iii ANALYSIS ON THE FLOW AND PRESSURE DISTRIBUTION FOR ACTUAL
advertisement

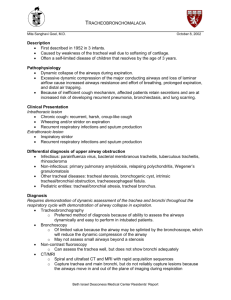
iii ANALYSIS ON THE FLOW AND PRESSURE DISTRIBUTION FOR ACTUAL STENOSIS IN TRACHEA ZULIAZURA BINTI MOHD SALLEH. A project report submitted in partial fulfilment of the requirements for the award of the degree of Master of Engineering (Mechanical) Faculty of Mechanical Engineering Universiti Teknologi Malaysia DECEMBER 2010 iii Sincerely dedicated to Abah, Mama, my fiancée, family members and friends; My all times beloved. iv ACKNOWLEDGEMENT Thanks to Almighty Allah SWT, the most gracious the most merciful, who gave me the knowledge, courage and patience to accomplish this thesis. May the peace and blessings of Allah be upon Prophet Muhammad SAW. To my parents and my family, I love to take this opportunity to say thank you for your entire support trough out this time. Without all of your support, I’m nobody in this world. To the organization that sponsor my scholarship and also my supervisor, Assoc. Prof.Dr. Kahar Osman, here I express my gratitude for all valuable helps, suggestions, advices and continual supervision for the whole period in completing this study. Not to forget my dearest fiancée, who always bear with me and encourage me in finishing my study and guiding my life. A special of appreciation to all my friends and CFM Lab’s members on their willingness to help and teach me when I’m facing trouble along this time. It means a lot to me and I will not forget all your kindness. A credit for my roommate on her thoughtful and consideration on me all this long. Thanks a lot. Finally, for all that involved direct or indirect in my life, thanks for the support that help me to facing any difficulties bravely. v ABTRACT Knowledge of flow inside the human airway is very important for medical practitioner to make accurate diagnosis. With the presence stenosis inside the airway, the flow will be changed significantly and will directly affect the input to the main bronchi. In this study, patient-specific image is used and remodelled using computational fluid dynamic software to simulate the flow within the trachea. The image contains one stenosis which was then reconstructed to other locations. This procedure will enable the study of flow behaviour in the trachea with different stenosis locations. Emphasis of analysis is focused on the flow and pressure distribution along the main airway. For each model, computations were carried out in three different flow rates which are 15 l/min, 60 l/min and 100 l/min corresponding to regular human activity which are resting, normal and heavy excersice breathing, respectively. The results show as stenosis located at the upper third of the trachea, the pressure drop along the trachea are insignificant in every breathing condition but differ to the velocity where the maximum velocity is increase as the flow rate increase. For stenosis located at the lower third or the trachea, both pressure drop and velocity did effect clearly as the flow rate increase. The effect of different location of the stenosis on the velocity distribution along the centerline shows similar increment in every flow rate and the risk in breathing difficulties if the patient having a stenosis at the third location is three times higher compare to the first location if the patient in resting condition. It increases to five times higher when doing the regular activity and eight times higher if the patient doing heavy exercise. The comparison is based on the same size of the stenosis. vi ABSTRAK Pengetahuan berkaitan dengan aliran udara di dalam ruang penafasan manusia adalah amat penting bagi kumpulan perubatan dalam membuat rawatan dan keputusan yang tepat. Stenosis dalam trakea memberi kesan besar terhadap pembahagian input ke bahagian utama bronkus. Dalam kajian ini, imej geometri yang spesifik dari pesakit yang mengalami stenosis digunakan untuk dijadikan model dan dengan menggunakan perisian perkomputeran bendalir dinamik,simulasi aliran udara sepanjang trakea dijalankan. Imej stenosis tersebut kemudiannya di struktur semula ke lokasi-lokasi yang berbeza untuk mengkaji kesan kedudukan lokasi stenosis terhadap sifat-sifat aliran di dalam trakea. Kajian ini tertumpu kepada taburan aliran dan juga tekanan sepanjang ruang utama pernafasan manusia. Simulasi di jalankan dengan menggunakan tiga kadar aliran yang berbeza iaitu 15 l/min, 60 l/min dan juga 100 l/min. yang mewakili aktiviti harian manusia: keadaan rehat, normal dan juga ketika melakukan senaman berat. Hasil daripada kajian menunjukkan sekiranya stenosis berada di bahagian atas trakea, perubahan tekanan sepanjang trakea mengalami perubahan yang kecil bagi setiap kondisi pernafasan tetapi kelajuan maksimum aliran meningkat sekiranya kadar aliran input meningkat. Bagi stenosis di bahagian bawah trakea, peningkatan kadar aliran menunjukkan efek yang ketara ke atas perubahan tekanan dan juga halaju aliran. tetapi bagi taburan halaju sepanjang trachea, ianya memberikan paten yang hampir sama bagi setiap kedudukan stenosis. Akhir sekali, risiko dalam pengalami kesukaran bernafas adalah tiga kali lebih tinggi bagi pesakit yang mengalami stenosis di bahagian bawah berbanding atas jika pesakit dalam keadaan rehat, lima kali lebih berisiko dalam keadaan normal dan lapan kali lebih berisiko sekiranya melakukan senaman berat. vii TABLE OF CONTENT CHAPTER 1 TITLE PAGE DECLARATION ii DEDICATION iii ACKNOWLEDGEMENT iv ABSTRACT v ABSTRAK vi TABLE OF CONTENTS vii LIST OF TABLES x LIST OF FIGURES xi LIST OF SYMBOLS xiii INTRODUCTION 1.0 Overview 1 1.2 Objectives 2 1.3 Scope 3 viii 2 3 4 LITERATURE REVIEW 2.1 Overview of human respiratory system 4 2.2 Trachea 5 2.3 Trachea stenosis 7 2.4 Trachea stenosis effect to velocity and pressure distribution . 9 2.5 Effect of the stenosis location to the flow characteristic 9 2.6 Actual modeling 10 2.7 Current study 12 METHODOLOGY 3.1 Introduction 13 3.2 Simulation model 14 3.3 Boundary Condition 17 3.4 Governing Equations 19 3.5 K-ε turbulent model 20 3.6 Summary of the methodology throughout the process 21 RESULT AND DISCUSSION 4.1 Overview 22 4.2 Velocity distribution 23 4.3 Pressure Distribution 26 4.3.1 Risk due to location of stenosis. 29 ix 5 CONCLUSION 33 REFERENCES 36 APPENDIX A 38 APPENDIX B 39 APPENDIX C 43 x LIST OF TABLE TABLE NO 3.1 TITLE Parameters at all trachea model for three different breathing conditions PAGE 18 xi LIST OF FIGURES FIGURE NO TITLE PAGE 2.1 Respiratory system 5 2.2 Trachea and major bronchi of the lungs 6 2.3 Normal bifurcation (Zuhairi, 2009) 7 2.4 Obstructive airway (Zuhairi, 2009) 8 2.5 Tracheal stenosis 8 2.6 Suggested location for tracheal stenosis 10 (Freitag et al.(2007), A proposed classification system of central airway stenosis, European Respiratory Journal) 2.7 Example of trachea model without stenosis. 