Document 14777306
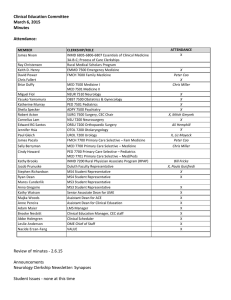
advertisement

Attendance: MEMBER James Nixon Clinical Education Committee June 6, 2014 Minutes Miguel Fiol Yasuko Yamamura Katherine Murray Sheila Specker Robert Acton Cornelius Lam Edward RG Santos Jennifer Hsia Paul Gleich James Pacala CLERKSHIP/ROLE INMD 6805-­‐6806-­‐6807 Essentials of Clinical Medicine 3A-­‐B-­‐C; Process of Care Clerkships EMMD 7500 Emergency Medicine FMCH 7600 Family Medicine MED 7500 Medicine I MED 7501 Medicine II NEUR 7510 Neurology OBST 7500 Obstetrics & Gynecology PED 7501 Pediatrics ADPY 7500 Psychiatry SURG 7500 Surgery, CEC Chair NSU 7200 Neurosurgery ORSU 7200 Orthopaedic Surgery OTOL 7200 Otolaryngology UROL 7200 Urology FMCH 7700 Primary Care Selective – Fam Medicine Sally Berryman Michael Kim MED 7700 Primary Care Selective – Medicine MED 7701 Primary Care Selective – Med/Peds Kathy Brooks Jacob Prunuske Stephen Richardson Ryan Dean Kathy Watson Suzanne van den Hoogenhof Brooke Nesbitt Chelsey Jernberg Mark Hilliard PED 7700 Primary Care Selective – Pediatrics INMD 7200 Rural Physician Associate Program (RPAP) Duluth Faculty Representative MS4 Student Representative MS4 Student Representative MS3 Student Representative MS3 Student Representative Senior Associate Dean for UME Measurement Specialist, Assessment & Evaluation Clinical Education Manager, CEC staff Clinical Scheduler Academic Technology Keith D. Henry David Power Briar Duffy ATTENDANCE -­‐ X X X X Deb Egger-­‐Smith X Jennifer Janacek X -­‐ X X -­‐ -­‐ X X X, Paula Guisfredi X X -­‐ -­‐ X X X X X Review of minutes 5.2.14 -­‐ approved as is Announcements: New Clinical Education Committee chair -­‐ Robert Acton New Neurology clerkship director -­‐ Miguel Fiol New MS4 representatives -­‐ Ryan Dean, Stephen Richardson Gold Humanism students (Power) -­‐ currently meeting in evening, which results in low attendance. If they were to meet at 8am (90 min mtg plus travel), every six weeks, how disruptive would that be to their current rotations? Excused? On average, would miss one half day per six-­‐week period? Dr Brooks asked if this would set a precedent for other requests for excused absences. Other clerkships shared concern about time of day -­‐ right in the middle of rounds. Would afternoon be better? RPAP shared that alums have had some luck leaving rotations around 3:30-­‐4:00pm in order to present for program. These GHHS students also leave rotations for ECM2 when possible and for facilitating FIPCC (six Friday afternoons). Dr Acton shared concern over students, in general, leaving required or elective rotations for extra curricular or administrative activities. Could be folded into absences-­‐related policies. Dr Prunuske suggested a pilot period be used to determine impact; also asked what the GHHS students' activities are during that time. Dr Power shared that in addition to teaching in MS1 courses, they plan the pre-­‐match retreat, Habitat for Humanity, etc. Meetings during the day/evening are to plan these events. Dr Duffy requested that only GHHS have this excused absence for committee meeting; at least for pilot period, no other groups will be approved for such absences. Updates: Medical Education Retreat (please refer to Slides handout) Critical Themes in UME from Survey -­‐ QI and Patient Safety, Public Policy and Public Health, Integrating Basic Science into Clinical Ed, New models of Clinical Education, IPE, Scholarship Advice to Medical School Faculty • Seek out partnerships • Understand the student experience • Actively seek and respect student input • Be aware of your influence as a role model for professionalism, lifelong learning, and critical thinning • Assess what content is core and what is expendable • Take advantage of faculty development opportunities • Accept and embrace change Operationalized through Workgroups -­‐ some are continuations of previous project groups; others are new efforts Example: Public Policy and Public Health • Environmental scan -­‐ what are we doing now? Surveys, focus groups, curriculum search • New educational activities -­‐ about public health and public policy across 4 years of medical school and both campuses (Power) • Evaluation tools -­‐ on effectiveness of new educational initiatives. • Digital Badge -­‐ criteria for advanced educational experiences • Faculty Development -­‐ assess FD needs for integrating new initiatives into curriculum COMMENTS: Dr Prunuske reinforced notion that Public Health is NOT only a Family Medicine issue; all specialties have a connection to public health and public policy. Dr Kim added that there are lots of opportunities to integrate into different specialties. Dr Rosenberg is administration