USING CONFORMAL RADIOBIOLOGY TO FIND THE ‘BEST’ TREATMENT PLAN
advertisement

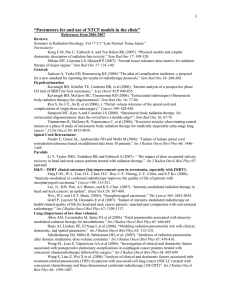
49th AAPM Annual Meeting, Minneapolis, 22-26 July 2007 USING CONFORMAL RADIOBIOLOGY TO FIND THE ‘BEST’ TREATMENT PLAN Alan E. Nahum PhD Physics Department Clatterbridge Centre for Oncology Bebington, Wirral Merseyside CH63 4JY UK Email: alan.nahum@ccotrust.nhs.uk Preface Physicists working in radiotherapy spend a lot of their time measuring doses in phantoms and then calculating the dose distributions in patients due to a particular arrangement of beams. This is because, according to the present state-of-the-art practice, the radiation oncologist prescribes the treatment in terms of a (uniform) dose to the target volume accompanied by some sort of constraint on the dose to one or more organs-at-risk. Well, this is not quite true, as today IMRT/‘inverse planning’ is forcing a change of this practice, but the philosophy has not changed i.e. prescription is done in terms of doses and volumes. However, it can be argued that the endpoints in radiotherapy that are truly of relevance are not dose distributions but the probability of (local) tumour control, often known as the Tumour Control Probability (TCP) and the Probability of Normal-Tissue Complications (NTCP). PART TWO of this course deals with the modelling of TCP and NTCP and how they can be actively used in treatmentplan optimisation with the emphasis on the spatial distribution of the absorbed dose within the target volume, though not forgetting that fractionation is an indispensible ‘degree of freedom’ in the search for optimal radiotherapy. Some of the reasons why models for TCP and NTCP might be useful follow (the references cited are not intended to be exhaustive): † Dose distributions in three dimension (3D) are inherently very complex and some way of assimilating this vast amount of information is needed (Mauro 1989; Goitein 1992). † Biological models enable estimates to be made of the effect of uncertainties in dose and patient position on therapy outcome (Boyer and Schultheiss 1988; Mijnheer et al. 1989; Mackay et al. 1999; Zavgorodni 2004). † The effect of non-uniformities in the tumour dose distribution can be approximately quantified (Brahme 1984; Sanchez-Nieto and Nahum 1999; Tome´ and Fowler 2000). † The values for α (especially important for tumours) and α/β from, for example, clonogenic assays can be both extracted from and fed into such models (Deacon et al. 1984; Peters et al. 1989; Mauro et al. 1989; West 1995; Bentzen 1997; Fenwick 1998; Sanchez-Nieto et al. 2001a; Buffa et al. 2001b; Levegrün et al. 2001, 2002; Wang et al. 2003a; Xiong et al. 2005; Carlone et al. 2006). † Estimates can be made of the effects on local tumour control of hypoxia and other information derived from functional imaging (Poppel et al. 2002; Nahum et al. 2003; Ruggieri 2004; Nioutsikou et al. 2005; Ruggieri and Nahum 2006). 1 49th AAPM Annual Meeting, Minneapolis, 22-26 July 2007 † The clinical effect of improvements in dose distributions through the use of new beam-delivery technology (e.g. MLCs, IMRT), 3D treatment planning systems, and new radiation modalities (brachytherapy, protons, light ions) can be approximately quantified (Webb 1993; Lee et al. 1994; Isacsson 1998; Gagliardi 1998, 2001; King et al. 2000; De Meerleer et al. 2000; Nahum and Glimelius 2001; Nutting et al. 2002). † Optimisation/inverse planning is beginning to be done in terms of biological criteria such as highest TCP for a fixed low value of NTCP, equivalent uniform dose (EUD) etc. (Källman 1992; Nahum and Tait 1992; Mohan et al. 1992; Brahme 1999, 2001; De Gersem et al. 1999; Engelsman et al. 2001; Iori 2001; Sanchez-Nieto et al. 2001a; Schwarz et al. 2003; Peñagarıcano et al. 2005; Kim and Tomé 2006; Hoffmann et al. 2006; Chen et al. 2007). † Models for TCP and NTCP can serve as an aid to clarity of thought about radiotherapy (Dutreix et al. 1988). Philosophy Radiobiology has ‘classically’ concerned itself with the properties of cell-survival curves. The linearquadratic model (e.g. Steel 2002, Chapman 2003) represents one of its triumphs in not only throwing a lot of light on the mechanisms of cell-killing by radiation, but in explaining so much of what was vaguely already known in an empirical sense, without much if any theoretical insight. Thus the principles of fractionation itself, the distinction between ‘early’ and ‘late’ reactions in terms of their dependence on the fractionation scheme, the calculation of iso-effective regimens with different fraction sizes (the Withers’ formula), the reduction in cell-killing at very low doserate and its implications for brachytherapy, all of these aspects and more are today immeasurably better understood as a result of the L-Q model. But knowing how many/what fraction of cells are killed by (uniform) doses, or how to change the fraction size safely, doesn’t get one nearly far enough in this age of Conformal Therapy. What Conformal Therapy also needs is a RADIOBIOLOGY of NORMAL TISSUES which applies to dose distributions and can tell us, therefore, what happens to the tolerance of an organ if we reduce the irradiated volume, or more precisely, change the dose distribution (and also, naturally, how fractionation and dose distributions are related). Normal tissues, organs-at-risk (OARs) or whatever one calls them, are as good as NEVER irradiated by uniform doses (even though tumours might be, though even here in the IMRT/stereotactic era this is less and less the case). Models, whether one calls them ‘biological’, ‘biophysical’, ‘biomathematical’ or anything else, which can quanitfy with reasonable certainty (and with quantifiable uncertainty/confidence limits) i) and ii) the probability of (local) tumour control - TCP the probability of a given type of complication is as a function of the dose distribution and fraction sizes - NTCP usher in the age of Conformal Radiobiology. NTCP models Underlying all NTCP models is the volume effect, which is central to how normal organs behave in response to inhomogeneous distributions of radiation and which therefore, has important implications for the design of treatment strategies. In organs with a small volume effect, it may be advantageous to use many fields in order to distribute the dose over a larger volume and thereby reduce the peak dose in the organ. Conversely, in parallel organs, it would be better to use a small number of fields to 2 49th AAPM Annual Meeting, Minneapolis, 22-26 July 2007 keep fractional damage below the organ’s functional reserve. Intensity modulation may prove useful in adjusting the volumetric distribution to normal organs while maintaining the intended dose to the large volume. In the future, we may find that organ architecture will play an important role in designing, in addition to evaluating treatment plans (Kutcher et al. 1994). In spite of their importance, NTCP values should be used with caution when evaluating treatment plans, since