U N -O A
advertisement

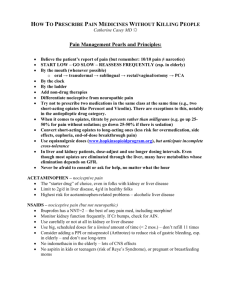
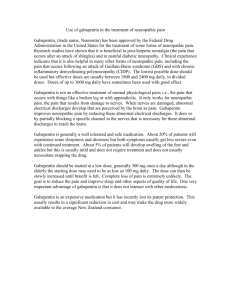
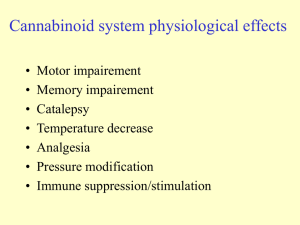
USE OF NON-OPIOID AGENTS AND NEUROPATHIC PAIN Calvin Lui, MD PGY2 February 8, 2014 OBJECTIVES Learn about neuropathic pain and commonly used agents and starting dosages Learn about common agents that address muscle spasm Learn about common agents and modalities that address cancer pain CLINICAL CASE A 70-year-old male with recent diagnosis of multiple myeloma presents to his PCP with pain of his shoulders and back. His back pain has been persistent for the past several months. It has two components: some “running shock-like down to his feet” and other “feeling as if his back is being eaten at.” There is radiologic evidence of bony metastases and DJD. Also, he feels as if his pain tightens on a nightly basis. He has been given 15 mg of MS Contin PO BID, but his pain is still uncontrolled. How would you address his pain. “SHOCK-LIKE” PAIN Likely neuropathic pain Common history items would include radiation from the pain and tingling that he has. NEUROPATHIC PAIN Sympathetically mediated pain- pain arising from a peripheral nerve lesion and associated with autonomic changes Peripheral neuropathic- damage to a peripheral nerve without autonomic change complex regional pain syndrome I and II postherpetic neuralgia, neuroma formation Central pain- abnormal central nervous system (CNS) activity phantom limb pain, pain from spinal cord injuries, and post-stroke pain HISTORICAL CLUES TOWARDS NEUROPATHIC AGENTS Burning, sharp, tingling Possibly dermatomal or stocking-glove Worse with touch May have associated numbness Radiating Possibly associated with Changes in skin temperature/sweating Changes in sensation (itching/numbness) COMMON AGENTS NEUROPATHIC PAIN AGENTS AND COMMON DOSAGES Methadone (opioid with neuropathic facets)- 5 mg PO BID or TID starting Ketamine: I.V.: 0.2-0.75 mg/kg May consider using as long acting and later short acting Larger gun, can be sedating and dissociative Gabapentin (600 mg PO TID or 300 AM/600 Noon/900 PM Be warned about drowsiness, need for weeks for levels to build Reduce to as little as 300 mg daily in renal disease NEUROPATHIC AGENTS CONTINUED Pregabalin (150 mg PO daily with titration up to 300 mg PO daily) Duloxetine: 30 mg PO daily for 1 week, then increase to 60 mg once daily as tolerated. Venlafaxine: 75-225 mg/day; onset of relief may occur in 1-2 weeks, or take up to 6 weeks for full benefit TCAs- nortripyline, desipramine, amytriptlyine Nortripyline- 10-25 mg PO qHS Amytripline- 25 mg PO qHS with titration to 100 mg qHS “SHOCK-LIKE” PAIN REGIMEN Likely neuropathic pain Let’s start Duloxetine 60 mg daily Consider Gabapentin 300 mg TID with titration up to 600 mg TID WHAT ABOUT HIS BACK TIGHTNESS Likely muscle spasm PAIN 2/2 TO MUSCLE SPASM sudden, involuntary contraction of a group of muscles Baclofen: 5 mg PO TID Methocarbamol :1.5 mg PO q6H for 2-3 days Carisoprodol: 250-350 mg PO TID and qHS Diazepam: 5mg q6-8H PRN WHAT ABOUT HIS BACK TIGHTNESS Likely muscle spasm Let’s start him on Baclofen 5 mg TID And now what is left to do is address his pain from his malignancy. PAIN FROM BONY METASTASES Corticosteroids Bone pain 2/2 to cancer Dexamethasone least amount of mineralocorticoid effect typical dosage: 4mg q6H Radiation therapy Bisphosphonates Zolendronate 4 mg IV FINAL PAIN REGIMEN FOR PATIENT Continue with MS Contin 15 mg PO BID Duloxetine 60 mg PO daily Consider gabapentin 300 mg TID with uptitration to 600 mg TID Dexamethasone 4 mg PO q6H Baclofen 5 mg TID Consider Lidocaine patch for localized pain if there is neuropathic pain in the region of the injured wrist Radioablative therapy to spine for extensive mets SUMMARY Different types of pain need to addressed and highlighted in each patient to provide sufficient pain control Many agents exist for neuropathic pain and need consideration of degree of neuropathic pain Bony Metastases may incur their own pain and benefit from corticosteroids and radiation in some cases Consider Muscle spasm as an etiology of pain and know common medications to treat it REFERENCES 1. Dworkin RH, Turk DC, Wyrwich KW, et al. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. The journal of pain : official journal of the American Pain Society. Feb 2008;9(2):105-121. 2. Dworkin RH, O'Connor AB, Backonja M, et al. Pharmacologic management of neuropathic pain: evidencebased recommendations. Pain. Dec 5 2007;132(3):237-251. 3. Chou R, Fanciullo GJ, Fine PG, et al. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. The journal of pain : official journal of the American Pain Society. Feb 2009;10(2):113-130. 4. Hocking G, Cousins MJ. Ketamine in chronic pain management: an evidence-based review. Anesthesia and analgesia. Dec 2003;97(6):1730-1739. 5. Knotkova H, Fine PG, Portenoy RK. Opioid rotation: the science and the limitations of the equianalgesic dose table. Journal of pain and symptom management. Sep 2009;38(3):426-439. 6. van Tulder MW, Touray T, Furlan AD, Solway S, Bouter LM, Cochrane Back Review G. Muscle relaxants for nonspecific low back pain: a systematic review within the framework of the cochrane collaboration. Spine. Sep 1 2003;28(17):1978-1992. 7. Mercadante SL, Berchovich M, Casuccio A, Fulfaro F, Mangione S. A prospective randomized study of corticosteroids as adjuvant drugs to opioids in advanced cancer patients. The American journal of hospice & palliative care. Feb-Mar 2007;24(1):13-19. 8. Saarto T, Wiffen PJ. Antidepressants for neuropathic pain. The Cochrane database of systematic reviews. 2007(4):CD005454. 9. Barakzoy AS, Moss AH. Efficacy of the World Health Organization analgesic ladder to treat pain in end-stage renal disease. J Am Soc Nephrol. 2006;17(11):3198-3203. 10. Dean M. Opioids in renal failure and dialysis patients. J Pain Symptom Manage. 2004;28(5):497-504. 11. Broadbent A, Khor K, Heaney A. Palliation and chronic renal failure: opioid and other palliative medications— dosage guidelines. Progress in Palliative Care. 2003;11(4):183-190(8).