Focal segmental glomerulosclerosis Medical Grand Rounds Jeffrey Kopp, MD Harbor
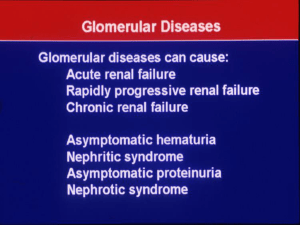
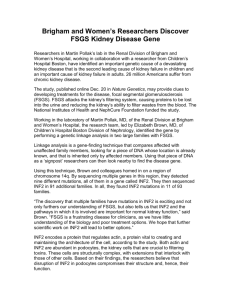
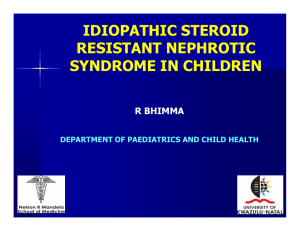
advertisement
Focal segmental glomerulosclerosis Medical Grand Rounds Harbor Irvine USC Jeffrey Kopp, MD Primer on the National Institutes of Health 27 Institutes/Centers: NCI, NHLBI, NIAID, NIDDK … Bethesda campus 18,000 people Baltimore, Frederick, MD; Research Triangle Park, NC; Phoenix, AZ … Principal investigators 1100, each leading a research group Postdoctoral fellows 5000 Clinical Research Center 240 beds - all “GCRC” Outpatient visits 100,000/yr How the NIH Clinical Center works Every patient is on a protocol Care is provided at no cost: hospitalization, clinic visits, medications related to protocol Travel and lodging (outpatients) is provided 1500 protocols – 48% involve treatment NIH is particularly expert at and interested in Pathophysiology of disease Rare diseases First in human trials Training and Faculty positions at NIH Summer internships Post-baccalaureate fellowships Medical Student rotations, residencies and fellowships Medical Student Research Program: 1 year in Clinical or Basic Research at NIH Postdoctoral Research fellowships Stadtman Fellowships: Tenure Track , cross-institute, mostly basic Lasker Clinical Scholar Awards: 12 year awards: 5 y intramural, 7 yr extramural Tenure track positions Training.nih.gov NIH Program Level in Nominal Dollars and Constant Dollars “Doubling” FY17 initiatives Cancer moonshot Precision medicine: million person cohort Brain research Lecture objectives • Review common causes of nephrotic syndrome • Appreciate that focal segmental glomerulosclerosis is set of syndromes, with distinct mechanisms and therpaies • Understand the role of APOL1 genetic variants in causing FSGS and related diseases Causes of end-stage kidney disease in adults most are diseases of the glomerulus Diabetes 40% Hypertension 30% Glomerulonephritis 20% Cystic 10% ESKD causes more premature deaths than most cancers Incident ESKD cases by cause Kidney diseases ESKD cases Diabetes 48,157 Hypertension 29,105 Glomerulonephritis 9,978 FSGS, including AIDS nephropathy 3,449 Myeloma kidney 1,215 Lupus nephritis 1,104 Cystic kidney diseases Total 2,613 ~100,000 USRDS 2008 Glomerular filtration barrier = endothelial cell + glomerular basement membrane + podocyte Renal blood flow ~1000 ml/min Renal plasma flow ~600 ml/min Filtration fraction ~15-20% Glomerular filtration ~100 ml/min = 150 L/d Tubular reabsorption ~99% Glomerular ultrastructure (electron microscopy) Urinary space 3 Blood 2 1 Model of slit diaphragm molecular assembly Tryggvasson, NEJM 2006 Nephrotic syndrome: diagnostic features • Proteinuria >3.5 g/d or spot urine protein/creatinine ratio ≥2 g/g • Reduced serum albumin • Hyperlipidemia Serum albumin 5 4 3 2 1 0 0 12 24 36 Months • Edema 48 60 Nephrotic diseases are podocyte diseases Fogo, JCI 2011 Podocyte depletion > segmental glomerular scar > global gomerulusclerosis GBM contacts Bowman capsule (synechia) Glomerular filtrate is misdirected into paraglomerular space, which enlarges and traps additional capillary loops, stressing additional podocytes Accumulation