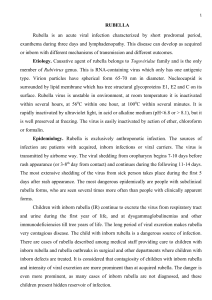
Rubella-virus associated uveitis Aniki Rothova Erasmus Medical Center Rotterdam, Netherlands
advertisement

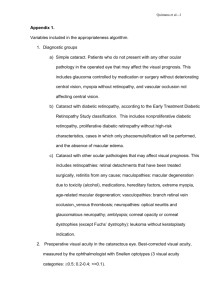
Rubella-virus associated uveitis Aniki Rothova Erasmus Medical Center Rotterdam, Netherlands Ocular / General History 35-year-old female presented with gradually decreasing visual acuity RE General medical history: not contributory Ocular findings at first presentation Note the lighter blue color of RE and wider pupil RE Ocular Examination OD: visual acuity 0.7 Keratic precipitates all around the corneal endothelium, mixed fine and mid-large Cells in anterior chamber 1+ Subcapsular posterior cataract Cells in anterior vitreous No retinal abnormalities, OS: visual acuity 1.25, no abnormalities IOP 19/13 mmHg Iris details Note the widespread distribution of keratic precipitates and their mixed size (fine and mid-large) and small nodules on the pupillary rim in combination with visible fine vascular network on the iris Presumed diagnosis: FHUS Clinical diagnosis based on: absence of acute inflammatory signs (no redness and pain) cells in anterior chamber and vitreous, but no synechiae cataract additional findings: visible vasculature of the iris and hyphema development during intraocular surgery 20% bilateral involvement, 20% glaucoma, 10-15% “toxo-like” chorioretinal scars Problems Diagnosis of FHUS is clinical and causes of this syndrome may vary High association with cataract and glaucoma FHUS in Europe: 95-100% of cases have intraocular antibody production against RV Not prevalent in vaccinated population Additional Information Patient was vaccinated according to official guidelines Received rubella vaccine at the age of 11 (before the combination vaccine currently used) Symptomatic rubella infection in our patient was not documented, but patient was probably infected before her vaccination Examinations Aqueous analysis: PCR for HSV, VZV, CMV and RV: negative Goldmann Witmer coefficient : for HSV, VZV and CMV: negative for Rubella virus =16 (highly positive, intraocular titers 1280> 260 serum titers) Final Diagnosis Rubella virus-associated uveitis Follow-up: Patient prefers to wait with cataract surgery No treatment despite the cells + Regular controls (cataract and glaucoma) Conclusion Fuchs heterochromic uveitis syndrome caused by Rubella virus: No treatment for rubella virus available Treatment with corticosteroids not satisfactory Regular follow-up is indicated for control of cataract development and IOP increase