Document 14476368
advertisement

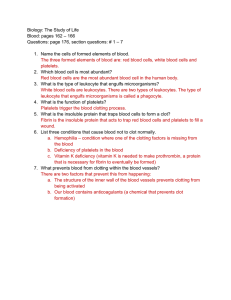
University of Baghdad College of Nursing Department of Basic Medical Sciences Overview of Anatomy and Physioloy –II Second Year Students Asaad Ismail Ahmad , Ph.D. Electrolyte and Mineral Physiology asaad50.2011@gmail.com 2012 - 2013 ANATOMY AND PHYSIOLOGY - II Brief Contents 1- Cardiovascular System 2- Blood 3- Lymphatic System 4- Urinary System 5- Male Reproductive System 6- Female Reproductive System 7- Sensory Function Asaad Ismail Ahmad, Ph.D in Electrolyte and Mineral Physiology College of Nursing – University of Baghdad / 2012 – 2013 asaad50.2011@gmail.com Text book Martini FH. Fundamentals of Anatomy and Physiology, 5th ed. Prentice Hall, New Jersey, 2001. References: 1.Barrett KE, Barman SM, Boitano S, Brooks HL. Ganong's Review of Medical Physiology, 23rd ed. McGraw Hill, Boston, 2010. 2.Drake RL, Vogl W, Mitchell AWM. Gray's Anatomy for Students. Elsevier, Philadelphia, 2005. 3.Goldberger ,E. 1975.A Primer of Water Electrolyte and Acid-Base Syndromes. 5th ed., Lea and Febiger ,Philadelphia. 4. Martini, FH and Welch K. Applications Manual Fundamentals of Anatomy and Physiology,4th ed., Prentice Hall, NewJersey, 1998. 5.Maxwell, MH and Kleeman CR. 1980.Clinical Disorders of Fluid and Electrolyte Metabolism. McGraw-Hill Book Company, New York. 6.McKinley M, and O'Loughlin VD. Human Anatomy, McGraw Hill, Boston, 2006. 7.Nutrition Foundation.1984.Present Knowledge in Nutrition. 5th ed., Nutrition Foundation, Inc , Washington, D.C. 8.Vander A, Sherman J, Luciano D., Human Physiology, 7th ed., McGraw Hill, Boston, 1998. BLOOD Contents: BLOOD 1- Overview of the blood. 2. Functions of the Blood. 3. Plasma 4. Erythrocytes (Red Blood Cells). 5. Leukocytes (White Blood Cells). 6. Platelets (Thrombocytes). 7. Hemopiesis (Hematopoiesis). 8. Hemostasis. Asaad Ismail Ahmad, Ph.D in Electrolyte and Mineral Physiology College of Nursing – University of Baghdad / 2012 – 2013 asaad50.2011@gmail.com SIXTH LECTURE Blood 6. Platelets (Thrombocytes). 7. Hemopoiesis (Hematopoiesis). 8. Hemostasis. Asaad Ismail Ahmad, Ph.D in Electrolyte and Mineral Physiology College of Nursing – University of Baghdad / 2012 – 2013 asaad50.2011@gmail.com CONTENTS: 6. Platelets (Thrombocytes). Continue: Overview PLATELETS 1234- Small fragments of megakaryocyte cytoplasm 2-4 um diameter, contain granules Rather than individual cells, it is flattened disc, round. Each platelet circulate in the bloodstream for 9-12 days, before being removed by phagocyte. 5- Normal count: 130,000 – 400,000 ul FUNCTION: 1- Secrete clotting factors and growth factors for vessels repair 2- Initiate formation of clot dissolving enzyme Platelets Production (Thrombocytopoiesis): Megakaryocytes in bone marrow manufacture Structural proteins, enzymes, and membrane. They shade cytoplasm in small membrane enclosed packet. These packets are platelets. A mature megakaryocyte produce 4000 platelets platelets Onions & Low Platelet Count Onions contain a chemical that is known to reduce platelet activity in humans and dogs. Continue: Hemopoiesis (Hematopoiesis) Asaad Ismail Ahmad, Ph.D in Electrolyte and Mineral Physiology HEMOPOIESIS (HEMATOPOIESIS): PRODUCTION OF FORMED ELEMENTS Hemopoiesis occurs in red bone marrow. The Process of hemopoiesis starts with hemopoietic Stem cells called Hemocytoblasts, which consider Pluripotent cells. Hemocytoblasts differentiate Into many different kinds of cells. Hemocytoblasts produce two lines for blood cell development: 1- Myeloid (line) Stem Cells forms erythrocytes, Megakaryocytes and all leukocytes except Lymphocytes. 2- Lymphoid (line) Stem Cells forms lymphocytes. Production of blood cells by the bone marrow TYPES OF HEMOPOIESIS (HEMATOPOIESIS) Hematopoiesis: Blood cells formation and differentiation in bone marrow TYPES OF HEMOPOIESIS 1- Erythropoiesis : Red blood cell formation inbone marrow. 2- Leukopoiesis : White blood cell formation. 3- Lymphopoiesis: Production of lymphocytes from lymphoid stem cells. 4- Thrombocytopoiesis: Platelets production. Asaad Ismail Ahmad, Ph.D in Electrolyte and Mineral Physiology FACTORS REGULATE ERYTHROPOIESIS (RBCs PRODUCTION) 1- Erythropoietin (EPO): hormone secreted by kidneys. 2- Hormone: thyroxin, androgen, cortisol. 3- Vitamin: B12, B6, Folic acid, vitamin C 4- Amino acids: for synthesis hemoglobin. 5- Metals: iron, cobalt and manganese. FACTOR REGULATE THROMBOCYTOPOIESIS 1- Thrombopoietin: hormone produce by kidneys FACTORS REGULATE LEUKOPOIESIS (WBCs PRODUCTION) 1- Multi-CSF: granulocyte, monocyte, platelets, RBCs colony stimulating factor. 2- GM-CSF: granulocyte, monocyte colony S.factor 3- G-CSF : granulocyte colony stimulating factor. 