of matrix proteins (mesangial cell?) Remaining capillary loops hypertrophy, further stressing podocytes Kriz, Kidney Int 1998 Mechanisms of glomerular injury: podocyte injury in context Category Specific mechanism Clinico-pathologic syndromes Autoantibody against glomerular antigen ANCA vasculitis Ag/Ab complexes depositing in glomerulus Lupus nephritis Membranous nephropathy IgA nephropathy Complement deposition Post-infectious glomerulonephritis Lupus nephritis Membrano-proliferative GN Other deposition Immunoglobulin light chain Serum amyloid protein Amyloid nephropathy GBM Genetic, ab Alport, Goodpasture Endothelial injury Complement, toxin, other Thrombotic microangiopathies Podocyte dysfunction (e.g.nephrin) Genetic focal segmental glomerulosclerosis (FSGS) To be discovered! Minimal change disease Primary FSGS Excessive glomerular load (e.g. obesity) or insufficient glomerular number (e.g. premature birth) Podocyte dysfunction Adaptive FSGS Podocyte dysfunction Viral FSGS (HIV, CMV…) Glomerulonephriitis Podocyte injury Focal segmental glomerulosclerosis Barisoni Map of FSGS, 1957 Terra incognita Rich, Bulletin Johns Hopkins Hosp, 1957 FSGS syndrome: six mechanistic groups Primary: cytokine, immune activation Mendelian genes >30 Virus: HIV, CMV, B19?, EBV? ? APOL1 72% AA FSGS Features of/mimics all other groups Medication: IFN, Lithium, Bisphosphonate Adaptive FSGS Mismatch: glomerular load > glomerular capacity FSGS course: Proteinuria response to therapy predicts long term outcome Complete remission (20% of cases) Partial remission (40% of cases) No response (40% of cases) Troyanov..Cattran, JASN 2005 Pathologic approach to FSGS: Columbia classification decision tree ≥1 glomerulus with hyalinosis or sclerosis IF limited to IgM and C3 EM immune deposits limited to mesangium Collapsing variant? Tip lesion? Cellular lesion? Perihilar variant? Not Otherwise Specified (NOS) = classic FSGS D’Agati, Fogo, Bruijn Jennette, AJKD 2004 Clinical relevance of FSGS classification: frequency and course Variant Frequency (total N=192) Collapsing variant 11% Tip lesion 17% Cellular lesion 3% Perihilar variant 26% NOS 42% Patients at risk … Tip n = 34 Perihilar 50 NOS 78 Collapsing 20 Thomas, KI, 2006 Tip Perihiilar NOS Collapsing 26 35 47 12 Renal Survival (years) 22 21 33 5 19 12 17 3 11 4 6 3 Mechanistic approach to FSGS Mechanism Primary Adaptive APOL1 Mendelian Genetic Medication Virus Subtypes Most cases: idiopathic suPAR? Cardiotrophin-like cytokine? Mismatch hypothesis: Decreased glomerular number/hypertrophic capacity and increased metabolic load (FSGS, HIVAN, arterionephrosclerosis) Monogenic: >30 genes (inheritance AR, AD, mitochondrial) Pamidronate (collapsing) Interferon a b or g, lithium CNI, amphotericin (adaptive) HIV, CMV, B19? EEBV? Biopsy report returns FSGS Historical data: family history, birth history (gestational age, weight) Renal biopsy findings Laboratory data: proteinuria, serum albuminuria Response to therapy Primary FSGS: characteristics May have a characteristic presentation Distinct or even explosive onset Heavy proteinuria (>4 g/d) Low serum albumin (<3 or lower) Marked hyperlipidemia Light microscopy: tip lesion or collapsing glomerulopathy suggestive Electron