Document 14809582
advertisement

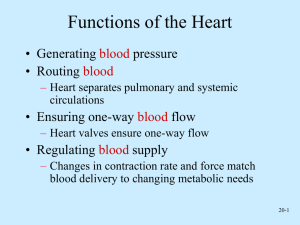
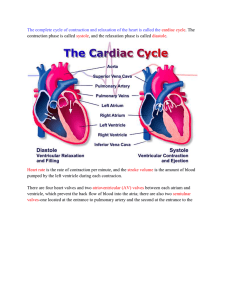
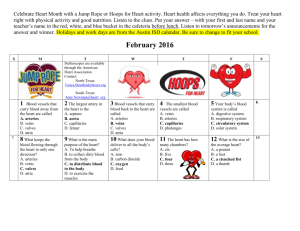
Interesting Facts At rest, the heart pumps 30xs its own weight each minute. There are 60,000 miles of blood vessels. In one day, the heart can pump 7000 L. In one year, the heart pumps about 5 million L. The average body contains about 5 L of blood volume. Functions of the Heart Generating blood pressure Routing blood – Heart separates pulmonary (lungs to left side) and systemic (O2 & nutrients) circulations Ensuring one-way blood flow – Heart valves ensure one-way flow Regulating blood supply – Changes in contraction rate and force match blood delivery to changing metabolic needs Size, Shape, Location of the Heart Size of a closed fist Shape – Apex: Blunt rounded point of cone (pointed bottom) – Base: Flat part at opposite of end of cone (rounded top) Located in thoracic cavity in mediastinum (b/w the lungs; 2/3 to left of center) Pericardium Encloses the heart and holds it in place Two layers: – Outer, fibrous pericardium prevents the heart from overstretching – The inner, serous pericardium contains pericardial fluid to prevent friction Heart Wall Three layers: – Epicardium—thin, transparent outer layer – Myocardium—cardiac muscle tissue; bulk of the heart – Endocardium—lines the inside of the myocardium and covers the valves Heart Chambers Two upper chambers: Atria – Receiving chambers – Separated by interatrial septum Two lower chambers: Ventricles – Pumping chambers – Separated by interventricular septum Thickness of Heart Chambers Vary according to each chambers functions. Atria—thin walls because they only pump blood to ventricles Right ventricle—pumps blood to lungs; slightly bigger than atria Left ventricle—pump blood to entire body and keep up with the other chambers; thickest of the four chambers Concept Check What are the functions of the heart? – Blood pressure, routing blood, one-way blood flow, regulating blood supply Name and describe the 3 layers of the heart. – Epicardium (thin/transparent outer layer), myocardium (cardiac muscle tisssue; bulk), endocardium (lines inside of myocardium & covers valves) What is the difference between atria and ventricles? – Atria receives blood; ventricles pumps blood Blood Vessel Structure Arteries – Elastic, muscular, arterioles Capillaries – Blood flows from arterioles to capillaries – Most of exchange between blood and interstitial spaces occurs across the walls – Blood flows from capillaries to venous system Veins – Venules, small veins, medium or large veins Valves of the Heart Four valves one for each chamber – They keep blood from flowing back to where it came from – They open and close in response to the pressure of blood against them Valves of the Heart Atrioventricular (cuspid) valves – Tricuspid valve — between right atrium and right ventricle; 3 flaps or cusps – Chordae tendinae — tendon-like cords that prevent the cusps from being pushed back – Bicuspid valve —between left atrium and left ventricle; two cusps Path of Blood Right atrium receives deoxygenated blood from 3 veins: – Superior Vena Cava—blood from above the heart – Inferior Vena Cava—blood from below the heart – Coronary Sinus—blood from the heart wall Vessels of the Heart Right Ventricle Blood goes from to the pulmonary trunk Pulmonary trunk divides into left and right pulmonary arteries Pulmonary arteries lead to the lungs From the Lungs Oxygenated blood enters the left atrium via four pulmonary veins From the Left Ventricle Blood enters the ascending aorta To the coronary arteries To the arch of the aorta To the thoracic aorta To the abdominal aorta Valves of the Heart Semilunar Valves – Pulmonary semilunar valve— between right ventricle and pulmonary artery – Aortic semilunar valve— between left ventricle and the aorta Blood Supply of the Heart Coronary Circulation—blood flow through the myocardium – Left and right coronary arteries bring blood to the tissue – Coronary sinus take deoxygenated blood from the tissue Blood Flow Through Heart Concept Check What are the 3 types of blood vessels? – Arteries, veins, capillaries Describe the flow of blood through the heart starting w/ the body. – Body, (SVC, IVC, CS), R Atrium, Tricuspid Valve, Chordae Tendinae, R Ventricle, Pulmonary SLV, Pulmonary Trunck, Pulmonary Arteries, Lungs, Pulmonary Veins, L Atrium, Bicuspid Valve, Chordae Tendinae, L Ventricle, Aortic SLV, Aorta, Body Disorders Ischemia —faulty circulation weakens cells due to lack of oxygen, but the cells don’t die Angina Pectoris —chest pain resulting from ischemia; also from stress, over exertion, high blood pressure, or narrow arteries Disorders Myocardial Infarction (MI) —heart attack – Infarction is the death of an area due to interrupted blood supply; usually from a clot – Tissue beyond the clot will die and become scar tissue – Location of the infarction area is key to how serious it is Conduction System of the Heart This is an intrinsic regulating system It does not need a stimulus from the nervous system All cardiac muscle is capable of selfexcitation Cardiac muscle generates its own action potential Sinoatrial (SA) Node Located