11 (a) actual model (b)simplified model 3.1 Four separate model of trachea and main bronchi 15 xii 3.2 3D model of the whole respiration system reconstructed 16 from CT-scan images 3.3 (a) Actual trachea model extract from the whole respiration 17 system (b) Actual trachea model ready to be simulated 4.1 Central velocity distribution of each model in Q=15 l/min 23 4.2 Central velocity distribution of each model in Q=60 l/min 24 4.3 Central velocity distribution of each model in Q=100 l/min 24 4.4 Central pressure distribution of each model in Q=15 l/min 26 4.5 Central pressure distribution of each model in Q=60 l/min 27 4.6 Central pressure distribution of each model in Q=100 l/min 28 4.7 Range of P/Po between inlet and bifurcation area for each 30 location of stenosis and flow rates 4.8 Risk of stenosis for every location and flow rate 31 xiii LIST OF SYMBOLS SYMBOLS A area C velocity of sound E total energy g local acceleration of gravity L length Re Reynolds number Q volume flow rate U mean velocity D diameter ρ density xiv v kinematic viscosity P pressure P0 stagnation pressure μ viscosity V velocity V0 stagnation velocity l liter min minute 1 CHAPTER 1 INTRODUCTION 1.0 Overview The flow in the bifurcating lung airway is one of the most basic and revealing problems in the general case of the breathing physiology. It influence drug particle delivery patterns, pollution dispersion and so on that related to respiration system. These days, the flow inside the human airways is gaining attraction to the researchers to choose as a subject of study either doing by experimental or numerical method. In fact, human airways flow studies have been carried out by many researchers previously to provide the solution especially for breathing problems. Due to the advanced development in the computational capability and computerized tomography (CT-scan), it offers an alternative to study a physically realistic model for the human airways. Basically, human anatomy and the respiration process are converted into simulation to understand its behaviour in the airway flow. However, knowledge of the airflow mechanism within the airways is the first thing that 2 needs to take into account before proceed the study. This is where the CFD tools were come as the handy tools where the characteristic and the condition that happen inside the human airways can be simulate and presented. The airways networks has quite small dimension and it is difficult to retain dynamic similarity to the physical model. Therefore, most of the studies were limited up to third generations. But the most crucial part that needs to be considered is the main trachea where it plays as a main vessel for the air to reach the lung in respiration process. If happen any obstruction in this area, it can lead to problems in breathing compared to if the obstruction happens in one of the airways networks (right or left side) since human still can survive if one side of the network is blocked. In this study, the actual model of the trachea diseases patients will be used to obtain the flow characteristic inside the human lung. The result then not only can aid the medical team by providing the solution for treatment but also can initiate to the new technology for medical instruments. 1.2 Objectives The objective of the study is to determine the effect of stenosis in different locations in trachea to the flow and pressure distribution. 3 1.3 Scope a) Actual image will be used b) Numerical modeling will be use for analysis c) Effect of the stenosis location will be considered 4 CHAPTER 2 LITERATURE REVIEW 2.1 Overview of human respiratory system Respiratory system is one of the essential systems for all organisms and the function of this system is to allow gas exchange to all parts of the body. Each cell in the body will receive the oxygen (O2) and release the carbon dioxide (CO2). The structure of the gasses exchange or the anatomy of the respiratory system is different depending on the organisms. For human, the respiratory system can be separated into two major parts which is an upper respiratory region and the lower respiratory region. The upper respiratory region comprises the nasal passages, pharynx, and the larynx while the lower respiratory region includes the trachea, the primary bronchi and lungs. Lungs and linked blood vessels deliver oxygen to entire body and remove carbon dioxide from the system. Normally, the left lung is smaller than the right lung as heart is located in the right lung region. 5 Figure 2.1 Respiratory system (www.lakesidepress.com, 2008) 2.2 Trachea Trachea is the tube that connects mouth and nose to lungs. It located in the front of neck and the end of the larynx. The trachea has rings called cartilages for support and it is similar to the rings in the vacuum cleaner host. The air will passes through the trachea while the food and drink go down a different tube called esophagus which located behind the trachea. 6 The larynx goes directly into the trachea or the windpipe. For adult, the trachea is a tube approximately twelve centimeters in length and two point five centimeters wide. The trachea is kept open by rings of cartilage within its walls. Similar to the nasal passages, the trachea is covered with a ciliated mucous membrane which brushes debris up and out. This tissue destroyed by smoking but can regenerate if the person stops smoking. At the end of trachea, it divided into two main bronchi (left and right), one to each lung. Figure 2.2 Trachea and major bronchi of the lungs (Encyclopedia Britainnica,Inc,2008) 7 Figure 2.3: Normal bifurcation (Zuhairi, 2009) 2.3 Trachea stenosis Breathing difficulties can be caused by many factors. One of the factors is the restriction of the main trachea. This restriction will alter the flow path of the inhaled and exhaled air and subsequently change the behavior inside the trachea. Therefore, it is important to understand the changes of the flow behavior along with the pressure distribution with respect to the presence of stenosis or obstruction in the trachea. Spittle (2000) suggested that tracheal stenosis presents as shortness of breath and the symptoms do not usually occur at rest until the trachea has stenosed to 30% of its original size. Yang (2007) has shown that long-segment stenosis due to congenital factor is very critical especially for infants and showed that the removal of the stenosis managed to remove the breathing problem. Hammer (2004) recommended that correct 8 diagnosis will need additional information in order for medical practitioners to perform proper diagnosis. Figure 2.4: Obstructive airway (Zuhairi, 2009) Figure 2.5: Tracheal stenosis (source from www.bidmc.org, accessed on 3rd of November 2009) 9 2.4 Trachea stenosis effect to velocity and pressure distribution. Apart from understanding the flow, another critical factor that is affected by the presence of stenosis is the pressure distribution. Brouns (2006) have completed an extensive numerical study on the pressure drop along the trachea. Brouns used artificial stenos in his study where the stenos were patched to a healthy airway. The model was in three-dimensional. Brouns results showed that the overall pressure drop at rest was only affected in case of severe constriction. The results also hinted that the pre-critical stage can be detected using the computed pressure drop The effect of the increasing size of the stenosis also was investigated by Jayaraju (2006) in their research and they found out that the pressure drop shows modest increases with the degree of narrowing up to 75% constriction. On the other hand, Cebral (2004) research showed decreased pressure and increased shear stress in the region of a stenosis besides an increased flow velocity during inspiration. 