microscopy: widespread foot process effacement Role of circulating plasma factors Recurrent FSGS after kidney transplant ~25%. Risk factors: FSGS onset <6 yr, rapid progression to ESKD (<3 yrs), and to a lesser degree white race, LD transplant Bioassay for the elusive factor (rat glomerular albumin permeability in vivo) is not useful for patient care: not sufficiently predictive Candidate molecules: soluble urokinase-type plasminogen activator receptor (SUPAR), cardiotrophin- like cytokine factor-1 (CLCF1) Prevention: plasma exchange? Treatment: plasma exchange? Cyclophosphamide? Rituximab? Adaptive FSGS: biopsy findings Large glomeruli Perhilar sclerosis: ≥50% of sclerotic glomeruli have sclerosis confined to hilar quarter of glomeruli (sensitivity and specificity unknown) Obesity-related FSGS Only partial foot process effacement, mean 40% vs 75% but much overlap Mismatch: increased load versus decrease increased filtration capacity > increase single nephron glomerular filtration Controls Khambam..D’Agati, KI, 2001 Helal ..Schrier, NRN 2012 Adaptive FSGS: clinical features Premature or small for gestational age Nephrotic or sub-nephrotic proteinuria “Bigness” - obesity or tall/muscular May have preserved serum albumin RAAS antagonism: proteinuria may fall >50% CNF, FSGS, DMS: 25 genes are implicated, functioning in 7 cellular compartments/functions Genes Cell Matrix Slit diaphragm Cytoskeleton Mitochondria DNA repair transcription Cell signaling Lysosome 2 5 5 7 6 2 1 NPHS1 ACTN4 INF2 * WT1 * PLCE1 NPHS2 INF2 * NEIL1 TRPC6 CD2AP AHRGP24 PTPRO AHRGDIA Nonsyndromic * = appear > once MYO1E Syndromic ITGB4 MYH9 Epstein, Fechtner LAMB2 Pierson INF2 CharcotMarie-Tooth * WT1 DenysDrash, Frasier * tRNA –leucine MELAS LMX1B Nail-patella COQ2 SMARCAL1 Schimke COQ6 NXF5 PDSS2 Leigh Most recessive, 8 autosomal dominant, 1 mitochondrial DNA ADCK SCARB2 Action mycoclonus Cellular pathways and podocyte genetics: 7 known and 5 pathways could be speculated Cell signaling Slit diaphragm Cell/matrix interaction Nucleus Lysosome Mitochondrion ER stress – unfolded protein response Secretory pathway Cytoskeleton Endocytosis Cell polarity Autophagy Genetic testing depends on clinical context Setting (onset age) Non-syndromic Syndromic Infant (<1 y) with nephrotic NPHS1, NPHS2, LAMB2, As suggested by syndrome WT1, PLCE1 clinical findings Child 1-10 with SRNS/FSGS NPHS2, LAMB2, WT1, PLCE1 “ Child with SSNS/FSGS, with PLCE1, PTPRO + FH - Child/adolescent 10-18 with SRNS - Adult with FSGS and family history INF2, ACTN4 TRPC6, WT1 Adult lacking family history Generally not tested “ “ Hinkes, Pediatrics 2007; Ismaiil Ped Nephrol 2009; Santin, CJASN 2011; McCarthy, CJASN 2013 Why test for FSGS genetic mutations? • Extra-renal manifestations • Prognosis • Therapy. Generally steroids don’t work. Calcineurin inhibitors may work. RAAS antagonist. • Kidney transplant: FSGS recurrence is unlikely • Family screening • Every patient/family deserves a molecular diagnosis, when feasible (Hildebrandt) FSGS treatment algorithm Primary FSGS >2-3 g/d despite RAAS antagonist + Primary FSGS, <2 g/d or diuretic and preserved GFR risk for treatment toxicity (>40-50 ml/min/1.73m2 ?) Genetic FSGS Adaptive FSGS Daily prednisone CSA or tacrolimus