4- M-CSF : monocyte colony stimulating factor. 5- Thymosin: hormone produce by thymus stimulate T- lymphocyte maturation and B- lymphocyte production. 6- Antigens: exposure to antigens promote the production of lymphocytes, B-cells and T-cells Note: the 1st, 2nd, 3rd and 4th factors are secreted by lymphocytes. CONTENTS: HEMOSTASIS Asaad Ismail Ahmad, Ph.D in Electrolyte and Mineral Physiology HEMOSTASIS 645 (positive feedback control of blood clotting) Hemostasis: stopping the bleeding through the wall of damage vessels, by clot formation or vessel spasm. The processes (steps)of hemostasis are: 1- Vascular phase 2- Platelets phase 3- Coagulation phase HEMOSTASIS: 1– VASCULAR PHASE Vascular phase lasts about 30 minutes, start When the wall of blood vessels is cutting. During this phase the following changes occurs: 1- Vascular spasm: contraction of local smoth Muscle fibers of the vessel wall. 2- Releasing chemical factors (mediators): (prostacyclin, nitric oxide) and local hormones (endothelins), by endothelial cells. 3- Endothelium cell membrane become sticky: On opposite side of the vessel endothelial cells Stick together. 2- PLATELET PHASE (PLATELET PLUG) Platelet phase start when the platelets attached to sticky endothelial surface. This process Called platelets aggregation forming platelets plug . This begins within “15 second” after injury (damage). When the platelets arrive injury site it becomes Activated and begin to releasing: 1- ADP “adenosine Diphosphate” 2- Thromboxane A2 3- Serotonin 4- Clotting factors 5- platelets growth factor 6- Calcium ions “ Ca++” 3- COAGULATION PHASE (formation of blood clot) 647 Cagulative phase dose not start until 30 seconds after the vessel has been damaged. Coagulation or formation of blood clotting involve complex process leading to conversion of soluble circulating Fibrinogen into the insoluble protein fibrin. As the fibrin network grows, it covers the surface of platelet Plug. Passing blood and additional platelets are trapped in the fibrous tangle, forming a blood clot, which effectively seals off the damaged portion of the vessel Asaad Ismail Ahmad, Ph.D in Electrolyte and Mineral Physiology BLOOD CLOT BLOOD CLOT BLOOD CLOT CLOTTING FACTORS 648 I- Fibrinogen II- Prothrombin(vit.k) III- Tissue factor IV- Calcium ions(Ca++) V- Proaccelerin VI no longer used VII-Proconvert (vit.k) VIII-Antihemophilic IX- Plasma thromboplastin (vit.k) X- Stuart-power factor (vit.k) XI- Plasma thromboplastin XII- Hageman factor XIII- Fibrin-stabilizing NEGATIVE FEEDBACK CONTROL OF BLOOD CLOTTING ( regulation of clotting mechanisms ) 1- Heparin: release by basophil and mast cells, activate antithrombin III. Heparin used clinically to prevent clotting. 2- Thrombomodulin: protein release by endothelial cells, bind to thrombin and convert it to enzyme activate protein C, then protein C inactivate several clotting factors and stimulate formation of plasmin, the enzyme that gradually breaks down fibrin strands. Continue: NEGATIVE FEEDBACK CONTROL OF BLOOD CLOTTING 3- Prostacyclin and Nitric oxide: release by normal intact endothelial cells, to maintain resting platelets and inhibit platelets aggregation and opposes the action of thrombin, ADP, and other clotting factors. 4- Alpha-2-macroglobulin: plasma protein inhibit thrombin and several clotting factors. 5- Magnesium ions (Mg++): is anticoagulant factor. Continue: NEGATIVE FEEDBACK CONTROL OF BLOOD CLOTTING 6- Antithrombin, proteins C & S These proteins are the body’s natural anticoagulants, hence deficiencies may lead to thromboembolic disease Factors Decrease Antithrombin ( AT levels ) 1- Hereditary (40–60% normal level), autosomal dominant. 2- Chronic liver disease. 3- Protein wasting disorders. 4- Heparin therapy. 5- 3rd trimester of pregnancy. 6- Acute leukaemia. 7- Burns. 8- Renal disease. 9- Gram –ve sepsis. CLOTTING RETRACTION AND FIBRINOLYSIS Fibrinolysis: process of dissolving clot. 1- Activation of proenzyme” plasminogen” by; a- Thrombin b- Tissue plasminogen activator 2- Plasminogen change to plasmin. Plasmin is the enzyme which digesting and eroding the clot. Note: clot retraction occurs within 30-60 minutes Asaad Ismail Ahmad, Ph.D in Electrolyte and Mineral Physiology HEMOSTASIS DISORDERS I- Inadequate blood clotting 1- Hemophilia a- Hemophilia type A - deficiency factor 8 b- Hemophilia type B - deficiency factor 9 c- Hemophilia type C - deficiency factor 11 II- Excessive blood clotting 1- Thrombosis: formation of thrombus Thrombus : blood clot attached to vessel wall 2- Embolism: blood clot, fat globule, air or bubble circulating in the blood. 3- Infarction Asaad Ismail Ahmad, Ph.D in Electrolyte and Mineral Physiology