the models suffer from a number of problems (Glatstein 2001). To begin with, they are generally quite crude and hardly even try to represent the multiple and interrelated toxicities observed in clinical practice (Deasy et al. 2002). In this respect, modelling of NTCP is much more complex than TCP because of the large and complex taxonomy of treatment toxicities (Niemierko and Goitein 1993b; Withers and Taylor 1993; Glatstein 2001; Schultheiss 2001; Travis 2001; Yorke 2001; Deasy et al. 2002). And even when clinical responses are reduced to the barest essentials, perhaps to one or a few critical endpoints, the paucity of clinical data and their large uncertainties makes it difficult to rely on the calculated complication probabilities (Deasy et al. 2001; Glatstein 2001). These uncertainties can lead not only to large variations in the absolute values of the calculated NTCPs (Lebesque et al. 1995) but can also affect the relative ranking of candidate treatment plans. However, this situation is changing as subsequent lectures will make clear; the increased use of 3D planning by many institutions is beginning to provide large databases of three-dimensional dose distributions potentially correlated with clinical endpoints. Although the endpoints characterizing clinical complications, as is well known, are difficult to define and the data are painstaking to collect, there is nevertheless a continuing accumulation of such data. There are also indications that the pooling of clinical data and the ability to share dose distributions between institutions electronically will provide databases that are more robust where models can be refined (see the lecture by John Fenwick and also Kwa et al. 1998b; Deasy et al. 2003; Rancati et al. 2003; El Naqa et al. 2006). Some consensus may then be reached on the models and their parameters, at least for some important organs and endpoints, e.g. Seppenwoolde et al. (2003) in the case of radiation pneumonitis in lung and Rancati et al. (2004) in the case of proctitis in the rectum. As a complement to the lectures which follow by Ellen Yorke and Marco Schwarz, excellent summaries of the status of the NTCP models themselves and their application to a number of organs/endpoints can be found in Ten Haken (2001) and in Cattaneo et al. (2001). In the meantime, tools (such as BIOPLAN - Sanchez-Nieto and Nahum 2000 and that described in Warketin et al. 2004) are available which simplify the evaluation of the existing models (of both NTCP and TCP). The development of further NTCP models is probably unnecessary. However, the generation of more dose-volume-complication data for the organs and endpoints of most interest is essential in order to derive more reliable values of the parameters for the currently established models such as the L–K–B (see lectures by Ellen Yorke) and Relative Seriality (Källman et al 1992) formalisms. It is now imperative to start using the models and their associated parameters to make predictions of complications and to compare these predictions with the observed complication rates (e.g. Gagliardi et al. 2000). Only in this way will NTCP models come to be used with confidence in the clinic (see the lecture by Philip Mayles). Furthermore, for those organs/endpoints for which a reasonable amount of reliable dose-volume-complication data already exists (e.g. radiation pneumonitis in the lung; proctitis in the rectum; RILD in the liver), one can start optimizing treatment plans based on the calculated NTCP values. Two of the forms that this active use of NTCP modelling could take are 1. Start with a relative-dose treatment plan arrived at using, for example, dose-based criteria (e.g. PTV within 95–105% of Dpresc, V90% of OAR < 80% of Dpresc) and then adjust Dpresc until NTCPOAR is equal to a value specified in the local clinical protocol, e.g. NTCPproctitis = 3% (Nahum and Tait 1992; Ten Haken et al. 1993; McGinn et al. 1998; Sanchez-Nieto et al. 2001a). 2. Use NTCP and TCP as part of the objective function in the (computer) optimisation/inverseplanning process, thus allowing the mathematical and radiobiological properties of the models to drive the search for the optimum plan (e.g. Peñagarícano et al. 2005; Hoffmann et al. 2006). 3 49th AAPM Annual Meeting, Minneapolis, 22-26 July 2007 Furthermore, it should not be forgotten that other variables such as fraction size, clonogen proliferation rate and the patient’s performance status should ideally be incorporated into both the biological models and the optimisation process (Glatstein 2001; Bentzen 2004; Fowler et al. 2004; Nahum and Bentzen 2004). Low-dose hypersensitivity (LDHRS) may also play an important role in our understanding of how certain complications depend on dose and volume. One consequence of factoring LDHRS into NTCP models, via a modification of the L-Q expression below around 0.6 Gy, will be an increased contribution to overall NTCP from those volumes of normal tissue receiving doses well below the tumour dose, i.e. at the 20% and lower isodoses. A significant increase in such volumes through the use of rotational techniques such as tomotherapy or many-field IMRT may be undesirable for certain organs and endpoints in which the killing of cells exhibiting LDHRS play a significant role in causing the complication. The question of cancer induction by radiotherapy (see the lecture by Geoff Lawrence) should also be mentioned. Concerns have been raised (Glatstein 2002; Hall and Wuu 2003) that certain modern conformal techniques such as (many-field) IMRT, IMAT and tomotherapy may increase cancer induction due to the increase in volumes irradiated at low doses compared to non-IMRT few-field techniques and especially compared to the use of proton beams. Hitherto cancer induction has not been classed as a complication due to the presumed low or extremely low frequency of occurrence. Models of (second) cancer induction probability (SCIP) which take into account details of the dose distribution in different organs and also the patient’s age and general prognosis (Lindsay et al. 2001) would be desirable additions to the collection of tools for predicting the clinical effect of radiotherapy. Sachs and Brenner (2005) have produced a very useful analysis from which such SCIP models can now be developed. ACKNOWLEDGEMENTS I should like to acknowledge fruitful collaborations on radiobiological modelling with John Fenwick, Philip Mayles, Alison Scott, Zafar Malik, Chinnamani Eswar, Isabel Syndikus and John Littler at CCO and also Mauro Iori (Reggio Emilia), Giovanna Gagliardi (Stockholm), Beatriz Sanchez-Nieto (Santiago, Chile), Francesca Buffa (Gray lab, Northwood and Oxford, UK), Don Chapman (formerly Fox Chase Cancer Center, Philadelphia) and colleagues at RaySearch Laboratories AB (Stockholm). REFERENCES (essentially a comprehensive bibliography; not all of these are referred to in the text) Austin-Seymour, M. M., Chen, G. T. Y., Castro, J. R., Saunders, W. M., Pitluck, S., Woodruff, K. H., and Kessler, M., Dose volume histogram analysis of liver radiation tolerance, Int. J. Radiat. Oncol. Biol. Phys., 12, 31–35, 1986. Awwad H K (1990) Radiation Oncology: Radiobiological and Physiological Perspectives (Dordrecht: Kluwer Academic) especially chapters II.1, Dose-Survival Relationships, pp 19-52 and IV.7, Estimates of the Outcome of Radiotherapy pp 647-665 Batterman, J. J., Hart, A. A. M., and Breur, K., Dose-effect relations for tumour control and complication rate after fast neutron therapy for pelvic tumours, Br. J. Radiol., 54, 899–904, 1981. Benk, V. A., Adams, J. A., Shipley, W. U., Urie, M. M., McManus, P. L., Efird, J. T., Willett, J., and Goitein, M., Late rectal bleeding following combined x-rays and proton high dose irradiation for patients with stages T3–T4 prostate carcinoma, Int. J. Radiat. Oncol. Biol. Phys., 26, 551–557, 1993. 