Prematurity Module AnS 536 April 22, 2016
advertisement

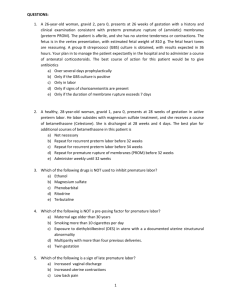
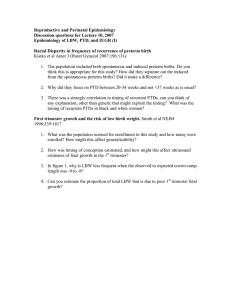
Prematurity Module AnS 536 April 22, 2016 Overview Prematurity Preterm labor Fetal and maternal pathology Physiological concerns What is Prematurity? Prematurity is defined as less than 37 weeks of gestation in humans Prior to 32 weeks is considered a very premature birth Less than 28 weeks is extremely premature Preterm Labor Birth prior to expected delivery date Occurs for a variety of reasons early rupture of fetal membranes can lead to amnionitis Methods to prevent labor stop /delay onset of pre-mature births does not guarantee a healthy infant Planned interventions to terminate pregnancy serious maternal illness problems affecting fetal well being or growth Preterm Labor Preterm labor prevention: Social measures increasing awareness of risk factors negatively impacting pregnancy smoking and alcohol consumption sexually transmitted diseases Physical measures regular doctor visits throughout pregnancy uterine-activity monitoring bed rest cervical assessment Preterm Labor Preterm labor prevention (cont.) Surgical measures cervical cerclage (applying stitches) Pharmacological agents betamimetic drugs stop uterine contractions in active labor most widely used among other labor-inhibiting agents inhibitors of prostaglandin synthesis strong and practical use in preventing labor antibiotics some use in preventing early labor in women with bacterial vaginosis Preterm Labor Types of preterm births Antepartum death Lethal malformations fetal outcome cannot be changed, vitality of mother is important Multiple pregnancies 50% of all multiple pregnancies result in premature delivery Elective deliveries Maternal and/or fetal pathology preclampsia antepartum hemorrhage intra-uterine growth restriction Antepartum death and lethal malformations 10-15% of all premature births Almost 50% of total perinatal mortality This form is unsavable Infant dies before labor or has malformations that are incompatible with life (fetal termination of pregnancy) Maternal well-being is a large factor Ethical controversy on outcome Multiple Pregnancy Any pregnancy involving more than one fetus Almost half of multiple births occur prematurely Multiple births are 15 times more likely to be associated with premature delivery Multiple births make up 20% of all premature cases Elective Delivery Planned obstetric decision Complications during pregnancy within the mother or the fetus Not necessarily premature infants have to be less than 37 weeks in gestation Maternal and Fetal Pathology Preeclampsia more severe eclampsia Antepartum hemorrhage placental abruption placental previa Intra-uterine growth restriction Spontaneous preterm labor Preeclampsia Mother develops high blood pressure during pregnancy (>140/90 mmMg) At risk 28 weeks gestation – 48 hours postpartum Symptoms include proteinuria, headaches, trouble with vision, upper abdominal pain, nausea and vomiting, decreased urination, thrombocytopenia, decrease liver function, and difficulty breathing Unnoticed mother at risk of eclampsia seizures or self-induced coma Antepartum Hemorrhage Bleeding from the birth canal (>20 weeks) Placental abruption placenta separates from uterine wall blood pools between placental and endometrium Placental previa placental attaches to lower uterus, covers opening of cervix worsens as pregnancy progresses Intra-uterine Growth Restriction Placenta develops abnormally= less room for the fetus to grow Fetus is smaller than normal while the cranium and feet are normal size Symmetric and asymmetric Low birth weight, sensitivity to vaginal delivery, hypoxia, hypoglycemia, decreased immune function, depressed thermoregulation, higher than normal red blood cell count, increased chance of meconium staining, and a low APGAR Spontaneous Preterm Labor Premature labor with no expected cause Route for Delivery Vaginal or Cesarean Section Breech much more common in preterm when unplanned Safer for premature infants to use C-section depending on how far along in gestation Premature baby is more susceptible to compress from the pelvic region than a term baby they have a softer skull Cow c-section video: https://www.youtube.com/wa tch?v=oAqM505ZsFI Preterm Birth Physiological consequences infant’s body systems are not prepared to function on their own numerous conditions that result from prematurity can be treated depending upon extent of prematurity, morbidity rate may be high Preterm Birth Preterm birth is the leading cause of neonatal mortality lack of development of body systems is underlying cause Concerns: increased morbidity and mortality intraventricular hemorrhage (IVH) periventricular leukomalacia (PVL) cerebral palsy necrotizing enterocolitis (NEC) retinopathy of prematurity (ROP) respiratory distress syndrome (RDS) Neurological Concerns Intraventricular hemorrhage (IVH) blood vessels of brain not fully developed bleeding in ventricles of the brain premature infants at a much higher risk (>10 weeks early) occurs after birth within the first couple of days of life not preventable increase risk if other problems Hydrocephalus fluid accumulation in the brain Neurological Periventricular leukomalacia (PVL) softening in the white matter of the ventricles severe damage or death to this