Movement Disorders in the Elderly Herbert Sier MD, FACP, AGSF
advertisement
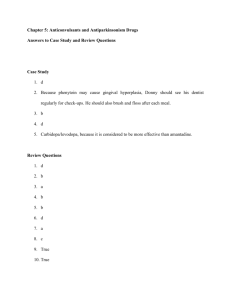
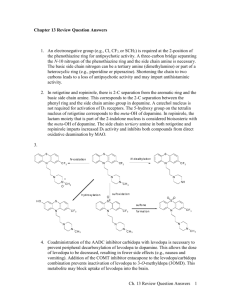
Movement Disorders in the Elderly Herbert Sier MD, FACP, AGSF Clinical Professor of Medicine UCI School of Medicine Movement Disorders Result of dysfunction of the basal ganglia or the extrapyramidal motor system: includes the subsantia nigra, striatum ( caudate and putamen), globus pallidus, subthalamic nucleus and thalamus not weakness or sensory deficits Classified as: Hyperkinesias: (excessive movement) Tremor, Tic, Chorea, Dystonia, Myoclonus, Akathesias Hypokinesias ( paucity of movement): PD A particular movement disorder may be characterized by several types of involuntary movements Parkinson’s Demographic Info 1.5 Million people in USA Affects 1/100 over age of 60 yrs Mean age at diagnosis is 70.5 yrs 5 to 10% of all persons with PD are diagnosed prior to age 40 Affects men and women in equal numbers Some studies: African American and Asians are less likely than Caucasians to develop PD Causes of PD Loss of dopamine producing neurons in substantia nigra results in difficulty with movement Free radicals: contribute to an oxygenation process in brain that damages neurons Toxins: such as pesticides; Viral infections Genetic factors: majority of cases do not have a clear genetic link, while several genes are known to cause specific forms of Parkinsons Accelerated aging in some fashion: mitochondrial dysfunction Diagnosis: PD Chronic progressive neurodegenerative disorder Cardinal signs for diagnosis: Rest tremor: pill rolling Rigidity Bradykinesia Gait disturbance, Postural instability Essential Tremor Present when the limbs are in active use Common in the arms, head and/or voice; may also include the chin, tongue, and legs Amplitude varies: tremor sometimes mild or absent, other times severe May interfere with activities of daily living Family hx is common, tremor improved with alcohol Intention tremor: action tremor increases toward end of action: cerebellum disorders, MS Treatment of Essential Tremor Initial therapy includes BB or primodone Second line drugs include gabapentin, topiramate, mirtazipine, benzodiazepenes Response is variable and tremor is rarely reduced to asymptomatic levels Severe, medically refractory tremor may be treated with deep brain stimulation Other Symptoms of PD Non motor Musculoskeletal: Micrograhpia, dystonia, shuffling gait, freezing, festination Motor Hypomimia: masked facies Decreased blink rate Speech impairment: dysarthria, hypohponia Dysphagia Sialorrhea Vision: gaze problems Differential Dx: PD Dementia with Lewy Bodies Atypical Parkinsonism ( Parkinson Plus) Multisystem Atrophy: Shy Drager, Striatoniagral degeneration, Olivopontocerebellar atrophy. MSA characterized by rigidity, bradykinesia, balance issues, autonomic dysfunction, pseudobulbar palsy, gait ataxia Progressive Supranuclear Palsy: difficulty moving eyes especially looking up, marked trunk as opposed to limb rigidity. Experience balance problems, difficulty swallowing, confusion, or inappropriate behavior Corticobasal Degneration: bradykinesia, rigidity, postural instability, language problems, myoclonus-dystonias, alien limb Differential Dx: PD Secondary: Drug Induced Parkinsons: antipsychotics, metaclopramide, ssri’s, amiodarone Head trauma: boxing Toxins: MPTP, organic solvents Metabolic, Neoplastic: Wilson’s disease Infections: HIV/AIDS, neurosyphilis Small vessel: lacunar infarctions= small strokes in basal ganglia Normal Pressure Hydrocephalus Essential tremor, Intention tremor Diagnostic Testing Careful neurologic exam Blood tests: CBC, Comprehensive Chem Panel Brain imaging: CT or MRI brain Clinical Diagnosis Features suggestive of Parkinsonism other than PD Falls at presentation and early in disease Poor response to Levodopa Symmetry at onset Rapid progression, Lack of tremor, Dysautonomia Gait Dysfunction One of the most disabling signs of PD Slow gait initiation Stooped posture Small shuffling steps Difficulty with turns All create a potential for falls Gait freezing=inability to initiate gait Most pronounced in small spaces like doorways, elevators, crowded spaces, etc. 12 Spectrum of PD Symptomatology Dementia Depression and Anxiety Psychosis Motor Symptoms Autonomic Dysfunction Pain, Fatigue, Olafactory Sleep Dysfunction 13 Non-motor Manifestations of PD Wide distribution of dopamine deficiency Neurodegneration and LB in SN, noradrenergic neurons in locus coeruleus, cholinergic