4 49th AAPM Annual Meeting, Minneapolis, 22-26 July 2007 Bentzen S M (1997) Potential clinical impact of normal-tissue intrinsic radiosensitivity testing Radioth. Oncol. 43 121-131. Bentzen, S. M., Dose-response relationships in radiotherapy, in Basic Clinical Radiobiology, Steel, G. G., Ed., 3rd ed., Arnold, London, pp. 94–104, 2002. Bentzen, S. M., High-tech in radiation oncology: Should there be a ceiling? Int. J. Radiat. Oncol. Biol. Phys., 58, 320–330, 2004. Bentzen, S. M. and Baumann, M., The L–Q model in clinical practice, in Basic Clinical Radiobiology, Steel, G. G., Ed., 3rd ed., Arnold, London, pp. 134–146, 2002. Bentzen, S. M., Thames, H. D., and Overgaard, J., Does variation in the in vitro cellular radiosensitivity explain the shallow clinical dose-control curve for malignant melanoma? Int. J. Radiat. Biol., 57, 117–126, 1990. Boersma, L. J., van den Brink, M., Bruce, A. M., Shouman, T., Gras, L., te Velde, A., and Lebesque, J. V., Estimation of the incidence of late bladder and rectum complications after high-dose (70–78 Gy) conformal radiotherapy for prostate cancer, using dose-volume histograms, Int. J. Radiat. Oncol. Biol. Phys., 41, 83–92, 1998. Boyer, A. L. and Schultheiss, T., Effects of dosimetric and clinical uncertainty on complication-free local tumor control, Radiother. Oncol., 11, 65–71, 1988. Brahme, A., Dosimetric precision requirements in radiation therapy, Acta Radiol. Oncol., 23, 379–391, 1984. Brahme, A., Optimized radiation therapy based on radiobiological objectives, Semin. Radiat. Oncol., 9, 35–47, 1999. Brahme, A., Individualizing cancer treatment: Biological optimisation models in treatment and planning, Int. J. Radiat. Oncol. Biol. Phys., 49, 327–337, 2001. Brahme, A. and A ° gren, A.-K., Optimal dose distribution for eradication of heterogeneous tumors, Acta Oncol., 26, 377–385, 1987. Brenner, D. J., Dose, volume and tumour-control predictions in radiotherapy, Int. J. Radiat. Oncol. Biol. Phys., 26, 171–179, 1993. Brenner, D. J. and Hall, E. J., Fractionation and protraction for radiotherapy of prostate carcinoma, Int. J. Radiat. Oncol. Biol. Phys., 43, 1095–1101, 1999. Buffa, F. M. and Nahum, A. E., Monte-Carlo dose calculations and radiobiological modelling: Analysis of the effect of the statistical noise of the dose distribution on the probability of tumour control, Phys. Med. Biol., 45, 3009–3023, 2000. Buffa, F. M., Fenwick, J. D., and Nahum, A. E., Letter to the editor: A realistic closed-form radiobiological model of clinical tumor-control data incorporating inter-tumor heterogeneity by Roberts and Hendry, Int. J. Radiat. Onc. Biol. Phys., 41, 689–699, 1999. Buffa, F. M., Fenwick, J. D., and Nahum, A. E., An analysis of the relationship between radiosensitivity and volume effects in tumour control probability modelling, Med. Phys., 27, 1258–1265, 2000. Buffa, F. M., West, C., Byrne, K., and Nahum, A. E., Radiation response and cure rate of human colon adenocarcinoma spheroids of different size: The significance of hypoxia on tumour control modelling, Int. J. Radiat. Onc. Biol. Phys., 49, 1109–1118, 2001a. Buffa, F. M., Davidson, S. E., Hunter, R. D., Nahum, A. E., and West, C. M. L., Incorporating biological measurements (SF2, CFE) in a tumor control probability model increases their prognostic significance: A study in cervical carcinoma treated with radiation therapy, Int. J. Radiat. Onc. Biol. Phys., 50, 1113–1122, 2001b. Burman, C., Kutcher, G. J., Emami, B., and Goitein, M., Fitting normal tissue tolerance data to an analytic function, Int. J. Radiat. Oncol. Biol. Phys., 21, 123–135, 1991. 5 49th AAPM Annual Meeting, Minneapolis, 22-26 July 2007 Carlone, M. C., Warkentin, B., and Stavrev, P., Fundamental form of a population TCP model in the limit of large heterogeneity, Med. Phys., 33, 1634–1642, 2006. Cattaneo, G. M., Gagliardi, G., Nahum, A. E., Eds., The practical use of TCP and NTCP models for the evaluation of treatment plans in radiotherapy. Physica Medica 17 (Suppl. 2), 2001. Chapman, J. D., Invited review: The single-hit mechanism of tumor cell killing by radiation, Int. J. Radiat. Biol., 79, 71-81, 2003 Chen, G. T. Y., Dose volume histograms in treatment planning, Int. J. Radiat. Oncol. Biol. Phys., 14, 1319–1320, 1988. Chen, G-P., Ahunbay, E., Schulz, C., and Li, X. Allen, Development of an inverse optimization package to plan nonuniform dose distributions based on spatially inhomogeneous radiosensitivity extracted from biological images, Med. Phys.., 34, 1198-1205, 2007. Cheng, C. W. and Das, I. J., Treatment plan evaluation using dose-volume histogram (DVH) and spatial dosevolume histogram (zDVH), Int. J. Radiat. Oncol. Biol. Phys., 43, 1143–1150, 1999. Dale, R. G., The application of the linear-quadratic dose-effect equation to fractionated and protracted radiotherapy, Br. J. Radiol., 58, 515–528, 1985. Dale, E., Olsen, D. R., and Fossa°, S. D., Normal tissue complication probabilities correlated with late effects in the rectum after prostate conformal radiotherapy, Int. J. Radiat. Oncol. Biol. Phys., 43, 385–391, 1999. Dasu, A. and Denekamp, J., New insights into factors influencing the clinically relevant oxygen enhancement ratio, Radiother. Oncol., 46, 269–277, 1998. Dawson, L. A., Ten Haken, R. K., and Lawrence, T. S., Partial irradiation of the liver, Semin. Radiat. Oncol., 11, 240–246, 2001. Dawson, L. A., Normolle, D., Balter, J. M., McGinn, C. J., Lawrence, T. S. et al., Analysis of radiation-induced liver disease using the Lyman NTCP model, Int. J. Radiat. Oncol. Biol. Phys., 53, 810–821, 2002. De Gersem, W. R. T., Derycke, S., Colle, C. O., de Wagter, C., and de Neve, W. J., Inhomogeneous target-dose distributions: A dimension more for optimization? Int. J. Radiat. Oncol. Biol. Phys., 44, 461–468, 1999. De Jaeger, K., Hoogeman, M. S., Engelsman, M., Seppenwoolde, Y., Damen, E. M. F. et al., Incorporating animproved dose-calculation algorithm in conformal radiotherapy of lung cancer: Re-evaluation of dose in normal lung tissue, Radiother. Oncol., 69, 1–10, 2003. Deacon, J., Peckham, M. J., and Steel, G. G., The radioresponsiveness of human tumours and the initial