2.5 Effect of the stenosis location to the flow characteristic Moreover, the locations of the tracheal stenosis vary from patients to patients. Freitag (2007) suggested five common locations of tracheal stenosis. Other researchers have chosen locations around these three sections first section which is upper, middle and lower third of the trachea. Jayaraju (2006) modeled the flow for patient-specific case where the location of the tracheal stenosis is at the upper third of the trachea only. However, Lam used a model of trachea stenosis at the lower third of the trachea to assess the accuracy of three-dimensional (3D) CT-image scan and virtual bronchoscopy. The 10 purpose was to apply the knowledge to the treatment for infants and children that having the tracheoesophageal fistula and tracheal stenosis. But no flow analysis was done. Figure 2.6: Suggested location for tracheal stenosis (Freitag et al.(2007), A proposed classification system of central airway stenosis, European Respiratory Journal) 2.6 Actual modeling While many researchers use simplified geometry of the trachea, there are many others who use patient-specific images to study the flow inside the trachea. Both 11 geometries have different advantages and disadvantages. The importance of using actual images as a model to study the flow pattern in the trachea with stenosis is very crucial. Some researchers used simplified model to obtain the flow conditions. However, Russo (2008) confirmed that the effect of cartilage rings increased with increased flow rate in the trachea. Therefore, by using actual images, the effect of this cartilage rings will be imbedded in the flow study Figure 2.7: Example of trachea model without stenosis. (a) actual model (b)simplified model Detailed patient-specific flow pattern using actual image was also obtained by Choi (2006) where flow separation due to sudden change in diameter was observed in the main trachea. Another actual image flow model studied by other researchers such that completed by Lin (2007) where turbulence induced by the laryngeal jet was shown to affect the airway flow pattern significantly. Sun and Yu (2007) claimed that using the 12 actual images, the models precisely preserve the original configuration and the results of the pressure and velocity distributions in the airflow field are accurately determined. It shows that pressure gradients of airway are lower for the healthy person and the airflow distribution is quite uniform in the case of free breathing. Further study regarding the flow using an actual model conducted by Gemchi (2007) demonstrated that the nature of the secondary vortical flows which develop in such asymmetric airways varies with the specific anatomical characteristics of the branching conduits. 2.7 Current study In this study, the effect of several locations of the stenoses to the air flow inside the trachea is investigated. Three locations of stenoses were chosen, namely upper, middle and lower third of the trachea. These choices follow the suggestion by Freitag (2007). This study will show the effect of these locations to the pressure drop as the flow enters the bifurcations. Critical stenos location such as near the bifurcation is also expected to alter the flow rates into the bifurcation which is one of the major contributions of this study. Actual images from CT scan were obtained and conversion to numerical modeling was made. The numerical study of the flow was then presented. 13 CHAPTER 3 METHODOLOGY 3.1 Introduction To achieve the objective of the study, several steps were used in order to accomplish the good results. In this study, one of the Computational Fluid Dynamics (CFD) software called Engineering Fluid Dynamics is used. This software simulates the flow inside the human airways using the actual model. Before the model can be simulating, it previously has been prepare using the Mimics software to get the actual geometry inside the human airways. Using several boundary conditions, the actual model then has been simulate using a few different flow rate to get the result of the flow characteristics inside the human airways. The details will be described in this chapter. 14 3.2 Simulation model There are two option of model that can be used to simulate the flow inside the human airways. One is using the simplified model where the model is draw back using the same geometry as the actual airways. But, due to the complexity of the actual human airway geometry, usually it will be simplified into the symmetric or asymmetric model (Luo,X.Y el at ,2004, Russo. J et al, 2008). The other option is using the actual model where it been processes from the CTscan images. The results from the analysis using the geometry of the scan-based have verified their consistency with measures from previous anatomic studies (Tawhai, M.H. et al, 2004). The actual complexity of the human trachea geometry and the location of stenosis inside the trachea did influence the accuracy of the distribution in velocity and pressure inside the human airways. To compare the difference that occurs in each circumstance, four separate tracheas and main bronchi models were created anatomically: (a) a healthy model without stenosis and (b) three other models with different locations of stenosis along the trachea (Figure 3.1). To evaluate the result from each model side by side, the major geometries were retained for every model and only the stenosis area were manipulate to create the other models. Toward reconstruction of the CT models, a few steps need to be done. 155 Stenosis locationns (ii)Model no.1 (ii) Model M no.2 (iii)Modeel no.3 (iiv)Model no o.4 H Healthy moddel Stenosiis location 1 Stenosis location 2 Stenosis location 3 Figure 3.1 Four sep parate mod del of trach hea and maain bronchii ges from onee Thhe models arre based onn the Compuuted Tomoggraphy (CT)) scan imag Chinese addult male patient, 60 years old as the referencce stenosis m model (Figu ure 3.1 (ii))). The locatiion of the sttenosis is loocated at thee upper thirrd of the trachea. The stenos s of thee same moddel then haad been rem moved to generated g thhe healthy model andd artificiallyy relocated aat different locations for f the other two stenoosis (Figure 3.1 (iii and d iv)) wheree the locatioon is at thee middle annd lower thhird of the trachea ass suggested d by Freitagg (2007). The CT scan n images weere taken in the axial pllane with a resolution r of o 512 x 5122 kness of 1mm m. AMIRA A, one of thee conversion software was used too pixels andd slice thick convert thhe CT-scann images thhat in the D DiCom form mat into soolid three dimensiona d al models. Smoothing S of the surfface was peerformed too eliminatee the rough hness of thee curves cauuse by partiaal volume effects, e Spirrka (2005). 