in the right atrial wall just below the superior vena cava Known as the pacemaker of the heart – Rate of self-excitation is faster than all other heart fibers – Its impulses are spread to all the other areas thus setting the rhythm of the heart – Both atria will contract at the same time – This will then depolarize the AV node (ventricles contract) Atrioventricular (AV) Node Located in the interatrial septum Last part of atria to depolarize This impulse will depolarize fibers in the interventricular septum— bundle of His This is the only electrical connection between the atria and ventricles Atrioventricular (AV) Node The impulse passes toward the apex through left and right bundle branches to the ventricles The actual contraction of the ventricles is done by the Purkinje fibers Conducting System of Heart Electrocardiogram (ECG) A record of the electrical changes that accompany the heartbeat. Electrocardiogram Action potentials through myocardium during cardiac cycle produces electric currents than can be measured Pattern – P wave Atria depolarization – QRS complex Ventricle depolarization Atria repolarization – T wave: Ventricle repolarization Cardiac Arrhythmias Tachycardia: Heart rate in excess of 100bpm Bradycardia: Heart rate less than 60 bpm Sinus arrhythmia: Heart rate varies 5% during respiratory cycle and up to 30% during deep respiration Premature atrial contractions: Occasional shortened intervals between one contraction and succeeding, frequently occurs in healthy people Alterations in Electrocardiogram Cardiac Cycle Cardiac Cycle Heart is two pumps that work together, right and left half Repetitive contraction (systole) and relaxation (diastole) of heart chambers Blood moves through circulatory system from areas of higher to lower pressure. – Contraction of heart produces the pressure Concept Check Why does the SA node act as the pacemaker? How does the heart contract without an impulse from the brain? – Impulses are spread to other areas setting the rhythm of the heart – Intrinsic regulation / Self-excitation / Cardiac muscle generates own action potentials What actually contracts the myocardium of the ventricles? – Purkinje fibers What is an infarct? – Death of an area due to interrupted blood supply; usually a clot Concept Check What does an EKG measure? – Electrical changes in the heart that accompany heart beat Why is QRS bigger than P? – QRS = contraction of ventricles – P = contraction of atria What is a fibrillation or arrhythmia? – Fibrillation = heart’s electrical activity has become disordered; contraction rapid, unsynchronized; flutter rather than beat; heart pumps little or no blood Heart Rate Cardiac Output —amount of blood ejected from the left ventricle into the aorta per minute Stroke volume —amount of blood ejected from the left ventricle per contraction Factors Affecting Heart Rate Autonomic control —baroreceptors—neurons sensitive to blood pressure changes Chemicals —too much or too little K+, Na+, or Ca+ either increases or decreases heart rate; oxygen demands Temperature —increase temperature, increase heart rate; lower temperature, decrease heart rate Emotions —fear, anxiety, anger all increase heart rate while depression and grief lower heart rate Sex and age —faster in females; fastest at birth but slows as one gets older More Disorders Arteriosclerosis - thickening of the walls of the arteries and loss of elasticity Atherosclerosis - Deposition of plaque on walls Congenital defects—a defect that exists at birth – Interventricular septal defect—hole in septum – Valvular stenosis—narrowing of a valve – Arrthymia—any irregularity in heart rhythm Effects of Aging on the Heart Gradual changes in heart function, minor under resting condition, more significant during exercise Hypertrophy of left ventricle Maximum heart rate decreases Increased tendency for valves to function abnormally and arrhythmias to occur Increased oxygen consumption required to pump same amount of blood Heart Sounds First heart sound or “lubb” – Atrioventricular valves and surrounding fluid vibrations as valves close at beginning of ventricular systole Second heart sound or “dupp” – Results from closure of aortic and pulmonary semilunar valves at beginning of ventricular diastole, lasts longer Third heart sound (occasional) – Caused by turbulent blood flow into ventricles and detected near end of first one-third of diastole Blood Pressure Measure of force exerted by blood against the wall Blood moves through vessels because of blood pressure Measured by listening for Korotkoff sounds produced by turbulent flow in arteries as pressure released from blood pressure cuff Pulse Pressure Difference between systolic (contraction of ventricles) and diastolic (relaxation of ventricles) pressures Increases when stroke volume increases or vascular compliance decreases Pulse pressure can be used to take a pulse to determine heart rate and rhythmicity Concept Check What types of things would increase your heart rate? Decrease? What is a congenital disorder? Describe the problems with interventricular septal defect. What is the difference between systole and diastole if they both measure on the arteries? What causes the heart sounds?