part of the brain born >10 weeks early, babies with IVH more likely to experience PVL hypoxia or uterine infection during gestation no treatment can cause cerebral palsy Respiratory Respiratory distress syndrome (RDS) Over 50% of premature infants Pulmonary surfactant produced during late pregnancy Use different techniques to speed up pulmonary maturation or assist lung function- corticosteriods betamethasone and dexamethasone Gastrointestinal and Metabolism Immature digestive system= abnormal digestion and reaction to the diet Necrotizing enterocolitis (3-7d after birth) cells in bowel are injured become inflammed cells spontaneous necrose infants fed only breast milk have lower risk surgically treated by removing dead tissue withdrawn feedings Immunity Compromised immune system= prolonged time in the NICU Lower levels of IGg & delayed development of innate immune response Passive transfer across the placenta occurs during third trimester Neutropenia at birth Renal System Decreased ability to maintain blood pressure Difficult time regulating electrolyte and water balance Glomeruli and tubules in the kidney that are responsible for blood filtration and urine secretion are not fully functionally until 6 weeks of age in full term babies Thermoregulation Less brown fat stores At high risk to hypothermia leads to breathing problems and low blood glucose Use available energy for heat hypoglycemia decreased stores of glycogen lower rates of grain and slow development after birth Preterm Birth in Cattle Abortions- 42-260 days of gestation Preterm birth >260 days concern for producers when incidence is over 35% in herd viral (BVD, IBR) bacterial infection genetic defects heat stress- hypoxia, hypotension and acidosis toxins in feed Ponderosa pine needles zearalenone (moldy forages) (Hovingh, 2009) Prevention of Preterm Birth Cattle Routine pregnancy checks Following vaccine protocol specific to herd administering at appropriate times Clean breeding techniques AI techs and ov/estrous sync (CIDRs) bull soundness exams (virgin bulls preferred) Heat abatement especially dry cows and prefresh pens Proper nutrition management Take home messages The health and well being of the mother greatly effects the health of the fetus and can increase the risk of premature labor The level of prematurity depends on how early birth occurs the more premature= more development/health concerns Some conditions are not treatableprevention is key References Folkerth, R.D. 2006. Periventricular Leukomalacia: Overview and Recent Findings. Pediatric and Developmental Pathology 9(1):3-13. doi:10.2350/06-01-0224.1 Gilliam, M., D. Rosenberg, and F. Davis. 2002. The Likelihood of Placenta Previa With Greater Number of Cesarean Deliveries and Higher Parity. Obstetrics and Gynecology 99(6):976-980. Gubhaju, L., M.R. Sutherland, and M.J. Black. 2011. Preterm Birth and the Kidney: Implications for Long-Term Renal Health. Reproductive Sciences 18(4):322-333. doi:10.1177/1933719111401659 Henry, D.L., T.F. McElrath, and N.A. Smith. 2013. Preterm Severe Preeclampsia in Singleton and Twin Pregnancies. Journal of Perinatology 33:94-97. doi: 10.1038/jp.2012.74 Hovingh, E. 2009. Abortions in Dairy Cattle (Virginia Cooperative Extension). http:// pubs.ext.vt.edu/404/404-288/404-288.html Kaneshiro, N.K. 2014. Premature Infant (A.D.A.M. Medical Encyclopeda). http://www.nlm.nlh..gov/medlineplus/ency/article/001562.htm (Accessed 3 March 2016). Kendig, J.W., and U. Nawab. 2015. Necrotizing Entercolitis (Merck Manual) http://www.merckmanuals.com/professionalpediatrics/perinatal-problems/ necrotizingentercolitis (Accessed 3 March 2016). Knobel, R.B. 2014. Thermal Stability of the Premature Infant in Neonatal Intensive Care. Newborn & Infant Nursing Reviews 14(2):72-76. doi:10.1053//nainr.2014/03/002 References (cont.) Linder, N., O. Haskin, O. Levit, G. Klinger, T. Prince, N. Naor, P. Turner, B. Karmazyn, and L. Sicota. 2007. Risk Factors for Intraventricular Hemorrhage in Very Low Birth Weight Premature Infants: A Retrospective Case-Control Study. Pediatrics 111(5):590-595. Magann, E.F., D.A. Doherty, K. Turner, G.S. Lanneau, J.C. Morrison, and J.P. Newnham. 2007. Second Trimester Placental Location as a Predictor of Adverse Pregnancy Outcome. Journal of Perinatology 27:9-4. doi:10.1038/sj.jp.7211621 Melville, J.M., and T.J. Moss. 2013. The Immune Consequences of Preterm Birth. Frontiers and Neuroscience 7(79) doi:10.3389/fnins.2013. Papile, L., G. Munsick-Bruno, and A. Schaefer. 1983. Relationship of Cerebral Intraventricular Hemorrhage and Early Childhood Neurologic Handicaps. Journal of Pediatrics 103(2): 273-277. Redman, C., and I.L. Sargent. 2005. Latest Advances in Understanding Preeclmampsia. Science 308(5728):1592-1594. doi:10.1126/science.1111726 Reshink, R. 2002. Intrauterine Growth Restriction. Obstetrics & Gynecology 99(3):490-496. Woolston, M.S. 2016. Premature Births on the Rise (Health Day). http://consumer.healthday.com/ encyclopedia/pregnancy-33/pregnancy-news- 543/premature-births-on-therise643869.html (Accessed 6 March 2016). Zohdi, V., L. Kyungjoon, J.T. Pearson, and M.T. Black. 2015. Developmental Programming of Cardiovascular Disease Following Intrauterine Growth Restriction: Findings Utilizing a Rat Model of Maternal Protein Restriction. Nutrients 7(1):19-152. doi:10.3390/nu7010119 Questions?