16 To extract the respiration model image and to remove other unrelated region that comprise in the CT-scan images taken, threshold separation range in between -1024 and -500 was used to get the air region. Then the respiration model was obtained by using region growing function where the voxels within the airway lumen were identified. Figure 3.2: 3D model of the whole respiration system reconstructed from CT-scan images The model then went through the cutting and removing process to separate the other respiration organs until only trachea and main bronchi remain as the solid model. The completed model then underwent the 3D calculation after the Morphology and Boolean operation where the anatomical wall created. Next, the model been export to another software package called MAGICS. Here, major alteration such as removing and relocating the stenosis, geometries correction and holes patching been done. Refined model is then saved in ASCII STL format and the numbers of faces are reduced to 15000 17 7 d to limittation of thee EFD softw ware that beeen used to simulate s thee faces usingg AMIRA due model. (a) (b) Figure 3.3: (a) Acctual tracheea model exxtract from m the wholee respiration system (b b) Actual trrachea mod del ready too be simulaated 3.3 Booundary Coondition Byy using SOL LIDWORK K 2008 softw ware, the STL S formatt model waas converted d into SLDP PRT formatt and the bo oundary conndition for every inlet and outlet are defined d. Flow ratess defined in n each cases are comp puted based on flow paartition ratio on given by y 18 Horsfield where 55% of inlet flow rates diverges into right bronchus while the other 45% to the left bronchus. The condition imposed on the inlet and outlets are summarized in Table 3.1. Table 3.1 Parameters at all trachea model for three different breathing conditions Parameter Incompressible flow Flow rate (l/min) 15,60 and 100 Inlet Pressure 101325 Pa Density 1.225 kg/m3 Viscosity 1.7894e-05 kg/ms-1 The wall model is assumed as smooth and rigid wall due to the realistic condition inside the trachea where the wall is covered with cilia and mucus which tends to make the wall area smooth and the cartilage rings that support the trachea makes the trachea rigid. In addition, the flow inside the human lung airway is taking as non-slip condition and the air was assumed to be a homogeneous. Besides, due to the speed of air taken is slower than the speed of sound, the air is assume as incompressible flow and the temperature together with density are constant (Luo,X.Y el at, 2004). M = V/C where: V = velocity of flow C = velocity of sound 19 3.4 Governing Equations Same as other fluid flow simulation, the following equations were applied to the actual human airways model. It is based on the Navier-Stokes equation. Continuity equation 0 Momentum Equations Reynolds Number The equation use to determine the flow type whether it is laminar or turbulent. The parameter that used to determine the Reynolds Number are density, ρ, velocity, u, length of flow, D and viscosity of the fluid, μ. 20 3.5 K-ε turbulent model In the CosmosFloWork software, there are built in K-ε turbulent model which is used to analyze the turbulent case. For turbulent kinetic energy k, For dissipation e, 2 where the value constants are; 1.44, 1.92, 1.0, 1.3 21 3.6 Summary of the methodology throughout the process CT scan data • Get the CT-scan data of the trachea patient from hospital. Process the data to built the actual model • Raw CT-scan data reconstruct using Mimics software to rebuilt the actual trachea model. • Preparing the actual model and export to Solidworks software. • From solidworks, choose CosmosFloWorks to run the simulation after fill in all the parameters and boundary condition Getting the results • Process the results obtain for better presentation 22 CHAPTER 4 RESULT AND DISCUSSION 4.1 Overview Using Engineering Fluid Dynamics software, all models then been simulated. The result shown in this study comprises the data from the healthy and also three other stenosis trachea models. The purpose is to study the effect of the stenosis in the different location (upper, middle and lower third of trachea) in flow characteristic and pressure distribution in human airways. The results of the simulation will be cover for three different values of flow rates which are 15 l/min, 60 l/min and 100 l/min. Besides, the risk in breathing problem due to the stenosis and stenosis location will be discuss in this chapter. 23 4.2 Velocity distribution The asymmetrical geometries of the trachea that was extracted from the CT-scan are contributes to the complexity of the flow pattern inside the human airways. This creates the imbalanced flow rate distribution all the way through the bronchus. Figure 4.1, Figure 4.2 and Figure 4.3 shows the influence of the stenosis location and the flow rate induced at the inlet to the velocity distribution along the human airways. It illustrated the comparison between the healthy models with the other three models with different location of stenosis for three values of flow rates represent the resting activity, regular activity and heavy exercise. Graph V/Vo vs Length for Q15 Healthy Trachea Stenosis Trachea 1 Stenosis Trachea 2 Stenosis Trachea 3 4 3.5 3 V/Vo 2.5 2 1.5 1 0.5 0 0 0.02 0.04 0.06 0.08 0.1 0.12 0.14 m Figure 4.1: Central velocity distribution of each model in Q=15 l/min 24 Graph V/Vo vs Length for Q60 Healthy Trachea Stenosis Trachea 1 Stenosis Trachea 2 Stenosis Trachea 3 4 3.5 3 V/Vo 2.5 2 1.5 1 0.5 0 0 0.02 0.04 0.06 0.08 0.1 0.12 0.14 m Figure 4.2: Central velocity distribution of each model in Q=60 l/min Graph V/Vo vs Length for Q100 Healthy Trachea Stenosis Trachea 1 Stenosis Trachea 2 Stenosis Trachea 3 4 3.5 3 V/Vo 2.5 2 1.5 1 0.5 0 -0.02 0 0.02 0.04 0.06 0.08 0.1 0.12 0.14 m Figure 4.3: Central velocity distribution of each model in Q=100 l/min 25 The flow enter the inlet of the trachea as the flow rates induced and having almost the same pattern for each cases where the stenosis located at the different location. After that it starts to accelerated at the stenosis area for each models with stenosis except for the healthy model due to the existing constriction of the crosssectional area. For the first location of stenosis, the gap between the patterns of the velocity throughout the trachea is almost the same as the healthy model except at the stenosis area for each flow rates used at the inlet. The velocity flow speeds up at the stenosis area and slows down just about the same pattern again as the healthy model before it reach the branches where the flow divided into right and left bronchi. It is different with the second and the third location of the stenosis. The result shows a huge different in velocity of the flow after downstream the stenosis area compared to the healthy model. Distance between the stenosis and bifurcation area and the localized disturbance originated at the geometries features such as the curvenature etc leads to dissimilar flow pattern. Since of the length between the stenosis and the bifurcation area for the second stenosis is shorter than the first but longer than the third location, some transformation on the velocity distribution still appears after the stenosis area but it is still not enough to reduce the velocity before it reach the inlet of the branches. Same situation applies o the third location but in this case, the velocity of the flow is still in high speed when it reaches the bifurcation area and it significantly influences the distribution of the flow rate to each bronchus, left and right. Overall, the velocity patterns for every case it not changing radically every time the flow rate is changed. The lower stenosis results in the biggest velocity difference at the bifurcation area as compared to that of the healthy model followed by the middle and the upper stenosis location. 26 4.3 Pressure Distribution The following figures show the pressure distribution from the inlet at the top of the trachea to the outlet at both right and left bronchi for every models and flow rates. The lines plotted represent the pressure at the centerline of the studied model. It can be seen that pressure drop is increasing as the flow passes through the stenosis area. The value of the pressure drop is neglected and only the pattern of the characteristic is emphasized in this study. Therefore, the graphs plotted in dimensionless unit for each models and flow rates. 