slope of the cell-survival curve, Radiother. Oncol., 2, 317–323, 1984. Dearnaley, D. D., Khoo, V. S., Norman, A., Meyer, L., Nahum, A. et al., Reduction of radiation proctitis by conformal radiotherapy techniques in prostate cancer: A randomized trial, Lancet, 353, 267–272, 1999. Deasy, J., Poisson formulas for tumor control probability with clonogen proliferation, Radiat. Res., 145, 382– 384,1996. Deasy, J. O., Niemierko, A., Herbert, D., Yan, D., Jackson, A., Ten Haken, R. K., Langer, M., and Sapareto, S., Methodological issues in radiation dose-volume outcome analyses: Summary of a joint AAPM/NIH workshop, Med. Phys., 29, 2109–2127, 2002. Deasy, J. O., Blanco, A. I., and Clark, V. H., CERR: A computational environment for radiotherapy research, Med. Phys., 30, 979–985, 2003. Dutreix, J., Tubiana, M., and Dutreix, A., An approach to the interpretation of clinical data on the tumour control robability-dose relationship, Radiother. Oncol., 11, 239–248, 1988. Ebert, M. A., Viability of the EUD and TCP concepts as reliable dose indicators, Phys. Med. Biol., 45, 441–457, 2000. 6 49th AAPM Annual Meeting, Minneapolis, 22-26 July 2007 Eisbruch, A., Ship, J. A., Kim, H. M., and Ten Haken, R. K., Partial irradiation of the parotid gland, Semin. Radiat. Oncol., 11, 234–239, 2001. El Naqa, I., Suneja, G., Lindsay, P. E., Hope, A. J., Alaly, J. R., Vicic, M., Bradley, J. D., Apte, A., and Deasy, J. O., Dose response explorer: an integrated open-source tool for exploring and modelling radiotherapy dosevolume outcome relationships, Phys. Med. Biol., 51, 5719–5735, 2006. Emami, B., Lyman, J., Brown, A., Coia, L., Goitein, M. et al., Tolerance of normal tissue to therapeutic irradiation, Int. J. Radiat. Oncol. Biol. Phys., 21, 109–122, 1991a. Engelsman, M., Remeijer, P., van Herk, M., Lebesque, J. V., Mijnheer, B., and Damen, E. M. F., Field size reduction enables Iso-NTCP escalation of tumor control probability for irradiation of lung tumours, Int. J. Radiat. Oncol. Biol. Phys., 51, 1290–1298, 2001. Fay, M., Tan, A., Fisher, R., Wirth, A., and Ball, D., Dose-volume histogram analysis as predictor of radiation pneumonitis in primary lung cancer patients treated with radiotherapy, Int. J. Radiat. Oncol. Biol. Phys., 61, 1355–1363, 2005. Fenwick, J. D., Predicting the radiation control probability of heterogeneous tumour ensembles: Data analysis and parameter estimation using a closed-form expression, Phys. Med. Biol., 43, 2159–2178, 1998. Fenwick, J. D., Biological modelling of pelvic radiotherapy: Potential gains from conformal techniques, PhD thesis, University of London, U.K., Available as internal report ICR/CCO/2000/1 from the author, Physics dept., Clatterbridge Centre for Oncology, Bebington CH63 4JY U.K., 1999. Fenwick, J. D., Khoo, V. S., Nahum, A. E., Sanchez-Nieto, B., and Dearnaley, D. P., Correlations between dosesurface histograms and the incidence of long-term rectal bleeding following conformal or conventional radiotherapy treatment of prostate cancer, Int. J. Radiat. Oncol. Biol. Phys., 49, 473–480, 2001. Fiorino, C., Cozzarini, C., Vavassori, V., Sanguineti, G., Bianchi, C. et al., Relationships between DVHs and late rectal bleeding after radiotherapy for prostate cancer: Analysis of a large group of patients pooled from three institutions, Radiother. Oncol., 64, 1–12, 2002a. Fiorino, C., Vavassori, V., Sanguineti, G., Bianchi, C., Cattaneo, G. M., Piazzolla, A., and Cozzarini, C., Rectum contouring variability in patients treated for prostate cancer: Impact on rectum dose-volume histograms and normal tissue complication probability, Radiother. Oncol., 63, 249–255, 2002b. Fiorino, C., Gianolini, S., and Nahum, A. E., A cylindrical model of the rectum: Comparing dose-volume, dosesurface and dose-wall histograms in the radiotherapy of prostate cancer, Phys. Med. Biol., 48, 2603–2616, 2003. Fischer, J. J. and Moulder, J. E., The steepness of the dose-response curve in radiation injury, Radiology, 117, 179–184, 1975. Fowler, J. F., The linear quadratic formula and progress in fractionated radiotherapy, Br. J. Radiol., 62, 679–694, 1989. Fowler, J. F., Normal tissue complication probabilities: How well do the models work? Physica Medica, 17(Suppl. 2), 24–35, 2001. Fowler, J. F., Chappell, R., and Ritter, M., Is α/β for prostate cancer really low? Int. J. Radiat. Oncol. Biol. Phys., 50, 1021–1031, 2001. Fowler, J. F., Tome´,W. A., Fenwick, J. D., and Mehta, M., A challenge to traditional radiation oncology, Int. J. Radiat. Oncol. Biol. Phys., 60, 1241-1256, 2004. Gagliardi, G., Modeling heart and lung complication data in radiotherapy of the breast, PhD thesis, Stockholm University, 1998. Gagliardi, G., Lax, I., Ottolenghi, A., and Rutqvist, L. E., Long-term cardiac mortality after radiotherapy of breast cancer—application of the relative seriality model, Br. J. Radiol., 69, 839–846, 1996. 7 49th AAPM Annual Meeting, Minneapolis, 22-26 July 2007 Gagliardi, G., Bjöhle, J., Lax, I., Ottolenghi, A., Eriksson, F. et al., Radiation pneumonitis after breast cancer irradiation: Analysis of the complication probability using the relative seriality model, Int. J. Radiat. Oncol. Biol. Phys.,46, 373–381, 2000. Gagliardi, G., Lax, I., and Rutqvist, L. E., Partial irradiation of the heart, Semin. Radiat. Oncol., 11, 224–239, 2001. Glatstein, E., Lichter, A. S., Fraass, B. A., and van de Geijn, J., The imaging revolution and radiation oncology: Use of CT, ultrasound and NMR for the localisation, treatment planning and treatment delivery, Int. J. Radiat. Oncol. Biol. Phys., 11, 1299–1311, 1985. Glatstein, E., Personal thoughts on normal tissue tolerance, or, what the textbooks don’t tell you, Int. J. Radiat. Oncol. Biol. Phys., 51, 1185–1189, 2001. Glatstein, E., Intensity-modulated radiation therapy: The inverse, the converse, and the perverse, Semin. Radiat. Oncol., 12, 272–281, 2002. Goitein, M., The utility of computed tomography in radiation therapy: An estimate of outcome, Int. J. Radiat. Oncol. Biol. Phys., 5, 1799–1807, 1979. Goitein, M., Causes and consequences of inhomogeneous dose distributions in radiation therapy, Int. J. Radiat. Oncol. Biol. Phys., 12, 701–704, 1986. Goitein, M. and Niemierko, A., Intensity modulated therapy and inhomogeneous dose to the tumour: A note of caution, Int. J. Radiat. Oncol. Biol. Phys., 36, 519–522, 1996. Graham, M. V., Purdy, J. A., Emami, B., Harms, W., Bosch, W., Lockett, M. A., and Perez, C. A., Clinical dosevolume-histogram analysis for pneumonitis after 3D treatment for non-small cell lung cancer (NSCLC), Int. J. Radiat. Oncol. Biol. Phys., 45, 323–329, 1999. Hall, E. J. and Wuu, C. S., Radiation-induced second cancers: The impact of 3D-CRT and IMRT, Int. J. Radiat. Oncol. Biol. Phys., 56, 83–88, 2003. Hanks, G., Martz, K. L., and Diamond, J. J., The effect of dose on local control of prostate cancer, Int. J. Radiat. Oncol. Biol. Phys., 15, 1299–1305, 1988. Hanks, G. E., Schultheiss, T. E., Hanlon, A. L., Hunt, M., and Lee, W. R., Optimization of conformal