The Language Barrier in Primary Care: Seekers Department of General Practice
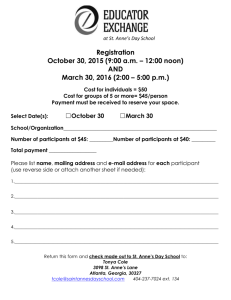
advertisement

The Language Barrier in Primary Care: Perspectives of Refugees and Asylum Seekers Department of General Practice Health Services Research Seminar December 13th 2005 Anne MacFarlane, Department of General Practice, NUI, Galway Unprecedented Patterns of Migration Anne MacFarlane, Department of General Practice, HSR Seminar December, 13 th 2005 Research about Refugee and Asylum Seeker Health Language differences, communication difficulties Refugees, asylum seekers, services providers (primary and secondary care) Use of interpreters Formal interpreters (telephone/face to face interpreting) Informal interpreters (Friends and relatives) Anne MacFarlane, Department of General Practice, HSR Seminar December, 13th 2005 Communication Matters General Practice and nursing Biopsychosocial model of health Participation of patients Patient agenda Patient narratives Shared decision making Anne MacFarlane, Department of General Practice, HSR Seminar December, 13th 2005 CARe Communication with Asylum Seekers and Refugees Conduct an in-depth exploration of the impact of language as a barrier in primary care Document experiences of refugees, asylum seekers & primary care providers Identify key features of the language barrier and its impact Explore solutions and strategies for service development and improvement Anne MacFarlane, Department of General Practice, HSR Seminar December, 13th 2005 Perspectives of Refugees and Asylum Seekers Aim is to document experiences of refugees and asylum who have experience of accessing and using primary care with little or no English Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Research Approach Participatory Learning and Action (PLA) More radical form of organisational action research Derived from Participatory Rural Appraisal (Chambers, 1994c) “growing family of approaches and methods that enable local people to share, enhance and analyse their knowledge of life and conditions, to plan and to act. Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 PLA Key Characteristics Meaningful participation of community members; acknowledging local expertise Focus on concrete actions arising out of data collection Equal relationship between the ‘researcher’ and the ‘researched’ Doing research ‘with people’ rather than ‘on them’ Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 PLA in action Inter-agency Partners HSE WA Health Promotion, Public Health Community Representation Galway Refugee Support Group Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 PLA in action Core group for the research Croatian woman, Ukrainian man, two Russian women and Nigerian woman Research planning – project name and logo, project materials PLA training to facilitate peer researcher model for data collection and data analysis Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Methods: Sampling and Recruitment Purposeful sampling Ethnicity (Serb-Croat and Russian speaking communities) Gender (men and women) 26 participants 16 women and 10 men 10 asylum seekers, 6 refugees, 10 with residency on the basis of having Irish born children Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Methods: Data Collection Topic Guide Research question “Tell me about people’s experiences of language differences and communication difficulties with GPs” Experiences of making appointments Arriving at the surgery, place of consultation Being in the consultation What happens afterwards Experiences with public health nurses and pharmacists Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Methods: Technique Emic card sort Qualitative data ‘Insider’ perspective Researcher elicits stories Interviews them Story broken down onto cards Cards ‘sorted’ thematically by participant Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Methods: Emic Card Sort Story about daughter acting as an interpreter ‘daughter interprets’ ‘daughter interpreter absent from school’ ‘daughter interpreter explains everything’ ‘Sorted’ with cards about friend acting as interpreter Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Methods: Co-analysis of Card Sorts Recording forms translated Sharing of data Manual analysis Framework analysis Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Overview of Thematic Framework GP ‘Attitude’ GPs & Interpreting Responses GP Competency Strategies Competency & Communication Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Strategies for Approaching GPs Three main strategies Use of informal interpreters Friends or relatives, including children Preparing with dictionaries, phrasebooks Gestures and body language Sense of agency among refugees and asylum seekers to manage the language barrier in the absence of an adequate structural supports in general practice Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Children as informal interpreters B2, for instance, a woman aged 37 who is an asylum seeker, married with two children had no English on arrival in Ireland daughter had very good English made appointments for her and interpreted for her during GP consultations absent from school for up to one or two hours This woman tried to attend GP consultations alone with sentences learned by heart ….once she had told her GP these few sentences, she couldn’t ask anything else and the consultation folded. Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 English language ability of informal interpreters B1 is an asylum seeker from Croatia married two children living in direct provision. She had no English when she arrived in Ireland No Croatian speaking friends informal interpreters was a friend from Czechoslovakia because there was some similarity between their languages and they could understand each other a little inevitable misunderstandings during her GP consultations ….on one occasion her son who had diarrhoea was prescribed medication for constipation Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 GPs’ Responses to Interpreters Mixed responses to informal interpreters sent away by GPs to find someone to interpret friends or relatives turned away by GPs resistance to informal interpreters Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Informal Interpreter as a ‘Complication’ B3 a Croatian woman brought her friend along to interpret. Her friend did not have very good English but had better English that the woman. GP felt “friend was just complicating matters” …”understood enough” …B3 emphasised that this view, even if accurate which it was not, did not take into account that she did not have enough English to ask questions of the GP or discuss her case with the GP in any depth Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Formal Interpreting? Only 4 participants had ever used formal telephone interpreters in general practice No participant had access to formal interpreter during the data collection period Formal interpreting highly valued Requests to GPs turned down Limits of formal interpreting Face to face versus telephone Issues of training and professionalism Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Decisions about Interpreters There is a power differential at play whereby decisions about the use of formal and informal interpreters lie with general practitioners rather than with refugees and asylum seekers. Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 GP ‘Attitude’ Z1 described a consultation where her doctor didn’t make any effort to understand what she was trying to say. The GP “switched off”, appeared annoyed and angry and started writing a prescription. Z1 stopped trying to explain herself, took the prescription offered and left. She emphasised how awful it was feeling that the GP wanted to get rid of her. Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Prescriptions and Treatments Being written before participant finished Prescriptions for over the counter medications (eg calpol) Repeat prescriptions for on-going problems Refused tests and investigations Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Attitudes and Language Differences Z6 felt that as soon as she opens her mouth, there is a negative response because the GP realises that there is a language difference. She does not feel attended to by her GP and feels that her/his GP thinks he doesn’t have to explain anything to people with little English In her experience, the GP doesn’t like to be asked many questions, pretends to be busy to “get rid of us”, frequently writing a prescription to end the consultation. Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Lack of English = less responsibility for GPs? K2 believed that GPs do not feel responsible for patients who do not speak English because the patient cannot control or cross check the treatments that are being given. In this way, GPs feels free to prescribe whatever they wish, or to send patient away. Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Lack of English = Lack of Intelligence? B4 felt strongly that GPs think people are less intelligent and stupid if they have bad English. GP openly shows that his lack of English irritates him, sneering when he speaks English. blood test but no result from GP B4 explained that he had no energy for fighting or standing up for himself; he felt humiliated and degraded. Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Relevance of being a ‘foreigner’? D4 describes her GPs manner in their consultations as “superficially pleasant, polite, well-mannered” but holds a strong perception that he is indifferent. an absence of true medical interest in her and engagement with her There is no open racist attitude but, she does wonder whether this underlies his behaviour and manner? Communication is embedded in social relations…there are significant racial and cultural dimensions at play Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Competencies B1 had a small child with bad cough repeat visits to her GP, asked for analysis and tests but the GP would not arrange them A&E diagnosis of asthma was made. New medicines were administered and were effective. B1 thinks that the fundamental problem was that her doctor didn’t listen to her and didn’t take her consultations seriously. Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 GP Competency and Communication Z4 asked “If there is no interpreter and you cannot explain the problem how can you clarify the problem, how can you get quality care from GP?” Competence of GP depends on quality of interpretation Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Responses Significant lack of faith and trust in Irish GPs Unused prescriptions Change GP Prefer hospital A&E department Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Medicine from home Z4 feels strongly that her GP doesn’t care about her or her family’s health. The GP cannot understand the seriousness of the problems and at the end of their consultations Z4 feels like a second class citizen. She only goes to the doctor if it is really really necessary. She uses alternative medicine, such as herbal medicine and supplements from health food shops as much as possible, particularly for her young son who has a skin condition. She also has contact with a Russian doctor in the city who has a cupboard of medicine from home. Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Health Seeking Behaviour Health-seeking behaviour of refugees and asylum seekers is characterised by heterogeneity of actions within which utilisation of GP services is carefully negotiated and managed Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Key Findings Three main informal strategies identified the use of informal gestures/body language interpreters, dictionaries and The inadequacy of these informal strategies has been highlighted problems include the use of children friends/family members who may not be trusted friends/family members who may not actually have ‘good’ English examples of errors and misdiagnoses as a result of language and communication difficulties Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Key Findings Good English does not guarantee ‘problem free’ communication Decisions about the use of formal and informal interpreters lie primarily with GPs. Refugees and asylum seekers do not feel listened to by GPs Profound lack of faith in GP care Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Solutions Accessible and Available Formal Interpreters Trained interpreters Training for uptake and use of interpreters Options for different kinds of interpreting for different kinds of consultations English Classes Exchange of Experiences and Perspectives Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Concrete Actions… Action Research Process and Outcomes Representation, participation, empowerment Impact on health policy and service delivery Presentation to HSE Primary Care Unit Network of regional projects Fellow in Refugee and Asylum Seeker Healthcare MARTA Galway Refugee Support Group Community Health Project Planned national inter-agency conference Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Acknowledgements Peer Researcher Group Galway Refugee Support Group Steering Group Members Mary Kilraine Hannon, Health Promotion, HSE WA Ena Polenjee, Public Health Nurse, HSE WA Ann O Kelly, Centre for Nursing Studies, NUI, Galway PLA Trainers Triona NicGiolla Choille Celine Geoffret Mary O’Rielly de Brun, Centre for Participatory Studies, Co. Galway Tomas de Brun, Centre for Participatory Studies, Co. Galway Research with Service Providers Pauline Clerkin, NUI, Galway Liam Glynn, NUI, Galway Julie McMahon, NUI, Galway Phillipe Mosinike, NUI, Galway Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Perspectives of Primary Care Providers Telephone Survey (GPs and PHNs) n=91/119; Response rate 76%; Qualitative Interviews (GPs) n=12 Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005 Overview of Results Use of interpreters Relative or friend Formal interpreter by telephone Formal interpreter face to face 90% 70% 19% 7% Preference for informal interpreter Preference for formal interpreter Managed without interpretation 36% 41% 63% Accounts of difficulties or sensitivities with informal and formal interpreters Language barrier not perceived as a major problem in their work Anne MacFarlane, Department of General Practice, HSR Seminar, December 13th 2005