1.001 P/Po Graph P/Po vs Length for Q15 1.0005 1 0.9995 0.999 0.9985 0.998 0.9975 0.997 0.9965 Healthy Trachea Stenosis Trachea 1 Stenosis Trachea 2 Stenosis Trachea 3 0.996 0.9955 0.995 0.9945 m 0.994 0 0.02 0.04 0.06 0.08 0.1 0.12 Figure 4.4: Central pressure distribution of each model in Q=15 l/min 0.14 27 7 d lenngth measurred from the inlet. For the stenosiss Eaach stenosis located at different located at the upper third t of the trachea, the distance of o the stenoosis is appro oximately at a 37mm from the inlet. The secon nd and the third t locatio on were aroound 57mm m and 87mm m w generatted from thee same sourrce, the bifu urcation areaa respectiveely. Since alll models were calculated d from the in nlet is the saame and it is i around 11 10 mm from m the inlet. From F Figuree 4.4, it can n be seen th hat the low w flow rate, 15 l/min that t is impo osed at the inlet of thee trachea do oes not show w a significcant effect w when the lo ocation of thhe stenosis s changing g. The pressu ure drop alo ong the tracchea are so small for each e model of the sten nosis tracheaa compared to the healthy modeel even thee location of the stennosis is neearer to thee bifurcation n area. Theerefore, the patient diaagnosed witth stenosis in the trach hea will no ot have a breeathing prob blem when they t in restiing conditio on. 1.001 P/Po Graph P/Po vs Leength for Q60 Q 1.0005 1 0.9995 0.999 0.9985 0.998 0.9975 0.997 0.9965 Healthy Traachea Stenosis Traachea 1 Stenosis Traachea 2 Stenosis Traachea 3 0.996 0.9955 0.995 0.9945 m 0.994 0 0.02 2 0.04 0.06 0.08 0.1 0.1 12 0.14 Figgure 4.5: Central C presssure distriibution of each e modell in Q=60 l//min 0.16 28 8 ure 4.5, thee effect of th he differentt stenosis loocations to the t pressuree Ass of the Figu along the trachea staarted to sh how clearly when the flow rate stimulated at the inleet increase too 60 l/min. Pressure drrop betweenn the inlet an nd the bifurrcation areaa for the firsst location of the stenossis illustratees a small difference d ass comparedd to the seco ond location n of the sttenosis evaaluated with h the heallthy modell. The diffference beccome moree significantt when the same flow w rate inducced at the inlet of thee third locaation of thee stenosis where w the lo ocation is nearest n to th he bifurcation area aree compared against thee other two stenosis mo odels. This circumstannce happenss for the reaason that the differencee in distance between the stenosiss with the bbifurcation area did afffect the prressure afterr hrough the stenosis. s Ass for stenosee located at the upper tthird of the trachea, thee passing th length bettween the sttenosis and d the bifurcaation area is i long enouugh for the pressure to o rise back after a passin ng through the t stenosiss area. So, as a the lengthh shortens, the chancess for the preessure to inccrease are lo ower. It lead ds to the hig gher pressuure drop for the stenosiss located neearer to the bifurcation. b P/Po 1.0 001 1.00 005 1 0.99 995 0.9 999 0.99 985 0.9 998 0.99 975 0.9 997 0.99 965 0.9 996 0.99 955 0.9 995 0.99 945 0.9 994 -0.02 Graph P P/Po vs Len ngth for Q1100 Healthy Trachea Stenosis Trachea 1 Stenosis Trachea 2 Stenosis Trachea 3 m 0 0.02 0.04 0 0.06 0.08 0..1 0.12 2 Figgure 4.6: Ceentral presssure distrib bution of each model in Q=100 l/min l 0.14 29 The flow rate then increase to 100 l/min and the result in pressure distribution along the trachea are plotted as in figure 3 (c). As seen in the figure, the pressure drop between the inlet and the bifurcation in all models is higher as compared to the 15 l/min and 60 l/min flow rates. Although the first stenosis location shows a bigger pressure drop compare to the previous flow rates, the second and the third location illustrate more significant differential when the flow rate increases. Moreover, the complex geometries that comply in the models structure also influence the pressure drop along the trachea due to the curvature, angle etc. It follows the Bernoulli and Continuity equations. As a result, if the stenosis located at the first location, the pressure drops is still not so severe even if the flow rate increases. It is because, the distance of the stenosis is far from the bifurcation and it give the pressure enough time to regain the approximate original value as before it undergoes the stenosis area. However, for the second and the third location, severe pressure drop is shown as the flow rate increase and it indicate the risk to the breathing problems. The pressure distributes to both right and left bronchi are at the lower state due to this higher pressure drop. 4.3.1 Risk due to location of stenosis. Figure 4.7 shows the differences between the inlet and bifurcation area of P/Po at every location of stenosis and also for every flow rates that induced at the every inlet of the model. The values plotted taken from the proximal of the trachea to the bifurcation area. From the figure, as the location of the stenosis located nearer the bifurcation area, the range of the maximum and minimum P/Po is increasing. This increment shows that the pressure drops is higher as the location is nearer to the bifurcation area. As the result, the difficulty in breathing problem will also increase as the pressure drop higher. 30 The graph also shows that, the difference in pressure drop is more significant when the flow rates increase and the stenosis that is nearer to the bifurcation area is the most affected as the flow rates changes. It can be used to indicate the risk in breathing problems for patient that is diagnosed with stenosis inside the trachea. ΔP/Po (P/Po imlet - P/Po bifurcation area) Range of P/Po between inlet and bifurcation area for each location of stenosis and flow rates 0.0045 0.004 0.0035 0.003 0.0025 HEALTHY 0.002 STENOSIS 1 0.0015 STENOSIS 2 0.001 STENOSIS 3 0.0005 0 0 15 30 45 60 75 90 105 120 Flow rates, Q (l/min) Figure 4.7: Range of P/Po between inlet and bifurcation area for each location of stenosis and flow rates Using the data plotted in Figure 4.7, the risk indicator for stenosis effect as the location located nearer to the bifurcation is calculated. The data from the range of pressure drop between the inlet and bifurcation area (ΔP/Po) for each model then been compared to the healthy model to obtain the different risk between the health condition and the condition with several location of stenosis. Hence, the effect of the stenosis can been group as severe or mild to the respiratory system. 31 Risk of stenosis for every location and flow rate 0.003 0.0025 ΔP/Po 0.002 Healthy 0.0015 Stenosis #1 0.001 Stenosis #2 Stenosis #3 0.0005 0 0 20 40 60 80 100 120 Flow rate, Q (l/min) Figure 4.8: Risk of stenosis for every location and flow rate Next, the risk effects from stenosis at every location were plotted in Figure 4.8. As of the graph illustrate, the healthy model did not have any difficulty even if the person having a heavy exercise. However, the first location of the stenosis start to show the effect of the stenosis when the flow rate increase compared to the healthy model but the risk is still low since the difference compared to the healthy is small. For the second location of the stenosis which is at the middle third of the trachea, the risk is mild for the lower flow rate but rise for heavy activity. It can be dangerous for several patient based on their condition. For both first and second location, the patient possibly need only inhaled type of treatment and can avoid the dissect treatment. In contrast with the third location of the stenosis, the regular activity already caused severe risk to appear and patient with this location of stenosis maybe need stent as the solution for their breathing problems. 