neurons in nucleus basalis of Meynert, and diffusely through cerebral cortex Involvement of non-dopaminergic pathways Serotonin/Cholinergic/Noradrenergic Impact of dopaminergic therapy 14 Nonpharmacological Tx Education Patient and family support Physical and occupational therapy Speech therapy Nutrition is a key Community services/resources 15 Cognitive Dysfunction and Dementia Prevalence of dementia is as high as 41% Lewy Body vs PD Dementia: depends on age of onset Sxs: psychomotor retardation, altered personality, executive dysfunction, visual spatial problems early. Deficits in exec dysfxn occur early on in contrast to AD, where features of aphasia and apraxia occur early. Memory problems early on less prominent than AD. Hallucinations, delusions, paranoia, depression, anxiety are also found in PDD Lewy bodies are seen under microscope, but also amyloid plaques and tangles seen. Lewy Body Dementia Cardinal feature: progressive cog decline that interferes with social and occupational function. Usually motor sxs occur before or within 1 year of PD symptoms, as opposed to late onset PD Supportive features: Core features: Falls, fainting, temporary loss of consciousness, delusions, depression, REM sleep disorders Cognitive fluctuations: thinking ,level of alertness Visual hallucinations PD sxs: stiffness, bradykinesia, gait problems, tremor less likely Treatment: - Rivastigmine ( pill or patch ) - Quetiapine or Clozaril if necessary Mood disorders Psychoses: 20-40% of drug treated pts and visual hallucinations are most common psychotic symptom. All antiparkinson meds can induce psychoses, in addition to the disease itself. Delusions: usually paranoid: spousal infidelity, stealing money Psychoses is single greatest risk factor for NH placement Management of PD Psychosis Rule out symptomatic causes (infection) and correct underlying problems Review medications list--Simplify Step-wise reduction of PD meds anitcholinergics, amantadine, maobi and comt inhibitors, dopamine agonists Consider cholinesterase inhibitor if patient is cognitively impaired Use Atypical Neuroleptics Antidepressants 19 Atypical Neuroleptics Clozapine- “gold standard” 6.25-50mg Very effective (Neurology 2004; 62:381) CBC monitoring due to agranulocytosis Can reduce tremor, and cause weight gain, sedation, OH, seizures ® Quetiapine (Seroquel ) 6.25->200mg sedating, weight gain (Fernandez 2003) ® ® Olanzapine (Zyprexa ), Risperidone (Risperal ), Aripiprazole Can worsen PD symptoms (Neurology 2009; 72: s 1-136) 20 Mood Disorders Depression: most common psychiatric disturbance in PD. Up to 50% have depressive symptoms. Rates of clinically significant depression is 10-20% Anxiety: 29-38%; panic disorder and generalized anxiety disorder seem to be most common Treatment for PD Depression 1. Correct diagnosis 2. Psychotherapy/Counseling 3. Medical management Dopamine agonists (Pramipexole) Anti-depressants: SSRIs most commonly used Mirtazapine or Trazodone Electroconvulsive therapy for severe depression not helped by meds 22 Treatment of Anxiety/Apathy Anxiety Adjust PD meds to minimize off periods SSRIs Short acting benzodiazepines: Alprazolam: 0.5 to 1 mg tid prn Lorazepam: 0.5 to 2 mg prn Apathy - Stimulants: Methylphenidate or Modafinil Sleep Disorders Prevalence: 74-98% have sleep disorders Sleep disorders: Night dreams: reduce dop qhs, ? antipsychotic Insomnia: trouble falling-staying asleep, frequent awakenings: rx behavioral means, possible melatonin, rx pain if interfering with sleep, consider sleep study Restless leg syndrome: rx dop med Periodic limb movement of sleep: rx dop med REM sleep behavior disorder: rx clonazepam Excessive daytime somnolence: rx ? modafinil Rx: Autonomic Dysfxn in PD Orthostatic hypotension Behavioral: elevating head of bed, compression stockings, increasing salt and fluid consumption Fludrocortisone Midodrine Droxidopa Domperidone Rx Autonomic Dysfunction Nocturia/urinary incontinence Rule out urinary infection and other causes Consider urologic evaluation Meds for Detrusor Hyperactivity Constipation Bowel regimen, dietary changes, exercise Hypersalivation Glycopyrrolate Botulinum toxin Hyperhydrosis Very refractory to treatment Adjustment of dopaminergic meds ( on/off issues) Botulinum toxin for focal hyperhydrosis Pharmacologic Treatment Neuroprotective: none definitively shown MAOB inhibitors: Rasagline: can block free radical formation Dopamine agonists: neuroprotective in lab because they act as antioxidants and free radical scavengers Coenzyme