radiation treatment of prostate cancer: Report of a dose escalation study, Int. J. Radiat. Oncol. Biol. Phys., 37, 543–550, 1997. Hartford, A. C., Niemierko, A., Adams, J. A., Urie, M. M., and Shipley, W. U., Conformal irradiation of the prostate: Estimating long-term rectal bleeding risk using dose-volume histograms, Int. J. Radiat. Oncol. Biol. Phys., 36, 721–730, 1996. Hoffmann, A. L., Siem, A. Y., den Hertog, D., Kaanders, J. H., and Huizenga, H., Derivative-free generation and interpolation of convex Pareto optimal IMRT plans, Phys. Med. Biol., 51, 6349–6369, 2006. Hoogeman, M. S., van Herk, M., de Bois, J., Muller-Timmermans, P., Koper, P. C. M. et al., Quantification of local rectal wall displacements by virtual rectum unfolding, Radiother. Oncol., 70, 21–30, 2004. Isacsson, U., Comparative treatment planning in external radiotherapy of malignant tumours, PhD thesis, Department of Oncology, Uppsala University, 1998. Jackson, A., Kutcher, G. J., and Yorke, E. D., Probability of radiation induced complications for normal tissues with parallel architecture subject to non-uniform irradiation, Med. Phys., 20, 613–625, 1993. Jackson, A., Ten Haken, R. K., Robertson, J. M., Kessler, M. L., Kutcher, G. J., and Lawrence, T. S., Analysis of clinical complication data for radiation hepatitis using a parallel architecture model, Int. J. Radiat. Oncol. Biol. Phys., 31, 883–891, 1995. Jackson, A., Skwarchuk, M. W., Zelefsky, M. J., Cowen, D. M., Venkatraman, E. S. et al., Late rectal bleeding after conformal radiotherapy of prostate cancer. II. Volume effects and dose-volume histograms, Int. J. Radiat. Oncol.Biol. Phys., 49, 685–698, 2001. 8 49th AAPM Annual Meeting, Minneapolis, 22-26 July 2007 Källman, P., Optimization of radiation therapy planning using physical and biological objective functions, PhD thesis, Department of Radiation Physics, Stockholm University, 1992. Källman, P., Ågren, A., and Brahme, A., Tumour and normal tissue responses to fractionated non-uniform dose delivery, Int. J. Radiat. Biol., 62, 249–262, 1992. Kaplan, E. L. and Meier, P., Nonparametric estimation from incomplete observations, J. Am. Stat. Assoc., 53, 457–816, 1958. Keall, P. J., Siebers, J. V., Jeraj, R., and Mohan, R., The effect of dose calculation uncertainty on the evaluation of radiotherapy plans, Med. Phys., 27, 478–484, 2000. Keall, P. J., Lammering, G., Lin, P.-S., Winter, D., Chung, T. D. et al., Tumor control probability predictions for genetic radiotherapy, Int. J. Radiat. Oncol. Biol. Phys., 57, 255–263, 2003. Kessler, M. L., Pitluck, S., Petti, P., and Castro, J. R., Integration of multimodality imaging data for radiotherapy treatment planning, Int. J. Radiat. Oncol. Biol. Phys., 21, 1653–1667, 1991. Kim, Y. and Tome´, W., Risk-adaptive optimization: selective boosting of high-risk tumor subvolumes, Int. J. Radiat. Oncol. Biol. Phys., 66, 1528–1542, 2006. King, C. R., DiPetrillo, T. A., and Wazer, D. E., Optimal radiotherapy for prostate cancer: Predictions for conventional external beam, IMRT, and brachytherapy from radiobiologic models, Int. J. Radiat. Oncol. Biol. Phys., 46, 165–172, 2000. Kutcher, G. J. and Burman, C., Calculation of complication probability factors for non uniform normal tissue irradiation: The effective volume method, Int. J. Radiat. Oncol. Biol. Phys., 16, 1623–1630, 1989. Kutcher, G. J., Burman, C., Brewster, L., Goitein, M., and Mohan, R., Histogram reduction method for calculating complication probabilities for three-dimensional treatment planning evaluations, Int. J. Radiat. Oncol. Biol. Phys., 21, 137–146, 1991. Kutcher, G. J., Niehaus, A., and Yorke, E. D., The effect of normal organ architecture on 3D conformal strategies, in XIth International Conference on The Use of Computers in Radiotherapy, Manchester, Hounsell, A. R.,Wilkinson, J. M., and Williams, P. C., Eds., Medical Physics Publishing, Madison, WI, pp. 10–11, 1994. Kutcher, G. J., Leibel, S. A., Ling, C. C., Zelefsky, M., and Fuks, Z., New wine in an old bottle? Dose escalation under dose-volume constraints: A model of conformal therpay of the prostate, Int. J. Radiat. Oncol. Biol. Phys., 35, 415–416, 1996. Kwa, S. L. S., Theuws, J. C. M., Wagenaar, A., Damen, E. M. F., Boersma, L. J., Baas, P., Muller, S. H., and Lebesque, J. V., Evaluation of two dose-volume histogram reduction models for the prediction of radiation pneumonitis, Radiother. Oncol., 48, 33–44, 1998a. Kwa, S. L. S., Lebesque, J. V., Theuws, J. C. M., Marks, L. B., Munley, M. T. et al., Radiation pneumonitis as a function of mean lung dose: An analysis of pooled data of 540 patients, Int. J. Radiat. Oncol. Biol. Phys., 42, 1– 9, 1998b. Laing, R. W., Bentley, R. E., Nahum, A. E., Warrington, A. P., and Brada, M., Stereotactic radiotherapy of irregular targets: A comparison between static conformal beams and non-coplanar arcs, Radiother. Oncol., 28, 241–246, 1993. Lawrence, T. S., Tesser, R. J., and Ten Haken, R. K., An application of dose volume histograms to the treatment of intrahepatic malignancies with radiation therapy, Int. J. Radiat. Oncol. Biol. Phys., 19, 1041–1047, 1990. Lawrence, T. S., Ten Haken, R. K., Kessler, M. L., Robertson, J. M., Lyman, J. T. et al., The use of 3-D dose volume analysis to predict radiation hepatitis, Int. J. Radiat. Oncol. Biol. Phys., 23, 781–788, 1992. Lebesque, J. V., Bruce, A., Kroes, G., Shouman, T., and van Herk, M., Variation in volumes, dose-volume histograms and estimated normal tissue complication probabilities of rectum and bladder during conformal radiotherapy of T3 prostate cancer, Int. J. Radiat. Oncol. Biol. Phys., 33, 251–257, 1995. 9 49th AAPM Annual Meeting, Minneapolis, 22-26 July 2007 Lee, M., Wynne, C., Webb, S., Nahum, A. E., and Dearnaley, D., A comparison of proton and megavoltage xraytreatment planning for prostate cancer, Radiother. Oncol., 33, 239–253, 1994. Levegrün, S., Jackson, A., Zelefsky, M. J., Skwarchuk, M. W., Venkatraman, E. S., Schlegel, W. et al., Analysis of biopsy outcome after three-dimensional conformal radiation therapy of prostate cancer using dose-distribution variables and tumor control probability models, Int. J. Radiat. Oncol. Biol. Phys., 47, 1245–1260, 2000. Levegrün, S., Jackson, A., Zelefsky, M. J., Skwarchuk, M. W., Venkatraman, E. S., Schlegel, W. et al., Fitting tumor control probability models to biopsy outcome after three-dimensional conformal radiation therapy of prostate cancer: pitfalls in deducing radiobiologic parameters for tumors from clinical data, Int. J. Radiat. Oncol. Biol. Phys.,51, 1064–1080, 2001. Li, S., Boyer, A., Lu, Y., and Chen, G. T., Analysis of the dose-surface histogram and dose-wall histogram for the rectum and bladder, Med. Phys., 24, 1107–1116, 1997. Liao, Z. X., Travis, E. L., and Tucker, S. L., Damage and morbidity from pneumonitis after irradiation of partial volumes of mouse lung, Int. J. Radiat. Oncol. Biol. Phys., 32, 1359–1370, 1995. Lindsay, K. A., Wheldon, E. G., Deehan, C., and Wheldon, T. E., Radiation