32 Thus, the utmost risk for breathing problem emerges when the stenosis is located at the lower third of the trachea and the patient doing heavy exercise where the air flow rate that going into the airways is around 100 l/m. The pressure gradient in this case is the highest compare to others cases. 33 CHAPTER 5 CONCLUSION The airflow within patien specific geometry of human airway derived from CTscan image is numerically studied using the Engineering Fluid Dynamics (EFD) software. The flow and pressure distribution as well as the characteristics all through the trachea are examine in details in this study. Using different models those represent healthy and other stenosis models with different stenose location, several conclusions are drawn. The results obtain using the CT-scan images shows more complicated flow pattern and also higher in pressure drop compared to the simplified model. This is due to the complexity of the geometries of the model and also the branching angle of the bronchus at the end of the bifurcation area that leads to the uneven pattern in velocity and pressure distribution in every model. From these results, it is confirmed that every patient will results in different pattern of the flow characteristic due to the different geometries of their trachea. 34 Then, when the stenosis is added to the healthy trachea, the flow pattern illustrated in the results show the disturbance especially at the stenosis area and also at the bifurcation area compared to the healthy model. The velocity started to increase where the stenosis located and reduce back before reach at the branches for the stenosis model results. The differential is more significant when the location of the stenosis is relocated at another two location where the stenosis positioned nearer to the bifurcation region. As the risk indicator plotted, the consequences for the different flow rates induced at the inlet are emphasized. It show that, stenosis at the upper third of the trachea, if the flow rates increase from 15 l/min to 100 l/min, it still can be consider as mild breathing problem because the pressure drop between the inlet and the bifurcation area is small and approximately similar to the healthy model. For the other two location of the trachea, the flow rates used at the inlet did affect the respiration flow significantly and it leads to the breathing problems. For some cases, if the patient that diagnoses with this kind of stenosis, it can be categorized as the severe breathing problems because the pressure drop at the branches is higher and it did influence the distribution of flow to both two bronchi, left and right. : As a conclusion, the results can be summarizing as follows: 1. As stenosis located at the upper third of the trachea, the pressure drop along the trachea are insignificant in every breathing condition but differ to the velocity where the maximum velocity is increase as the flow rate increase. 2. For stenosis located at the lower third or the trachea, both pressure drop and velocity did effect clearly as the flow rate increase. 35 3. The effect of different location of the stenosis on the velocity distribution along the centerline shows similar increment in every flow rate. 4. The risk in breathing difficulties if the patient having a stenosis at the third location is three times higher compare to the first location if the patient in resting condition. It increases to five times higher when doing the regular activity and eight times higher if the patient doing heavy exercise. The comparison is based on the same size of the stenosis. 36 References 1. Brouns, M., Jayaraju, S. T., Lacor, C., Mey, J. D., Noppen, M., Vincken, W., et al. (2007). Tracheal stenosis: a flow dynamics study. J Appl Physiol , 102: 1178-1184. 2. Calay, R. K., Kurujareon, ,. J., & Holdo, A. E. (2002). Numerical Simulation of Respiratory Flow Patterns within Human Lung. Elsevier , 130:201-221. 3. Cebral, J., & Summers, R. (2004). Tracheal and central bronchial aerodynamics using virtual bronchoscopy and computational fluid dynamics. Medical Imaging , 8:1021 1033. 4. CHOI, L.-T., & TU, J. (2007). FLOW AND PARTICLE DEPOSITION PATTERNS IN A REALISTIC HUMAN DOUBLE BIFURCATION AIRWAY MODEL. Fifth International Conference on CFD in the Process Industries , 19:117–31. 5. Freitag, L., Unger, M., Ernst, A., Kovits, K., & Marquette, C. (2007). A proposed classification system of central airway stenosis. European Respiratory Journal . 6. Gemci, T., Ponyavin, V., Chen, Y., Chen, H., & Collins, R. (2007). CFD Simulation of Airflow in a 17-Generation Digital Reference Model of the Human Bronchial Tree. Biomechanics . 7. Guan, X., & Martonen, T. B. (2000). FLOW TRANSITION IN BENDS AND APPLICATIONS TO AIRWAYS. J. Aerosol Sci , 31: 833-847, . 8. Hammer, J. r. (2004). Acquired upper airway obstruction. PAEDIATRIC RESPIRATORY , 5:25–33. 9. Heged´us, C. J., Balásházy, I., & Farkas, Á. ( 2004). Detailed mathematical description of the geometry of airway bifurcations. Respiratory Physiology & Neurobiology , 141:99– 114. 10. Jayaraju, S. T., Brouns, M., Lacor, C., Mey, J. D., & Verbanck, S. (2006). EFFECTS OF TRACHEAL STENOSIS ON FLOW. European Conference on Computational Fluid Dynamics . 37 11. Lam, W. W.-m., Tam, P. K., Chan, F.-L., Chan, K.-l., & Cheng, W. (2000). Esophageal Atresia and Tracheal Stenosis:Use of Three-Dimensional CT and Virtual Bronchoscopy in Neonates, Infants, and Children. American Roentgen , 174:1009–1012. 12. Lin, C.-L., Tawhai, M. H., McLennanc, G., & Hoffmanc, E. A. (2007). Characteristics of the turbulent laryngeal jet and its effect on. Respiratory Physiology & Neurobiology , 157:295–309. 13. Luo, X. Y., Hinton, J. S., Liew, T. T., & Tan, K. K. (2004). LES Modeling of Flow in a Simple Airway Model. Medical Engineering and Physics . 14. Russo, J., Robinson, R., & Oldhamb, M. J. (2008). Effects of cartilage rings on airflow and particle deposition in the trachea and main bronchi. Medical Engineering & Physics , 30: 581–589. 15. Spittle, N., & McCluskey, A. (2000). Tracheal stenosis after intubation. PubMed Central , 321(7267): 1000–1002. 16. Yang, J. H., Jun, T. G., Sung, K., Choi, J. H., Lee, Y. T., & Park, P. W. (2007). Repair of Long-segment Congenital Tracheal Stenosis. J Korean Med Sci , 22: 491-496. 