I. Imaging of the Spine in Victims of Trauma II. Authors
advertisement

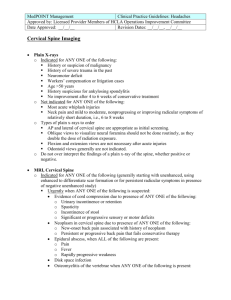
Back to Contents Page I. Imaging of the Spine in Victims of Trauma II. Authors C. Craig Blackmore, MD, MPH Department of Radiology Gregory Avey, MD Department of Radiology Harborview Medical Center University of Washington 325 Ninth Avenue, Box 359728 Seattle WA 98104 206-731-3561 fax: 206-731-8560 KEY POINTS ISSUES: 1. The cervical spine: A. Who should undergo cervical spine imaging? B. What imaging is appropriate in high-risk subjects? Special case: Defining subjects at high fracture risk Special case: The unconscious patient 2. The thoracolumbar spine: A. Who should undergo thoracolumbar spine imaging? B. What imaging is appropriate in blunt trauma patients? IV KEY POINTS: - Cervical spine imaging is not necessary in subjects with all five of the following: 1. absence of posterior midline tenderness, 2. absence of focal neurological deficit, 3. normal level of alertness, 4. no evidence of intoxication, and 5.absence of painful distracting injury. (STRONG EVIDENCE) - CT scan of the cervical spine is cost-effective as the initial imaging strategy in subjects at high probability of fracture (neurological deficit, head injury, high energy mechanism) who are already to undergo head CT. (MODERATE EVIDENCE) - No adequate data exists on the appropriate cervical spine evaluation in subjects who are unexaminable due to head injury. (INSUFFICIENT EVIDENCE) - Imaging of the thoracolumbar spine is not necessary in blunt trauma patients with all five of the following: 1. absence of thoracolumbar back pain, 2. absence of thoracolumbar spine tenderness on midline palpation, 3. normal level of alertness, 4. absence of distracting injury, 5. no evidence of intoxication. (MODERATE EVIDENCE) 1. Cervical Spine Issue A: Who should undergo cervical spine imaging? Summary Determination of which blunt trauma subjects should undergo cervical spine imaging, and which should not undergo imaging, is a question that has been studied in detail in literally tens of thousands of subjects. The two major Level 2 (Moderate Evidence) studies, the NEXUS trial and the Canadian C-spine Rule, were comprehensive multicenter investigations of this topic. The NEXUS rule has undergone extensive validation and demonstrates high sensitivity for detection of fractures. The Canadian Cspine rule also has high sensitivity, and potentially higher specificity than the NEXUS. However, neither of these rules has been tested in an implementation trial to determine their impact outside the research setting. Issue B: What cervical spine imaging is appropriate in high-risk subjects? Summary Cervical spine CT is more sensitive than radiography, and more specific in subjects at high risk of fracture. CT has higher direct costs than radiography. However, costeffectiveness analysis demonstrates that CT is cost-effective, and may actually be cost- saving from the societal perspective in subjects at high probability of fracture. Cost savings with CT are from a decreased number of second imaging examinations resulting from inadequate radiograph studies, and to the high cost in dollars and health for the rare fracture missed from radiography that leads to severe neurological deficit. Radiography remains the most cost-effective imaging option in subjects at low probability of injury. Special Case: Defining subjects at high fracture risk Summary Selection of subjects for cost-effective use of cervical spine CT is dependent on probability of fracture. The Harborview high-risk cervical spine criteria have been developed and validated by a single institution Level 2 (Moderate Evidence) study. Using these criteria, subjects can be identified with injury probabilities ranging from 0.2% to 12.8%. Special Case: The unconscious patient Summary The theoretical risk of radiographically occult unstable ligamentous injury in subjects who are unexaminable due to head injury has lead to a variety of imaging approaches. There is insufficient evidence to support any particular approach. 2. The Thoracolumbar Spine Issue A: Who should undergo thoracolumbar imaging? Summary Clinical prediction rules to determine which patients should undergo thoracolumbar spine imaging have been developed, but not validated. Although these prediction rules have high sensitivities for detecting thoracolumbar fractures, their low specificities and low positive predictive values would require imaging a large number of patients without thoracolumbar injuries. This drawback limits the clinical utility of these prediction rules [Moderate evidence]. B. What thoracolumbar imaging is appropriate in blunt trauma patients? Summary Multiple studies have shown that some CT protocols used for imaging the chest and abdominal visceral organs are more sensitive and specific for detecting thoracolumbar spine fracture than conventional radiography. In patients undergoing such scans, conventional radiography may be eliminated [Limited evidence]. The effect of primary screening with CT scan on cost and radiation exposure has not been thoroughly studied for the thoracolumbar spine. Back to Contents Page