carcinogenesis modelling for risk of treatment-related second tumours following radiotherapy, Br. J. Radiol., 74, 529–536, 2001. Lindsay, P. E., Moiseenko, V. V., van Dyk, J., and Battista, J. J., The influence of brachytherapy dose heterogeneity on estimates of α/β for prostate cancer, Phys. Med. Biol., 48, 507–522, 2003. Lu, Y., Li, S., Spelbring, D., Song, P., Vijayakumar, S. et al., Dose-surface histograms as treatment planning tool for prostate conformal therapy, Med. Phys., 22, 279–284, 1995. Lyman, J. T., Complication probabilities as assessed from dose-volume histograms, Radiat. Res., 104, S13– S19, 1985. Lyman, J. T. and Wolbarst, A. B., Optimization of radiation therapy. III. A method for assessing complication probabilities from dose-volume histograms, Int. J. Radiat. Oncol. Biol. Phys., 13, 103–109, 1987. Lyman, J. T. and Wolbarst, A. B., Optimization of radiation therapy. IV. A dose volume reduction algorithm, Int. J. Radiat. Oncol. Biol. Phys., 17, 433–436, 1989. Mackay, R. I., Hendry, J. H., Moore, C. J., Williams, P. C., and Read, G., Predicting late rectal complications following prostate conformal radiotherapy using biologically effective doses and normalized dose-surface histograms, Br. J. Radiol., 70, 517–526, 1997. Mackay, R. I., Graham, P. A., Moore, C. J., Logue, J. P., and Sharrock, P. J., Animation and radiobiological analysis of 3D motion in conformal radiotherapy, Radiother. Oncol., 52, 43–49, 1999. Marks, L. B., The pulmonary effects of thoracic irradiation, Oncology, 8, 89–100, 1994. Martel, M. K., Ten Haken, R. K., Hazuka, M. B., Turrisi, A. T., Frass, B. A., and Lichter, A. S., Dose-volume histogram and 3-D treatment planning evaluation of patients with pneumonitis, Int. J. Radiat. Oncol. Biol. Phys., 28, 575–581, 1994. Martel, M. K., Ten Haken, R. K., Hazuka, M. B., Kessler, M. L., Strawderman, M. et al., Estimation of tumor control probability parameters from 3-D dose distributions of non-small cell lung cancer patients, Lung Cancer, 24, 31–37, 1999. Mauro, F., Arcangeli, G., D’Angelo, L., Marino, C., and Benassi, M., Mathematical models of cell survival after ionising radiation: Application to radiotherapy planning, Health Phys., 57, 355–361, 1989. Mayles P, Nahum A and Rosenwald J-C, Handbook of Radiotherapy Physics Theory and Practice, Taylor & Francis (New York and London), 2007; ISBN 0-7503-0860-5 Mavroidis, P., Lind, B. K., Theodorou, K., Laurell, G., Fernberg, J. O., Lefkopoulos, D., Kappas, C., and Brahme, A., Statistical methods for clinical verification of dose-response parameters related to esophageal stricture and AVM obliteration from radiotherapy, Phys. Med. Biol., 49, 3797–3816, 2004. 10 49th AAPM Annual Meeting, Minneapolis, 22-26 July 2007 McGinn, C. J., Ten Haken, R. K., Ensminger, W. D., Walker, S., Wang, S. et al., Treatment of intrahepatic cancers with radiation doses based on a normal tissue complication probability model, J. Clin. Oncol., 16, 2246– 2252, 1998. Mohan, R., Mageras, G. S., Baldwin, B., Brewster, L. J., and Kutcher, G. J., Clinically relevant optimization of 3D conformal treatments, Med. Phys., 19, 933–944, 1992. Mohiuddin, M., Fujita, M., Regine, W. F., Megooni, A. S., Ibbott, G. S., and Ahmed, M. M., High-dose spatiallyfractionated radiation (GRID): a new paradigm in the management of advanced cancers, Int. J. Radiat. Oncol. Biol. Phys., 45, 721–727, 1999. Moore, J. V., Hendry, J. H., and Hunter, R. D., Dose incidence curves for tumor control and normal tissue injury in relation to the response of clonogenic cells, Radiother. Oncol., 1, 143–157, 1983. Morrison, R., The results of treatment of cancer of the bladder—a clinical contribution to radiobiology, Clin. Radiol., 26, 67–75, 1975. Mothersill, C. E., Moriarty, M. J., and Seymour, C. B., Radiotherapy and the exploitation of bystander effects, Int. J. Radiat. Oncol. Biol. Phys., 58, 575–579, 2004. Movsas, B., Chapman, J. D., Greenberg, R. E., Hanlon, A. L., Horwitz, E. M. et al., Increasing levels of hypoxia in human prostate carcinoma correlate significantly with increasing clinical stage and age: An Eppendorf pO2 study, Cancer, 89, 2018–2024, 2000. Movsas, B., Chapman, J. D., Hanlon, A. L., Horwitz, E. M., Greenberg, R. E. et al., A hypoxic ratio of prostate pO2/muscle pO2 predicts for biochemical failure in prostate cancer patients, J. Urol., 60, 634–639, 2002. Munro, T. R. and Gilbert, C. W., The relationship between tumour lethal doses and the radiosensitivity of tumour cells, Br. J. Radiol., 34, 246–251, 1961. Nahum, A.E., Converting dose distributions into tumour control probability, in IAEA-TECDOC-896, Radiation Dose in Radiotherapy from Prescription to Delivery: Proceedings of a Seminar Held in Rio de Janeiro, Brazil, 27–30 August 1994, IAEA, Vienna, pp. 27–40, 1996. Nahum, A. E. and Bentzen, S. M., IMRT and hypofractionation: A double therapeutic gain if used with care, Radiother. Oncol., 73(Suppl. 1), S174, 2004. Nahum, A. E. and Chapman, J. D., Correspondence: In response to Dr. Colin Orton, Int. J. Radiat. Onc. Biol. Phys., 58, 1637–1639, 2004. Nahum, A. E. and Glimelius, B., Biological models applied to the comparison of proton and photon treatments, Physica Medica, 17(Suppl. 2), 126–130, 2001. Nahum, A. E. and Sanchez-Nieto, B., Tumour control probability modelling: Basic principles and applications in treatment planning, Physica Medica, 17(Suppl. 2), 13–23, 2001. Nahum, A. E. and Tait, D. M., in Maximising Local Control by Customised Dose Prescription for Pelvic Tumours Advanced Radiation Therapy: Tumour Response Monitoring and Treatment Planning, Breit, A., Ed., Springer, Heidelberg, pp. 425–431, 1992. Nahum, A. E., Movsas, B., Horwitz, E. M., Stobbe, C. C., and Chapman, J. D., Incorporating clinical measurements of hypoxia into tumor local control modeling of prostate cancer: Implications for the α/β ratio, Int. J. Radiat. Oncol. Biol. Phys., 57, 391–401, 2003a. Nahum, A. E., Polico, R., Iori, M., Iotti, C., Paiusco, M. et al., Adapting the LQ expression for surviving fraction to organ-at-risk dose distributions: Why large fractions may make sense for parallel OARs, Radiother. Oncol., 68, S113, 2003b. Niemierko, A., Reporting and analysing dose distributions: A concept of equivalent uniform dose, Med. Phys., 24, 103–110, 1997. Niemierko, A., A generalized concept of equivalent uniform dose (EUD), Med. Phys., 26, 1100, 1999a. 11 49th AAPM Annual Meeting, Minneapolis, 22-26 July 2007 Niemierko, A., A unified model of tissue response to radiation, Med. Phys., 26, 1100, 1999b. Niemierko, A. and Goitein, M., Random sampling for evaluating treatment plans, Med. Phys., 17, 753–762, 1990. Niemierko, A. and Goitein, M., Calculation of normal tissue complication probability and dose-volume histogram reduction schemes for tissues with critical element architecture, Int. J. Radiat. Oncol. Biol. Phys., 25, 135–145, 1991. Niemierko, A. and Goitein, M., Implementation of a model for estimating tumor control probability for an inhomogeneously irradiated