38 APPENDIX A Title/Week Project Plan Literature Review Mimics Tutorials Model Development Initial Simulation Analysis results Draft Preparation Slide Preparation Title/Week Project Plan Models development Simulation Analysis results Draft Preparation Paper preparation Slide Preparation Gantt Chart for Master Project 1 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Gantt Chart for Master Project 2 1 2 3 4 5 6 7 8 9 10 11 12 13 14 39 APPENDIX B Velocity and Pressure Contour along Trachea Velocity Q15 Healthy Model Stenosis #1 Stenosis #2 Stenosis #3 40 Q60 Healthy Model Stenosis #1 Stenosis #2 Stenosis #3 Q100 Healthy Model Stenosis #1 Stenosis #2 Stenosis #3 41 Pressure Q15 Healthy Model Stenosis #1 Stenosis #2 Stenosis #3 Stenosis #1 Stenosis #2 Stenosis #3 Q60 Healthy Model 42 Q100 Healthy Model Stenosis #1 Stenosis #2 Stenosis #3 43 APPENDIX C 44 Simulation of stenosis effect on airflow pattern in trachea and main bronchi Z.M.Salleh1, N.H.Johari2, K.Osman, Juhara, Rafiq 1 Faculty of Mechanical and Manufacturing Engineering, Universiti Tun Hussein Onn Malaysia, 86400 Batu Pahat,Johor Malaysia E-mail : zulia@uthm.edu.my 2 Faculty of Mechanical Engineering Universiti Malaysia Pahang 26600 Pekan, Pahang Malaysia Faculty of Mechanical Engineering Universiti Teknologi Malaysia, 81310 Skudai, Johor, Malaysia Abstract—Tracheal stenosis is a condition where the diameter size of trachea wall decreases and leads to the obstruction of the breathing airflow. Investigation on the effect of the stenosis to the airflow pattern in the trachea and main bronchi is the objective for this study. CT-scan images of two airways models were modeled, one with the stenosis and one without. Numerical solution was used to study the airway pattern inside the airway. Different boundary conditions of inspirations flow rate were applied; 15 l/min, 60 l/min and 100l/min where the ratio for the right main bronchus is 55% and for the left main bronchus is 45%. The results showed that the pressure drop inside the stenosis model is higher compared to that of healthy model. The pressure drop was also shown to interrupt the inlet condition into the main bronchi. Keywords- Trachea, main bronchi, CT-scan images, simplified model and respiratory system. Introduction Knowledge about airflow in human airways was known as the alternative source that helps in treatment for the breathing patients. The treatment for the respiration disease usually in the form of aerosol that delivered into the lung and the efficiency of the treatment is depends on the percentage of the drug particle received by the lung. Tracheal stenosis is one of the tracheal symptoms that obstruct the airways path and lead to breathing difficulties. Thus, present study aims to explore the flow dynamics inside the actual abnormal trachea which are suffering of stenosis. Ideally, the flow pattern would be different and inconsistent compared to healthy trachea. The very straight way to understand the airflow characteristics are to study its pressure drop and velocity field along the tracheabronchial region. Numerous numerical studies of inhaled airflow and particle transport modeling have been performed until now. Schroter and Sudlow [1] initiated the earliest study of airflow inside the human lung. Their experimental study of single symmetric bifurcation and flow was at Reynolds numbers ranging from 50 to 4500 concluded that the inhale flows were independent on either Reynolds number and entry velocity profiles. It was followed by other studies which address varieties of airflow and particle deposition problems in selected segment at bifurcation, main bronchi and lower generations [2-6]. They have shown that simulation of airflow and particle transport at different bronchi’s generation with different boundary conditions resulting significant changes of velocity and pressure drop which influenced the breathing cycle. However, all the research named above was used simplified 45 model of human lung due to the limitation of applications. Their findings and conclusions were initiated this present study to go deeper on investigation of air flow dynamics patterns in actual human lung model. Besides, studies on airflow and particle deposition inside abnormal trachea specifically have received relatively small numbers. In 2006, Mark Brouns et al. [7] made the earliest study of Computational Fluid Dynamics (CFD) simulations within model of stenosis trachea. They initiated a study of flow dynamics inside a few sizes of stenosis and found that pressure drop dramatically increased due to the constriction of trachea airways and concluded that the pressure drop can be detected at early stage of stenosis. Although Mark Brouns et al. simulated airflow inside a few conditions of model geometry and boundary condition, the results produced still can be argued. It is because the model used have smooth wall, no rings protrusions effect, and only shows flow pattern until centre of trachea. We believed that the actual wall conditions, shapes, angle of bending, bifurcation of main bronchi and all the boundary conditions are a priority in analyzing the effect of stenosis on air flow inside trachea. In this study, two actual models of trachea are used; with and without the stenosis. The flow pattern in healthy trachea is benchmark to the stenosis trachea. Dimensionless techniques were used along the way of analyzing the result. Methodology A. The model geometry The complexity of the actual airway geometry is essential in improving the efficiency of simulation airflow to capture the velocity distribution and pressure drop. For this study, two models with different geometry conditions were utilized for comparison purpose (figure 1). The models were reconstructed from the Computed Tomography (CT) scan images by using modeling software before being exported into Computational Fluid software for simulation of airflow. The images of the reconstructed model of human airways consists of trachea and main bronchi were taken from an Asian, 60 years old male as for stenosis model and the stenosis area for the same model then been removed to used as the healthy model. Smoothing of the surface was performed on the model to eliminate the roughness of the curves caused by partial volume effects and pixilation of rounded images [8]. The model provides an anatomically realistic model of human airways Figure 1: The extracted actual model of trachea and main bronchi from CT images. Healthy model (left) and abnormal trachea with constriction of stenosis model (right). B. Boundary conditions Beside the model geometry, boundary conditions are another factor that needs to be looked while studying the airflow [2]. Laminar flow does not occur in human lung airways except in very small airways deep down into the lung at resting condition [9]. The airflow from larynx to third generation is transitional-toturbulent even at a low local Reynolds number. The turbulence may be induced again at the central zone due to flow instabilities generated by the great geometric transition at the carinal ridges which may complicate flow structures [10] have shown that the turbulent influenced the particle deposition. Higher particle deposition was recorded for turbulent flow over laminar flow [11]. Thus, the turbulence generated by the larynx need to be taken into account. K-epsilon model is appropriate to simulate internal laminar-transitional-turbulent flow. The actual model wall was assumed as smooth and rigid wall along the airways. In the actual trachea, the wall actually covers by cilia and normally lined up with mucus which tends to make it smooth. It is also have the cartilage rings to support the trachea. The airflow in healthy and stenosis human airways is to be solved using k-epsilon model. 