lead on the Public Health/Public Policy initiative. Dr Henry asked what the current curricular model is for Public Policy -­‐ Dr Power introduced new sessions being implemented in ECM 3A by David Satin and Tyler Winkelman, including national speaker/medical resident Nathan Moore ("The Health Care Handbook"). Dr Santos shared that time in the Ortho clerkship may be limited for integrating public policy/public health, but that MS2 lectures they are active with may provide a more appropriate opportunity for integration. Dr Brooks shared that in any specialty, public health/public health issues can be worked in to any patient encounter. Dr Fiol (Neurology) added that introducing a large public policy/health initiative into a clerkship is difficult, must be done at school level. Several directors commented that its not a separate conversation, but rather part of the conversations that are already happening during patient encounters. Dr Prunuske agreed that what each clerkship can do will vary based on specialty, schedule, and student need. What is one thing you could do on your rotation to reinforce public health concepts? Dr Murray shared that our current block schedule limits our thinking about longitudinal concepts, such as public policy, but young trainees can use their new perspective to make connections. Student representative, Ryan Dean, shared that early clinical experiences, like ECM, would help students to develop those connections between issues and cases. Get students started thinking about these initiatives? Dr Duffy added that this issue is an opportunity to think longitudinally and develop best practices for integration and continuation. Discussion Step 2 CK Changes (please refer to Changes to USMLE 2014-­‐2015 handout) • Increased focus on QI, patient safety, epidemiology, biostatistics, population health, professionalism, interpersonal and communications skills. • Med Ed Retreat outcomes will connect with this increased focus (alignment) • Will continue to be administered electronically • Additional changes to Step 2 CS -­‐ internally we are changing institutional assessments to enhance the assessment of communication skills. Plagiarism common statement review -­‐ Statement will be distributed electronically • Multiple cases of plagiarism in medical school this year. • Cases referred to Peer Review Committee (great resource for recommendations, fantastic leadership, responsibility, policies). How would they feel about reporting out the numbers for the year? • In one case, student has subsequently submitted suggestions and recommendations for students. • Dr Murray requested that it be distributed and managed at program-­‐level, not clerkship level. • Dr Prunuske added that perhaps a generational, educational focus on IPE and teamwork has blurred line for some students as to what is the "team's" and what deserves reference or credit. • Dr Gleich expressed concern that this is even an issue; Dr Power responded that the case in FMCH was intentional, not an unawareness of what plagiarism is. • Dr Duffy asked if there was a university-­‐wide policy on plagiarism -­‐ answer is YES, but it has not been highlighted/applied specifically to Medical School • Dr Murray added that there is poor modeling in medical practice where physicians can copy notes on patients; Dr Prunuske countered that the case is a little different between patient notes and published work. Dr Brooks stated that EMR it is still an opportunity to practice clean documentation -­‐ "From the discharge summar..." • Dr Brooks queried if since perceived focus of years 3 and 4 is on clinical work, are papers and didactic work pushed to back burner. Dr Fiol wondered if workload is also a contributing factor. Diagnoses & Procedures List Review (please refer to PxDx list) • Instead of deliberating in CEC, request is for 1-­‐2 volunteers to review list and cut it down (1-­‐2 pages, 60-­‐100 encounters) to fewer diagnoses and procedures. • Dr Murray indicated she has done some preliminary work such as this for EPAC to remove duplication. Will partner with Dr Acton to review list. • Dr Kim asked if diagnoses could be linked. Or create general Dx or Px and use other data fields to differentiate. • Dr Brooks asked for clarification on whether requirement is to log encounter specific to each clerkship, or are directors satisfied if students have logged particular encounters in "some" clerkship. • Dr Fiol asked if there were specific guidelines for what diagnoses or procedures should be completed in each clerkship -­‐ he was referred by group to a specialty-­‐specific national organization. LCME does not have specific encounter requirements. No meeting in July!