Q10: stimulated by evidence that mitochondrial dysfunction may paly a role in pathogenesis of PD NMDA antagonists: antiexcitatory Gene therapy: prevent protein accum/aggregation Symptomatic Therapy Effect of disease on dominant hand Degree to which disease interferes with functional activities, work, ADLs, or social or leisure activities Presence of significant bradykinesia or gait disturbance Major drugs: Levodopa MAOB inhibitors Dopamine agonists Comt inhibitors Anticholinergic Agents Amantadine Levodopa In elderly: often first line agent Usually combined with a peripheral decarboxylase inhibitor carbidopa to block its conversion to dopamine peripherally in order to prevent nausea, vomiting and orthostasis. Immediate vs Controlled release Adverse: nausea, somnolence, dizziness, headache, OH Associated with higher risk of dyskinesias than direct dopamine agents Complications Long-term Levodopa Tx Decreased response to Tx Less “on” time Unpredictable motor fluctuations Drug induced dyskinesias, hallucinations Motor complications: related to nonphysiologic pulsatile stimulation of dopamine receptors Does not treat nondopaminergic sxs 31 Dopamine Agonists Ropinorole, Pramipexole, Rotigotine patch, Apomorphine Advantages Effective monotherapy early on Levodopa-sparing effect as adjuncts to levodopa later on Reduced incidence of levodoparelated adverse events Potential neuroprotective effect Often initial agent in those less than 65 Ineffective in those who show no response to levodopa Disadvantages Less potent Long titration schedule More prone to induce cognitive side effects More prone to cause somnolence Do not eliminate need for Levodopa eventually Not Rx non dopaminergic sxs N/V/OH/legedema/hallucinations /confusion Somnolence, ICD 32 MAOB Inhibitors Modestly effective as sx treatment in early disease, may be used as adjunct to levodopa (may increase on time while reducing motor fluctations) Value for neuroprotection is unclear Adverse: nausea, headache; confusion, OH, dyskinesias, insomnia; need to be careful with SSRI antidepressants. Usually does not cause a hypertensive crisis when eating tyramine rich foods Agent: Rasagiline COMT Inhibitors Mechanism: inhibit catechol-o-methyl transferase and degredation of dopamine, and prolongs activity of dopamine in the brain Useful in treating motor fluctuations, wearing off. Only effective when used with levodopa Adverse: due to increased dopaminergic stimulation and include dyskinesia, hallucinations, confusion, nausea and OH Agent: Etacapone Anticholinergics Most helpful with tremor Problems in elderly due to anticholinergic side effects: Constipation Confusion Hallucinations Urinary retention Dry mouth Tachycardia Amantadine Antiviral agent initially used for influenza Mech of action: uncertain Known to increase dopamine release, inhibit dopamine reuptake, stimulate dopamine receptors, and may exert anticholinergic effects Relatively weak AntiPark drug, but may be useful in early or mild PD and perhaps later if dyskinesia becomes problematic Adverse: livedo reticularis, ankle edema, confusion, halluincations, nightmares Motor Fluctuations 50% of patients on levodopa for 5 years experience MF and dyskinesias As disease progresses, effect of levodopa tends to wear off earlier after doses. MF: are alterations between periods of being on, which there is a good response to med, and being off during which the patient has increased PD symptoms Wearing Off Management Increasing dose of levodopa: issue dyskinesias Shortening interval between doses and decreasing dose at each administration Long acting Sinemet CR may be useful in early stages of wearing off phenomenon, but then does not work, so not great plan Addition of dopaminergic agonist and decrease of levodopa dose Addition of COMT inhibitor, often need to reduce dose of levodopa MAOB inhibitor: Rasagiline may be added Failure of On Response Management May be due to delayed gastric emptying, which results in inadequate plasma concentration of drug due to narrow therapeutic window Avoid taking Levodopa with high protein meals Take 30 minutes before eating In future: Different preparation of levodopa, such as gel infusion via g tube Dyskinesias Variety of involuntary movements, occur as a direct effect of levodopa. Occur in up to 30-40% after 5 yrs of Levodopa and nearly 60% by 10 years Usually choreiform: continuous, restless appearing movements of extremities, head, face, trunk, and respiratory muscles. But can also take form of large amplitude ballistic