairs CNS cognitive performance and adult neurogenesis. A severe inflammatory response following CNS injury may exacerbate rather than reduce neuronal death and the accumulation of T cells in a healthy CNS may result in paralysis. 14. What is immune modulation and how it could be achieved? Immune modulation, unlike immune suppression, is aimed at regulating the immune response, rather than eliminating it. For example, oral administration of a high dose of self-antigens will switch the T cells response from Th1 (pro-inflammatory) to Th2 (anti-inflammatory), and thus remodel the inflammatory process. Other types of immune modulation may be based on injection of regulatory T cells or injection of anti-inflammatory cytokines. Administration of self-like proteins that compete with self-proteins for presentation by MHC class II is another way of modulating the immune response. Presentation of self-like epitopes in the context of MHC class II results in an attenuated autoimmune T cell response, due to weak interaction with the T cell receptor. 42. Immunotherapy Jonathan Kipnis 4 15. Immune suppression is neuroprotective under certain circumstances whereas neurodestructive under others. How this apparent dichotomy could be resolved? Neuroprotection upon the suppression of immune activity is achieved when the immune system is over activated and the damage mediated by excess inflammatory metabolites outweighs the benefit induced by T cells. Thus, for example, the immediate immune response to injury is destructive and its elimination may benefit recovery from injury. Such immune suppression however, will only be beneficial overall if it is of restricted duration, and the later phases of the immune response (72 hours post injury and beyond), are not affected. 16. What is the evolutionary benefit from having a complex network of autoimmune and regulatory T cells? Autoimmune T cells are needed to protect “auto-organs” after injury. Having these cells in the periphery without tight control may result in their activation and the subsequent induction of autoimmune disease. Naturally occurring regulatory T cells keep peripheral autoimmune T cells in a state of tolerance (and readiness!). When damage to the tissue is inflicted, regulatory T cells sense it (hypothetically as a “danger signal”) and their suppression over effector T cells is relieved, allowing the latter to migrate to the tissue in need, and mediate a protective effect. When the “danger” signal from the tissue disappears, regulatory T cells regain their suppressive function and are thus able to suppress any ongoing inflammation. 17. Does the presence of BBB favors in favor or not of the role of immune system in post-injury recovery? The role of the blood brain barrier, (BBB) in post-injury recovery is unclear, depending on the nature of the injury itself, and the immune response. The BBB may be destroyed, or malfunction following injury. This can allow an influx of T cells into the CNS. The presence of an intact (or nearly intact) BBB (as in chronic neurodegenerative disorders, such as Alzheimer’s or Parkinson’s) slows down T cell influx, but because activated T cells, unlike naïve, can migrate across the BBB, its presence only eliminates the migration of non-specific T cells preventing the unwanted side effects of non-specific inflammation.