ACEI or ARB ± Aldo blocker MMF Blocking RAAS: Renin-angiotensin-aldosterone and more PTXF mAb PAI-1 Leptin CTGF ARB Ang Ang I Angiotensin Receptor I Ang II ACEi Aliskeren Renin Angiotensin converting enzyme PTXF TSP-1 NEP Aldo Spironolactone Eplerenone TGFb1 ET-1 Bosentan Pirfenidone Tranilast fresolimumab FSGS: Time to remission (complete + partial) with steroid Rx Dose 1 mg/kg up to 80 mg Continue 8 – 16 wk Proteinuria reduced by 50%: slow taper Proteinuria not reduced: rapid taper Alternatives 80 or 120 mg QOD Pulse oral dexamethasone: 25 mg/m2 d1-2-3-4, repeat q28d X 8 cycles (Cho, submitted) Rydel AJKD 1995 ESKD incidence ~100,000 cases/yr: Major African American health disparity ESKD Cause All causes 3.4 Diabetes 3.7 Hypertension-attributed 5.3 Glomerular disease 2.7 Lifetime risk for ESKD: WF 1.8%, WM 2.5%, BM 7.3%, BF 7.8% Kiberd, JASN 2002 AA:EA incidence ratio FSGS 4.5 AIDS nephropathy 20 USRDS, 2007 report 2004-2006 incidence rates, adjusted for gender Hypothesis The increased risk for idiopathic FSGS and HIV-associated collapsing glomerulopathy (HIVAN) among African Americans is due to an African origin genetic variant Assumptions Ancestral populations from Africa, Europe, Asia differ in prevalence of FSGS risk alleles Admixture mapping can find the gene by using SNPs that tag African vs European origin genetic segments Analysis: among cases, the causative gene should be in a genomic region that preferentially came from Africa C22 C22 Cases: Preferentially African segments Controls: African and European segments Admixture mapping in African American FSGS identified a peak of African ancestry: MYH9 ->APOL1 Kopp..Winkler, Nat Genet 2008 Kao…Parekh, Nat Genet 2008 FSGS association S342G, I384M (G1) 180 African American FSGS cases and 205 African American controls. Genovese…Pollak, Science 2010 Tzur…Skorecki, Human Genet 2010 Controlling for rs73885319 (G1) NYK388K (G2) Controlling for G1 and G2 Apolipoprotein L1 Pays..Perez-Morga, Nat Rev Microbiol, 2014 Pore forming Membrane addressing SRA interacting 7 exons, 3 isoforms, 398 – 414 amino acids Component of innate immune system, driven by IFN-a Friedman..Pollak, Kidney Int, 2014 Minor component of HDL subclass 3 Binds phospholipids, induces autophagy Wan..Hu, JBC 2008 The Apolipoprotein L gene family evolved Figure 2 rapidly in primates APOL1 APOL2.1 (Macaque) (Orangutan) Gorilla Human Island Siamang Gibbon Macaque (Baboon #2) (Baboon) APOL4 Baboon Macaque Patas Monkey African Green Monkey Pseudogenes in parentheses Human (Gorilla) (Orangutan) Gorilla Human Chimpanzee Orangutan (Island Siamang Gibbon) APOL7 (Baboon) (Rhesus) APOL3 0.96 1.00 1.00 1.00 1.00 Human Chimpanzee APOL2 Gorilla Kikuyu Colobus Purple-Faced Langur Patas Monkey Baboon Douc Langur African Green Monkey Macaque Hominoids Old World Monkeys New World Monkeys Prosimians 0.1 1.00 APOL6 APOL5 (Lemur) (Macaque) (Baboon) (African Green Monkey) (Douc Langur) (Kikuyu Colobus) Smith and Malik, Genome Research, 2009 (Orangutan) Gorilla Chimpanzee Human Lemur Gorilla Human Chimpanzee Orangutan Island Siamang Gibbon White-Cheeked Gibbon Pygmy Marmoset White-Tufted-Ear Marmmoest Tamarin Squirrel Monkey Owl Monkey Titi Monkey White-Faced Saki Spider Monkey Kikuyu Colobus Douc