46 The k-epsillon was empployed as paart of the consideratioon for occurrennce of turbuleent flow at low Reynoldds numbers as a a result of shear s flow and its proven ability too simulate thhe airflow [12]. A commercial finite-volum me based software Enngineering Fluid F Dynamiics (EFD) was deployeed to solve stteady state conservation of mass andd momentum equations in all cases. The EFD iss capable of solving s turbullent model by employinng a finite-vollume method.. The flow rates imposeed at the outlets are compuuted based on flow parrtitioning ratiion given by Horsfield [13] where 55% of inlet flow rates diiverge into right broncchus while 45% 4 of flow into left bronchus. The T conditionss imposed on the t outlets are summariized in Table 1 b trachea model m for Table I: Parrameters at both three differeent breathing conditions. c Parameeter Flow raate (l/min) Inlet Prressure Densityy Viscosiity Incompressible flow 15,60 and 100 101325 Paa 1.225 kg/m m3 1.7894e-055 kg/ms1 area after the stenosis is locateed. The gnificant difference became more sig when the flow rate increases ass shown. The diffferences aare due to the obstructionn and redduce sizes of the trachea diiameter at the stenosis and it affected thhe flow from m moving smoothly s to the main m bronchhi. The flo ow that reaches to each side oof the main n bronchi also effeccted when the differeent flow rates were applied intto both mod del. Then again, for the velocity co ontour, it started to show diffferences in contour when appplying the 60 l/min and a 100 The l/min booundary cconditions. contours are a more uuniform thrroughout the tracheea and maiin bronchi for the healthy model m compaared to the stenosis model. For the steenosis mod del, the velocity fllow happeniing to distraact when reach the obstructioon and staarting to speed up before b it beecame unev ven. But the locatioon of the sstenosis itseelf is far enough foor the veloocity to refform the uniform profile bbefore reaach the bifurcationn area. (a) 15 l/m min Re esult and Discussiion A. Pressurre and veloccity contourrs The veloocity and thhe pressuree contour throughouut the trachhea and thhe main bronchi are a shown in Figuree 2 and Figure 3.. Both coontours aree almost similar foor both heealthy and stenosis models foor the restting flow rate (15 l/min). Thhere are no significant pressure drop and velocity different d thrroughout the tracheea and main bronchi for both models. The T contouurs begin to t show different between both b modells when simulated using 60 l//min and 100 l/min flow rates. From the Figure 2 (b) ( and Figuure 2 (c), it shows that the presssure drop is i higher in the steenotic modeel especiallly at the Healthy model m Stenosis model m 47 (a) 15 l//min (b) 60 l/m min Healthyy model model Healthy model m Stenosiis model Sttenosis (b) 60 l//min (c) 100 l/m min Healthyy model Steenosis moddel (c) 100 l/min Healthy model m Stenosis model m Figure 2: Simulated pressure coontour in the tracheea and mainn bronchi inn healthy and stenoosis modelss at differeent flow rates. (a) 15 l/min, (bb) 60 l/minn and (c) 100 l/min Healthy mode m Stenosiss model 48 (a) 15 l/min Figure 3: Simulated velocity contour in the trachea and bronchus in healthy and stenosis models at different flow rates. (a) 15 l/min, (b) 60 l/min and (c) 100 l/min B. Pressure and velocity distributions Figure 4 and Figure 5 show the simulated pressure and velocity distributions along the centerline of healthy and stenosis models at different flow rates. In general, the pressure drop occur in the stenosis model is much higher than that in the healthy model. It is happens due to the contraction at the stenosis area that effect the pressure distribution along the airways. The overall pattern of the pressure distribution in stenosis model still having the same pattern as the healthy model except at the stenotic area where the large drop of pressure value take place. It is shown at every flow rates applied for each model. With reference to velocity distribution plots, the pattern for both model showing the same pattern except the velocity in the stenosis model having higher spped especially when reach the stenosis area. For the resting flow rate (15 l/min), there are not significant gap between the healthy and stenosis model and it started to have a different when the flow rate increases. Overall, due to the location of the stenosis that located at the beginning of the trachea which is far enough from the bifurcation area, the pressure and the velocity distribution did not effected the flow characteristic too much and the flow still reach at the main bronchi in content condition. (b) 60 l/min (c) 100 l/min Figure 4: CFD simulated pressure drop along the centerline of trachea and main bronchi in healthy and stenosis models 49 at different flow rates. (a) 15 l/min, (b) 60 l/min and (c) 100 l/min (a) 15 l/min Figure 5: CFD simulated velocity distribution along the centerline of trachea and main bronchi in healthy and stenosis models at different flow rates. (a) 15 l/min, (b) 60 l/min and (c) 100 l/min Conclusion Stenosis inside the trachea did affect the flow characteristic for human airways. The results show that the flow pattern will become more non-uniform when the flow rates apply increases. The results also show that the stenosis affect the flow in the trachea as well as the inlet flow condition into the main bronchi. References (b) 60 l/min [1] (c) 100 l/min Schroter, R.C., Sudlow, M.F., 1969. “Flow patterns in model of the human bronchial airways”. Respiratory Physiol.J. 7, 341–355 [2] Natalya Nowak, Prashant P.Kakade and Ananth V.Annapragada, “Computatioal fluid dynamics simulation of airflow and aerosol deposition in Human Lung”, Annals Biomedical Engineering Vol.31,pp.374390,2003 [3] Martonen T.B., and I.M.Katz, “Deposition patterns of polydisperse aerosols within human lung, J.Aerosol Med 6:251-274,1993 [4] Balashazy, I., T.Heistracher and W.Hofman, “Airflow and particle deposition patterns in bronchial airways bifurcation, J.Aerosol Med. 9:287-301,1996 [5] Zhang, Z., and C.Kleinster, “Effect of particle inlet distributions on deposition in a triple bifurcation lung airway model; Edwards, D.A. “Numerical simulation of air and particle transport in the conducting airways, J. Aerosol Med.9:303-316;1996 [6] I.M. Katz and T.B Martonen, “Flow patterns in 3D laryngeal model, Journal Aerosol Medicine,9, 501-511 (1996) [7] Mark Brouns .M,Jayaraju, S.T. Lacor C., Mey JD, Noppen M, Vincken, W.Verbanck, “Tracheal stenosis”, A Flow Dynamics Study, Journal Applied Physiology 2006 [8] Thomas A. Spirka, Jerry G. Myers, Randolph M. Setser, Sandra S. Halliburton, Richar D. White, George P. Chatzimavroudis. “Construction of a computational non-planar curved tube models from MRI data”. IEEE IST 2005. International Workshop on Imaging Systems and Techniques. [9] R.K.Calay,Jutarat Kurujareon and Arne Erik Holdo, “Numerical simulation of respiratory flow patterns within human lung, Respiratory Physiology & Neurobiology 130 (2002) 201-221 [10] Zhang, Z. and Kleinstreuer, C. (2004). Airflow structures and nano particle deposition in a human upper airway model. Journal of Computational Physics, 198, 178-210 [11] J. Russo, R. Robinson, Michael J. Oldham (2008), Effects of cartilage rings on airflow and particle”, Journal of Medical 50 [12] Luo, X. Y., Hinton, J. S., Liew, T. T., Tan, K. K., LES modelling of flow in a simple airway model, Medical Engineering & Physics 26 (2004) 403–413 [13] Horsfield, K., Dart, G., Olson, D.E., Filley, G.F., Cumming, G. (1971). Models of human branching airways. J. Appl. Physiol. 31: 207-21 51