tumour, Radiother. Oncol., 29, 140–147, 1993a. Niemierko, A. and Goitein, M., Modeling of normal tissue response to radiation: The critical volume model, Int. J. Radiat. Oncol. Biol. Phys., 25, 135–145, 1993b. Niemierko, A. and Goitein, M., Dose-volume distributions: A new approach to dose-volume histograms in threedimensional treatment planning, Med. Phys., 21, 3–11, 1994. Nioutsikou, E., Partridge, M., Bedford, J. L., and Webb, S., Prediction of radiation-induced normal tissue complications in radiotherapy using functional image data, Phys. Med. Biol., 50, 1035–1046, 2005. Nutting, C. M., Corbishley, C. M., Sanchez-Nieto, B., Cosgrove, V. P., Webb, S. et al., Potential improvements in the therapeutic ratio of prostate cancer irradiation: Dose escalation of pathologically identified tumour nodules using intensity modulated radiotherapy, Br. J. Radiol., 75, 151–161, 2002. Padhani, A. R., Khoo, V.S, Suckling, J., Husband, J. E., Leach, M. O. et al., Evaluating the effect of rectal distension and movement on prostate gland position using cine MRI, Int. J. Radiat. Oncol. Biol. Phys., 44, 525– 533, 1999. Peñagarícano, J. A., Papanikolaou, N., Wu, C., and Yan, Y., An assessment of biologically-based optimisation (BORT) in the IMRT era, Med. Dosim., 30, 12–19, 2005. Peters, L. J., Brock, W. A., Chapman, J. D., Wilson, G., and Fowler, J. F., Response predictors in radiotherapy: A review of research into radiobiologically based assays, Br. J. Radiol., Suppl. 22 69–108, 1989. Poppel, R. A., Ove, R., and Shen, S., Tumor control probability for selective boosting of hypoxic subvolumes, including the effect of reoxygenation, Int. J. Radiat. Oncol. Biol. Phys., 54, 921–927, 2002. Porter, E. H., The statistics of dose/cure relationships for irradiated tumours Part II, Br. J. Radiol., 53, 336–345, 1980. Rancati, T., Ceresoli, G., Gagliardi, G., Schipani, S., and Cattaneo, G. M., Factors predicting radiation pneumonitis in lung cancer patients: A retrospective study, Radiother. Oncol., 67, 275–283, 2003. Rancati, T., Fiorino, C., Gagliardi, G., Cattaneo, G. M., Sanguineti, G. et al., Fitting late rectal bleeding data using different NTCP models: Results from an Italian multi-centric study (AIROPROS0101), Radiother. Oncol., 73, 21–32, 2004. Rowbottom, C. G., Oldham, M., and Webb, S., Constrained customization of non-coplanar beam orientations in radiotherapy of brain tumours, Phys. Med. Biol., 44, 383–399, 1999a. Rowbottom, C. G., Oldham, M., and Webb, S., Is it possible to optimize a radiotherapy treatment plan? Int. J. Oncol. Biol. Phys., 43, 698–699, 1999b. Ruggieri, R., Hypofractionation in non-small cell lung cancer (NSCLC); suggestions from modelling both acute and chronic hypoxia, Phys. Med. Biol., 49, 4811–4823, 2004. Ruggieri, R. and Nahum, A. E., The impact of hypofractionation on simultaneous dose-boosting to hypoxic tumor subvolumes, Med. Phys., 33, 4044–4055, 2006. Sachs, R. K. and Brenner, D. J., Solid tumor risks after high doses of ionizing radiation, Proc. Natl. Acad. Sci. U.S.A., 102, 13040–13045, 2005. 12 49th AAPM Annual Meeting, Minneapolis, 22-26 July 2007 Sanchez-Nieto, B. and Nahum, A. E., The Delta-TCP concept: A clinically useful measure of tumour control probability, Int. J. Radiat. Oncol. Biol. Phys., 44, 369–380, 1999. Sanchez-Nieto, B. and Nahum, A. E., BIOPLAN: Software for the biological evaluation of radiotherapy treatment plans, Med. Dosim., 25, 71–76, 2000. Sanchez-Nieto, B., Nahum, A. E., and Dearnaley, D. P., Individualisation of dose prescription based on normaltissue dose-volume and radiosensitivity data, Int. J. Radiat. Ther. Biol., Phys., 49, 487–499, 2001a. Sanchez-Nieto, B., Fenwick, J. F., Nahum, A. E., and Dearnaley, D. P., Biological dose surface maps: Evaluation of 3D dose data for tubular organs, Radiother. Oncol., 61, S52, 2001b. Schultheiss, T. E., Orton, C. G., and Peck, R. A., Models in radiation therapy: Volume effects, Med. Phys., 10, 410–415, 1983. Schultheiss, T. E., Hanks, G. E., Hunt, M. A., and Lee, W. R., Incidence of and factors related to late complications in conformal and conventional radiation treatment of cancer of the prostate, Int. J. Radiat. Oncol. Biol. Phys., 32, 643–649, 1995. Schwarz, M., Lebesque, J. V., Mijnheer, B. J., and Damen, E. M. F., Sensitivity of treatment plan optimisation for prostate cancer using the equivalent uniform dose (EUD) with respect to the rectal wall volume parameter, Radiother. Oncol., 73, 209–218, 2003. Seppenwoolde, Y. and Lebesque, J. V., Partial irradiation of the lung, Semin. Radiat. Oncol., 11, 247–258, 2001. Seppenwoolde, Y., Lebesque, J. V., de Jaeger, K., Belderbos, J. S. A., Boersma, L. J. et al., Comparing different NTCP models that predict the incidence of radiation pneumonitis, Int. J. Radiat. Oncol. Biol. Phys., 55, 724–735, 2003. Seppenwoolde, Y., de Jaeger, K., Boersma, L. J., Belderbos, J. S. A., and Lebesque, J. V., Regional differences in lung radiosensitivity after radiotherapy for non-small-cell lung cancer, Int. J. Radiat. Oncol. Biol. Phys., 60, 748–758, 2004. Steel, G. G., Ed., Basic Clinical Radiobiology, 3rd ed., Edward Arnold, London, 2002. Steel, G. G. and Peacock, J. H., Why are some human tumours more radiosensitive than others?, Radiother. Oncol., 15, 63–72, 1989. Stewart, J. G. and Jackson, A. W., The steepness of the dose response curve both for tumor cure and normal tissue injury, Laryngoscope, 85, 1107–1111, 1975. Stock, R. G., Stone, N. N., Tabert, A., Iannuzzi, C., and DeWyngaert, J. K., A dose-response study for I-125 prostate implants, Int. J. Radiat. Oncol. Biol. Phys., 41, 101–108, 1998. Suchowerska, N., Ebert, M. A., Zhang, M., and Jackson, M., In vitro response of tumour cells to non-uniform irradiation, Phys. Med. Biol., 50, 3041–3051, 2005. Suit, H., Skates, S., Taghian, A., Okunieff, P., and Efird, J. T., Clinical implications of heterogeneity of tumor response to radiation therapy, Radiother. Oncol., 25, 251–260, 1992. Tait, D. M., Nahum, A. E., Meyer, L., Law, M., Dearnaley, D. P., Horwich, A., Mayles, W. P., and Yarnold, J. R., Acute toxicity in pelvic radiotherapy: A randomized trial of conformal versus conventional treatment, Radiother. Oncol., 42, 121–136, 1997. Ten Haken, R.K., Ed., Partial organ irradiation, Semin. Radiat. Oncol., 11, 181–267, 2001. Ten Haken, R. K., Forman, J. D., Heimburger, D. K., Gerhardsson, A., McShan, D. L., and Perez-Tomayo, C., Treatment planning issues related to prostate movement in response to differential filling of the rectum and bladder, Int. J. Radiat. Oncol. Biol. Phys., 20, 1317–1324, 1991. Ten Haken, R. K., Martel, M. K., Kessler,M. L., Hazuka, M. B., Lawrence, T. S. et al., Use of veff and iso-NTCP in the implementation of dose escalation protocols, Int. J. Radiat. Oncol. Biol. Phys., 27, 689–695, 1993. 