Langur African Green Monkey Macaque Baboon APOL gene sets vary among primates: A flexible tool kit for innate immuty ✚ Human − Chimpanzee Ψ Gorilla Orangutan Ψ Macaque Ψ Baboon Mouse Serum lytic to T.b.brucei Ψ ✚ Ψ − Ψ − Ψ ✚ − Adapted from Smith and Malik, Genome Res. 2009 APOL1 alleles: G1, red and G2, orange Kopp..Winkler, JASN 2011 Trypanosoma brucei and African Sleeping Sickness T.b.gambiense T.b.brucei T.b. rhodesiense APOL1 is the Trypanolytic Factor of Human Serum Alternate: Plasma membrane cation channel. Thomson, PNAS 2015 Pays..Perez-Morga, Nat Rev Microbiol, 2006 APOL1 is under balancing selection 0 risk allele G0/G0 (WT/WT) 1 risk allele G0/G1 G0/G2 Homozygous disadvantage Heterozygous advantage Trypanosomiasis (African sleeping sickness) Resistance 2 risk alleles G1/G1 G1/G2 G2/G2 Homozygous disadvantage Resistance Chronic kidney disease APOL1 nephropathies Disease/setting Phenotype/ effect size Reference HIVAN OR 29 (US), 89 (SA) Kopp..Winkler, JASN 2011 Kasembeli..Naicker, JASN 2015 FSGS OR 17 Kopp..Winkler, JASN 2011 Arterionephrosclerosis > ESKD OR 7 Lipkowitz..Kopp, KI 2012 Deceased donor genotype -> kidney allograft survival Allograft loss, HR 3.8 Reeves-Daniel..Freedman, Am J Transplant 2011 Recipient genotype -> kidney allograft survival No effect Lee..Chandrakar, Am J Transplant, 2012 Sickle cell Proteinuria, RR 3.4 Ashley-Koch..Telen, Br J Heme 2011 Lupus Collapsing glomerulopathy, OR 5.4 Larsen..Walker, JASN 2013 APOL1 FSGS can manifest clinically as four different mechanistic forms Primary FSGS Adaptive glomerular processes Viral FSGS Drug Associated FSGS Can be steroid responsive Sickle cell disease >CKD (no biopsies) HIVAN OR: US 29 OR: South Africa 89 Interferon therapy Kopp..Winkler, JASN 2011 Ashley-Koch..Telen, Br J Hem 2011 Kopp. .Winkler JASN 2011 Kasembeil..Naicker, JASN 2015 Nichols..Friedman, KI 2014 Can recur after kidney transplant CKD associated with prematurity Unpublished observation Unpublished (CKID, NEPTUNE) APOL1-associated FSGS: sharper incidence peak - spanning ~15-45 yr APOL1 2-risk allele individuals with CKD tend to progress quickly despite conventional therapy: therapeutic need Percent survival 100 80 60 0/1 RA 40 p = 0.001 2 RA 20 0 0 5 10 15 Years since FSGS onset FSGS, NIH Deceased donor transplant, Wake Forest FSGS, Controlled Trial AASK: hypertension Approximate lifetime risks for APOL1 nephropathy ~43 million African Americans ~5 million (~13%) have 2 APOL1 risk alleles Among those, perhaps 20-25% (over 1 million) will develop a renal disease or renal phenotype associated with APOL1 variants FSGS 4% 5 million at-risk individuals: estimated life-time risks HIVAN HA-ESKD 11% OR 17 Lupus CG, ESKD HA-CKD (not ESKD) ? OR 7 Kopp..Winkler, JASN 2011 Lipkowitz..AASK Investigators, Kidney Int, 2012 Dummer..Kopp, Sem Nephrol, 2015 Nephropathy in type 2 diabetics: rapid progression Proposed pathways of APOL1 variant toxicity: mechanisms may lead to targeted therapy NLRP12 suppression NLRP3 activation Cation channels Amplification of TLR4 and IL1R signaling Inflammasome activation G1 and G2 RNA stem loops Protein kinase R activation JNK/MAPK IL-1b Altered endolysomal trafficking and lysosomal function Reduced protein synthesis Podocyte injury & loss