movements that interfere with function Dyskinesias Peak dose dyskinesias most common Management: for dyskinesias or dystonias Lowering dose of Levodopa Reducing dose of adjunctive drugs with Levodopa such as MAOB inhibitors, COMT inhibitors In more advanced patients may need to greatly reduce dose of Levodopa and go up on Dopamine agonists Amantadine may be useful in advance PD with dyskinesias For early morning dystonias: bedtime dose of sustained release levodopa/carbidopa or long acting dopamine agonist. Surgical Treatment for PD Used when MFs, tremors or dyskinesias are severe and meds no longer working, or unable to tolerate side effects of Anti PD meds Generally done on younger patients PDD is a contraindication to surgery Rationale for surgery: Striato nigral degeneration and dopamine deficiency leads to excessive Subthalamic Nucleus excitation of the Globus Pallidus, and excessive GP inhibition of the Thalamus. This causes symptoms of rigidity and akinesia Surgical Treatment: PD Pallidotomy: ablates GP and reverses the excess pallidal inhibitory effect: non reversible surgery Deep brain stimulation: preferred method now, it suppresses GP inhibition: generally not done in frail elderly Decreases dyskinesias and MFs Studies have shown effect good for at least 5 yrs after initiated Surgical complications: Death: 0.6% Permanent neurologic sequelae: 2.8% Hemorrhage: 3.1% Infection: 4% Confusion: 3.1%, especially in postoperative period Depression CSF leak: 0.6% Hardware malfunction: 2.5 – 5% Tics Repetitive stereotyped purposeless brief actions, gestures, sounds, and words that emerge suddenly from a background of normal motor activity Simple: blinking, facial grimacing, neck movements throat clearing, grunting: generally quick and short lived Complex: sequenced, stereotyped acts: tapping or touching, obscene gesturing, Tourettes in young Rx: - focal tics blinking: botulin toxin injections Centrally acting alpha agonists such as clonidine first line drug; clonazepam may be helpful - meds that block dopamine transmission: tetrabenazine and reserpine, neuroleptic drugs ( but significant side effects ) Dystonias Torsional , twisting movement that is slightly sustained at peak of contraction and may cause twisted postures Involves the basal ganglia Path: idiopathic, infectious, ischemic, hypoxic, drug induced, metabolic, genetic, or degenerative, PD, Wilson’s Disease Focal: spasmodic torticollis, craniofacial, eyelids or hands: responds to botulin toxin Anticholinergic and baclofen: improvement limited Chorea Flowing, continuous, random movement that flits from one part of the body to another; arises from dysfunction of striatum Cause: linked to basal ganglia: Huntington’s disease, drugs, stroke, age ( senile chorea ), PD, post infectious, autoimmune, hemiballism Rx: dopamine depleter or dopamine D2 receptor blockers Tetrabenazine: FDA approved for HD; associated depression, parkinsonism, QT prolong Typical or atypical antipsychotics ( OL ) associated with tard dyskinesia, parkinsonism, metabolic syndrome Myoclonus Single, rapid, shocklike muscle jerk Causes: postanoxic, neurologic diseases such as Cretuzfeldt-Jakob, Alzheimers, paraneoplastic, metabolic ( uremic or hepatic encephalopathy Physiologic: sleep states nocturnal myoclonus, hiccups Focal restricted to body part: from tumor or stroke Generalized: disease involving cerebral cortex diffusely: hypoxia or encephalitis Rx: anticonvulsant agents with antimyocloinc activity: valproic acid, clonazepam, levetiracetam Akatheisa Inner restlessness coupled with repetitive movements Cause: Parkinsonism Drug induced tardive dyskinesias Restless leg syndrome Drug Induced MD Antipsychotics can cause acute dystonia; treat severe cases with IV diphenhydramine or lorazepam Chronic reversible movement disorders can occur with: Lithium, theophylline, valproic acid, antiemetics, antipsychotics, estrogen, antiepileptics, dopamine replacement therapy in PD Chronic non reversible: usually antipsychotic: tardive dyskinesia, dystonia, myoclonus, tics, akathesia Tardive Movement Phenomena Chronic and irreversible; older age and duration of antipsychotic treatment are risk factors May begin weeks or months after initiation of drug; outcome improved if offending drug can be stopped Rx: reduce or eliminate med causing the problem Rx includes trihexyphenidyl, baclofen (ol), tetrabenazine (ol) or clozapine (ol) Botulin toxin (ol) injections are an option for severe cases of dystonia (neck jerking or sustained eye closure)