Practical Principals of Inpatient Opioid Pain Management
advertisement
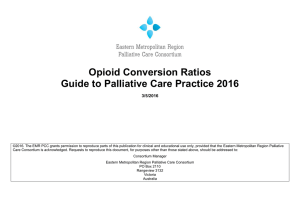
Cory Taylor, MD January 15, 2016 56 year-old veteran with obstructive sleep apnea presents with subacute abdominal pain. CT findings are concerning for gastric adenocarcinoma. The patient is complaining of 10/10 pain and the nurse wants to know what you would like to give him… Understand practical pharmacology behind selecting dose amounts and frequencies Appreciate the different ways of making opioids available to patients Bring balance to the Force and order to your opioid selection Prepare for the possible respiratory side effects of opioid administration Onset: informs the dose amount IV speed of onset (fastest-slowest) Fentanyl ≈ Heroin : Dilaudid : Morphine PO speed of onset (fastest-slowest) Oxycodone ≈ Dilaudid : Morphine ≈ Hydrocodone ≈ Codeine* IV time to max efficacy = 10 min PO time to max efficacy = 60 min Duration: informs the dose frequency Dilaudid, Morphine, Hydrocodone, Oxycodone = 4 hours* Practically Speaking… • Opioids should be dosed at least Q4H to prevent gaps in the maintenance of pain control PRN or “As • PROS Needed” Dosing Patient triggered – they can only get what they ask for Added layer of overdose protection Set it and forget it – less thought, faster ordering • CONS Time to administration can take 30-60 min depending on staff Leads to coverage gaps, poorly controlled pain Makes patient’s feel dependent, disempowered, or “seeking” Creates nursing-patient tension => increased nursing stress Overlooks altered or less verbal patients Interferes with patient sleep Around-the-clock or “Scheduled” Dosing • PROS Better coverage, better control, better sleep Patients are empowered – reduces patient/nursing tension Easier on nursing workflow Don’t need, don’t want: patients can always refuse • CONS Need holding parameters* Dynamically inflexible with changes in metabolism or mental status Takes more time and thought Basal-Breakthrough Dosing ATC dose provides basal coverage PRN dose covers breakthrough pain • PROS Less nursing pages Better satisfaction scores • CONS More time ordering, thinking Can increase demands on nursing staff* Enter the PCA • Best of every world Patient finally feels some control over their illness Nursing can set and forget Doctor can set and [sort-of] forget • Responsiveness + Precision => Finesse Smaller doses, greater frequencies, immediate delivery Allows for precise and expeditious titration up or down No coverage gaps Streamlines opioid consolidation and conversion • No safer alternative than Bolus-only PCA* • CONS Requires cognitive function and trigger-ability Parenteral administration only # 1: Opioid Solidarity • Stick to a single opioid type • Less medication errors • Easier for titration and conversion # 2: Opioid Equivalency • No one opioid activates receptors better than others • Some opioids are more potent, but potency can be overcome by concentration • But some patients will maintain that one opioid “works better for me” than another… Opioids are more like loop diuretics than antibiotics With antibiotics, one may “cover” the patient’s infection where another fails With opioids – Morphine : Lasix as Dilaudid : Bumex* Consequences of sub-optimal utilization • Can inadvertently reinforce drug-anchoring or drug- seeking behaviors • Can detract from future encounters and therapeutic relationships You give the patient an basal-breakthrough opioid regimen. Later on that night, the nurses calls to inform you the patient’s oxygen saturation is 80%. He wants to know if you should dial back on the opioids… See Notes Section for Discussion Not all opioid-related sleep is opioid narcosis Opioid-induced narcosis produces resistant or refractory somnolence Healthy opioid-related sleep in wake-able Opioid overdose always leads to somnolence before respiratory failure Respiratory failure is caused by decreased respiratory drive* Keep in mind: respiratory rates of 8-10 are normal in healthy individuals Responsiveness to naloxone in altered mental status is not diagnostic for opioid-narcosis Naloxone blocks the body’s natural endorphinmediated suppression of pain • Can cause pain and discomfort, even in healthy individuals Responsiveness to naloxone = responsiveness to noxious stimulus Morphine SR + percocet for breakthrough Morphine IVP PRN for moderate pain + Dilaudid IVP PRN for severe pain Fentanyl drip + oral dilaudid q6h as needed Norco q4H ATC + Norco Q2H PRN Oxycontin + tramadol See additional slides for supplemental material* EQUIANALGESIC DOSING GUIDELINES FOR CHRONIC PAIN CHANGING ROUTES OF ADMINISTRATION PO/PR IV/SC/IM 3 1 CHANGING ANALGESICS OPIOIDS Enteral Dose Analgesic (Oral, Rectal) 150 Meperidine 150 Tramadol 150 Codeine 15 Hydrocodone 15 Morphine 10 Oxycodone 5 Oxymorphone 3 Hydromorphone 2 Levorphanol Fentanyl *1000 mcg = 1 mg: must convert to mg to calculate equianalgesic dose Epidural 0.1 Intrathecal 0.01 Parenteral Dose (SC/IV/IM) 50 50 5 1 1 0.050 mg* TRANSDERMAL FENTANYL METHADONE Daily Morphine Dose (mg/24 hrs PO) < 100 101 - 300 301 - 600 601 - 800 801 - 1000 > 1000 > 2000 - 5000 > 5000 Conversion Rates Morphine PO Methadone PO 3 1 5 1 10 1 12 1 15 1 20 1 40 1 80 1 METHADONE SC DOSING 1. Convert from daily Morphine Equivalent PO Dose / 24 hrs to Methadone PO Dose / 24 hrs using the Methadone PO Dosing Table above 2. Then ÷ 2 to convert to Methadone SC Dose/24 hrs ADJUSTING FOR INCOMPLETE CROSS TOLERANCE Complete Near-complete Incomplete Morphine 50 mg PO in 24 hrs ≈ Fentanyl 25 mcg transdermal patch q 72 hrs Ferris FD and Pirrello RD: Improving Equianalgesic Dosing for Chronic Pain Management, American Association for Cancer Education Annual Meeting, oral presentation, Cincinnati, Ohio, September 2005 These are guidelines only and do not replace clinical judgement. © International Programs, OhioHealth, 2013. Permission to reproduce material is granted for non-commercial educational purposes only, provided that the attribution statement and copyright are displayed To reproduce for all other purposes, contact The International Programs at 1-888-278-6615 or visit IPCRC.net 100% 75% 33-50% Faster onset, time to peak, and other factors can increase the euphoria associated with a given opioid Euphoria is sometimes mistakenly perceived by patients as increased efficacy • => increased drug-anchoring/requesting behaviors • Euphoria ~> dependency, STREET VALUE Not all aberrant behavior is drug-seeking behavior • Traffickers are not always abusers Desperate or anchoring behavior ≠ “drugseeking” behavior • Legitimate patients with undertreated pain or opioid withdrawal have genuine needs Negative or discordant urine drug screen Inconsistency of story Splitting Provider-jumping Losing prescriptions RED FLAGS Poor self-care or selfinvestment Running out of medication Haggling or making demands Irrationality, especially regarding equivalent doses YELLOW FLAGS