13 49th AAPM Annual Meeting, Minneapolis, 22-26 July 2007 Ten Haken, R. K., Balter, J. M., Marsh, L. H., Robertson, J. M., and Lawrence, T. S., Potential benefits of eliminating planning target volume expansions for patient breathing in the treatment of liver tumours, Int. J. Radiat. Oncol. Biol. Phys., 38, 613–617, 1997. Terahara, A., Niemierko, A., Goitein, M., Finkelstein, D., Hug, E. et al., Analysis of the relationship between tumor dose inhomogeneity and local control in patients with skull base chordoma, Int. J. Radiat. Oncol. Biol. Phys., 45, 351–358, 1999. Thames, H. D. and Hendry, J. H., Fractionation in Radiotherapy, Taylor and Francis, London (Philadelphia, PA), 1987. Thames, H. D., Schultheiss, T. E., Hendry, J. H., Tucker, S. L., Dubray, B. M. et al., Can modest escalations of dose be detected as increased tumor control? Int. J. Radiat. Oncol. Biol. Phys., 22, 241–246, 1992. Tome´,W. A. and Fowler, J. F., Selective boosting of tumor subvolumes, Int. J. Radiat. Oncol. Biol. Phys., 48, 593–599, 2000. Trapp, J. V., Warrington, A. P., Partridge, M., Philps, A., Glees, J. et al., Measurement of the three-dimensional distribution of radiation dose in grid therapy, Phys. Med. Biol., 49, N317–N323, 2004. Travis, E. L., Lung morbidity of radiotherapy, in Complications of Cancer Management, Plowman, P. N., McElwin, T. J., and Meadows, A. T., Eds., Butterworth and Heinemann, Stonehan, MA, pp. 232–249, 1991. Travis, E. L., Organizational response of normal tissues to irradiation, Semin. Radiat. Oncol., 11, 184–196, 2001. Tucker, S. L., Thames, H. D., and Taylor, J. M. G., How well is the probability of tumor cure after fractionated irradiation described by Poisson statistics? Radiat. Res., 124, 273–282, 1990. Tucker, S. L., Dong, L., Cheung, R., Johnson, J., Mohan, R., Huang, E. H., Liu, H. H., Thames, H. D., and Kuban, D., Comparison of rectal dose-wall histogram versus dose-volume histogram for modeling the incidence of late rectal bleeding after radiotherapy, Int. J. Radiat. Oncol. Biol. Phys., 60, 1589–1601, 2004. van Dyk, J., Keane, T. J., Kan, S., Rider, W. D., and Fryer, C. J., Radiation pneumonitis following large single dose irradiation: A re-evaluation based on absolute dose to lung, Int. J. Radiat. Oncol. Biol. Phys., 7, 461–467, 1981. van Herk, M., Remeijer, O., Rasch, C., and Lebesque, J. V., The probability of correct target dosage: Dose population histograms for deriving treatment margins in radiotherapy, Int. J. Radiat. Oncol. Biol. Phys., 47(4), 1121–1135, 2000. Walker, A. M. and Suit, H. D., Choosing between two formulations of a dose/cure function, Br. J. Radiol., 54, 1012–1013, 1981. Wang, J. Z. and Allen Li, X., Evaluation of external beam radiotherapy and brachytherapy for localized prostate cancer using equivalent uniform dose, Med. Phys., 30, 34–40, 2003a. Wang, J. Z., Guerrero, M., and Allen Li, X., How low is the a/b ratio for prostate cancer? Int. J. Radiat. Oncol. Biol. Phys., 55, 194–203, 2003b. Warkentin, B., Stavrev, P., Stavreva, N., Field, C., and Fallone, B. G., A TCP–NTCP estimation module using DVHs and known radiobiological models and parameter sets, J. Appl. Clin. Med. Phys., 5(1), 50–63, 2004. Webb, S., The effect on tumour control probability of varying the setting of a multileaf collimator with respect to the planning target volume, Phys. Med. Biol., 38, 1923–1936, 1993. Webb, S., Optimum parameters in a model for tumour control probability, including interpatient heterogeneity, Phys. Med. Biol., 39, 1895–1914, 1994. Webb, S. and Nahum, A. E., A model for calculating tumour control probability in radiotherapy, including the effects of inhomogeneous distributions of dose and clonogenic cell density, Phys. Med. Biol., 38, 653–666, 1993. 14 49th AAPM Annual Meeting, Minneapolis, 22-26 July 2007 Webb, S. and Nahum, A. E., Correspondence: Regarding, Wu, Chua, Sham, et al., IJROBP 37(4):913–920; 1997, Int. J. Radiat. Oncol. Biol. Phys., 40, 1009–1010, 1998. West, C. M., Intrinsic radiosensitivity as a predictor of patient response to radiotherapy, Br. J. Radiol., 68, 827– 837, 1995. West, C. M. L., Hendry, J. H., Scott, D., Davidson, S. E., and Hunter, R. D., 25th Paterson Symposium—is there a future for radiosensitivity testing? Br. J. Cancer, 64, 197–199, 1991. Wheldon, T. E., Deehan, C., Wheldon, E. G., and Barrett, A., The linear-quadratic transformation of dosevolume histograms in fractionated radiotherapy, Radiother. Oncol., 46, 285–295, 1998. Wigg, D. R., Applied Radiobiology and Bioeffect Planning, Medical Physics Publishing, Madison, WI, 2001. Willoughby, T. R., Starkschall, G., Janjan, N. A., and Rosen, I. I., Evaluation and scoring of radiotherapy treatment plans using an artificial neural network, Int. J. Radiat. Oncol. Biol. Phys., 34, 923–930, 1996. Withers, H. R. and Taylor, J. M., Critical volume model, Int. J. Radiat. Oncol. Biol. Phys., 25, 151–152, 1993. Withers, H. R., Taylor, J. M. G., and Maciejewski, B., Treatment volume and tissue tolerance, Int. J. Radiat. Oncol. Biol. Phys., 14, 751–759, 1988. Wolbarst, A. B., Optimization of radiation therapy. II. The critical voxel model, Int. J. Radiat. Oncol. Biol. Phys., 10, 741–745, 1984. Wolbarst, A. B., Chin, L. M., and Svensson, G. K., Optimization of radiation therapy: Integral-response of a model biological system, Int. J. Radiat. Oncol. Biol. Phys., 8, 1761–1769, 1982. Xiong, W., Li, J., and Ma, C.-M., Effect of patient variation on standard- and hypo-fractionated radiotherapy of prostate cancer, Phys. Med. Biol., 50, 1483–1492, 2005. Yaes, R. J., The slope of the sigmoid dose response curve for tumor control, Int. J. Radiat. Oncol. Biol. Phys., 44, 470–471, 1999. Yorke, E. D., Dose distributions in normal tissues, Semin. Radiat. Oncol., 11, 197–209, 2001. Yorke, E. D., Kutcher, G. J., Jackson, A., and Ling, C. C., Probability of radiation induced complications in normal tissues with parallel architecture under conditions of uniform whole or partial organ irradiation, Radiother. Oncol., 26, 226–237, 1993. Yorke, E. D., Jackson, A., Rosenzweig, K. E., Merrick, S. A., Gabrys, D. et al., Dose-volume factors contributing to the incidence of radiation pneumonitis in non-small-cell lung cancer patients treated with three-dimensional conformal radiation therapy, Int. J. Radiat. Oncol. Biol. Phys., 54, 329–339, 2002. Zagars, G. K., Schultheiss, T. E., and Peters, L. J., Inter-tumour heterogeneity and radiation dose-control curves, Radiother. Oncol., 8, 353–362, 1987. Zaider, M. and Minerbo, G. N., Tumour control probability: A formulation applicable to any temporal protocol of dose delivery, Phys. Med. Biol., 45, 279–293, 2000. Zavgorodni, S., The impact of inter-fraction dose variations on biological equivalent dose (BED): The concept of equivalent constant dose, Phys. Med. Biol., 49, 5333–5345, 2004. Zelefsky, M. J., Leibel, S. A., Kutcher, G. J., Kelson, S., Ling, C. C., and Fuks, Z., The feasibility of dose escalation with three dimensional conformal radiotherapy in patients with prostatic carcinoma, Cancer J., 1, 142–150, 1995. Zwicker, R. D., Meigooni, A., and Mohiuddin, M., Therapeutic advantage of grid irradiation for large single fractions, Int. J. Radiat. Oncol. Biol. Phys., 58, 1309–1315, 2004. 15