Hospital-Acquired Pneumonia Internal Medicine Mini-Lecture Revised Jan 2016
advertisement
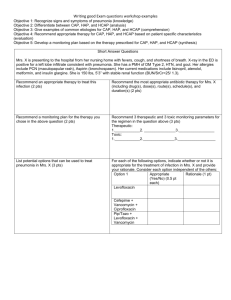
Hospital-Acquired Pneumonia Internal Medicine Mini-Lecture Revised Jan 2016 Learning Objectives • Definition of Hospital-Acquired Pneumonia (HAP). • Risk factors associated with HAP. • Current treatment guidelines Clinical Case 68-yo female with insulin-dependent diabetes presents with 2day history of fever, cough, and pleuritic chest pain. She had knee replacement surgery 60 days ago and spent 2 weeks at a rehabilitation facility. On exam, temp 101.8 F, HR 124, BP 110/76, RR 24 with O2 sat 92% on RA. She is alert and oriented with NAD. Auscultation reveals RLL crackles. White count 18,000 with L shift, BUN 32. CXR shows focal consolidation in RLL. What antimicrobial treatment should be initiated? Definitions Hospital-acquired pneumonia, HAP Pneumonia occurring more than 48 hours after admission, not present at admission. Ventilator-associated pneumonia, VAP Pneumonia developing 48 hours after endotracheal intubation. Definitions Healthcare-associated pneumonia, HCAP Pneumonia that occurs in a patient with extensive healthcare contact, one or more of the following: • IV therapy, wound care, or IV chemotherapy within the prior 30 days. • Residence in a nursing home or long-term care facility • Hospitalization in an acute care hospital for two or more days within the prior 90 days • Attendance at a dialysis clinic within the prior 30 days Risk Factors for HAP Modifiable Non-modifiable Depressed level of consciousness Age > 70 years Enteral nutrition Immunosuppression Malnutrition Thoracic or abdominal surgery Mechanical ventilation Underlying chronic lung disease Oropharyngeal colonization Re-intubation Stress ulcer prophylaxis Supine position Treatment Empiric treatment guidelines depend on whether HAP is early or late onset (>4 days) and risk factors for MDR pathogens present. Risk Factors for Multi-Drug Resistant pathogens • Antimicrobial therapy in preceding 90 days • Onset of pneumonia after 5 days of hospitalization • High frequency of antibiotic resistance in the community or hospital unit • Duration of ICU stay and mechanical ventilation • Immunocompromised state American Thoracic Society, Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcareassociated pneumonia. Am J Respir Crit Care Med 2005; 171:388. Treatment For early onset with no MDR risk factors: • Pathogens include S. pneumo, H. influenzae, MSSA, E. coli, Enterobacter, Proteus. • Recommended antibiotics: Ceftriaxone or Levofloxacin or Unasyn or Ertapenem. Source: American Thoracic Society, Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 2005; 171:388. Treatment For late onset or MDR risk factors present: • Pathogens include Pseudomonas, Klebsiella ESBL, Acinetobactor, MRSA, Legionella. • Recommended antibiotics: Cefepime or imipenem or Zosyn PLUS levofloxacin or gentamicin PLUS vancomycin or linezolid Source: American Thoracic Society, Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 2005; 171:388. Special considerations No evidence indicates that HAP or VAP caused by Pseudomonas species requires combination therapy or that a synergistic combination improves outcomes. Oral anaerobe coverage may be considered for patients with a witnessed aspiration event or recent surgery. All patients should be re-evaluated for clinical improvement and review of microbiologic results at 48 to 72 hours and considered for de-escalation (narrow spectrum or oral therapy). Special considerations The duration of therapy for HAP and VAP is generally 7 to 8 days except in cases caused by Pseudomonas or Acinetobacter spp., for which treatment should continue for 14 days. Patients who do not improve within 72 hours of appropriate antimicrobial therapy should be evaluated for infectious complications (e.g. empyema or lung abscess), an alternate diagnosis (e.g. PE, ARDS, neoplasm), or another site of infection (e.g. C. diff colitis, pleural effusion) to explain the clinical picture. Clinical Case 68-yo female with insulin-dependent diabetes presents with 2day history of fever, cough, and pleuritic chest pain. She had knee replacement surgery 60 days ago and spent 2 weeks at a rehabilitation facility. On exam, temp 101.8 F, HR 124, BP 110/76, RR 24 with O2 sat 92% on RA. She is alert and oriented with NAD. Auscultation reveals RLL crackles. White count 18,000 with L shift, BUN 32. CXR shows focal consolidation in RLL. What antimicrobial treatment should be initiated? Clinical Case Patient was started on Cefepime, Levofloxacin, and Vancomycin for HCAP with MDR risk factors. She is at risk for MDR pathogens due to her history of diabetes and recent knee surgery with subsequent rehab. On hospital day 3, sputum culture grew MRSA. Cefepime and Levofloxacin stopped. After a 10-day course of Vancomycin, patient improved and was sent home. Summary • Prompt, appropriate, broad-spectrum antimicrobial therapy should be started for all patients with suspected HAP. • Patients with HCAP need therapy for MDR pathogens. • De-escalation of antibiotics should be considered once the results of culture and patient’s clinical response are known. • Nonresponding patient should be evaluated for possible MDR pathogens, extrapulmonary sites of infection, and noninfectious causes. References • American Thoracic Society, Infectious Disease Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcareassociated pneumonia. Am J Respir Crit Care Med 2005; 171:388. • American College of Physicians. MKSAP 17: Infectious Disease. 2015: 82-84. MKSAP question 59-yo man is evaluated in the ICU for fever and leukocytosis. He was admitted 13 days ago with respiratory failure resulting from Guillain-Barre syndrome. He was intubated and mechanically ventilated. On hospital day 9, he developed fever without an increase in secretions or change in oxygenation. A new left lower lobe infiltrate was seen on chest X-ray, and his leukocyte count was 17,500. Sputum culture grew MSSA. Nafcillin was started. Medical history is otherwise unremarkable. Medications are nafcillin and IVIG. MKSAP question On exam, temp is 100.8 deg F, blood pressure is 132/84 mm Hg, pulse is 94/min, and respiratory rate is 18/ min. Lung exam reveals decreased breath sounds in the left lower lung field. Lab studies show a leukocyte count of 17,300. Sputum gram stain reveals 1+ leukocytes and 1+ gram-positive cocci in clusters. Remainder of the exam is noncontributory. A new moderate left pleural effusion is seen on chest X-ray, but no increase in the LLL infiltrate. CT scan shows LLL consolidation with air bronchograms and a moderate left pleural effusion. MKSAP question Which of the following is the most appropriate next step in management? (A) (B) (C) (D) Add gram-negative antimicrobial coverage Change nafcillin to vancomycin Perform bronchoscopy with bronchoalveolar lavage Perform thoracentesis MKSAP answer Answer: (D) perform thoracentesis This patient should undergo thoracentesis to determine why he is not improving with treatment. In patients who do not respond to appropriate treatment after 72 hours, it is imperative to search for another explanation (such as infectious compication, another site of infection, or an alternate diagnosis). A new or increasing pleural effusion could represent a parapneumonic effusion, empyema, or a lung abscess. Thoracentesis and pleural fluid examination should be performed because the results could significantly alter management.