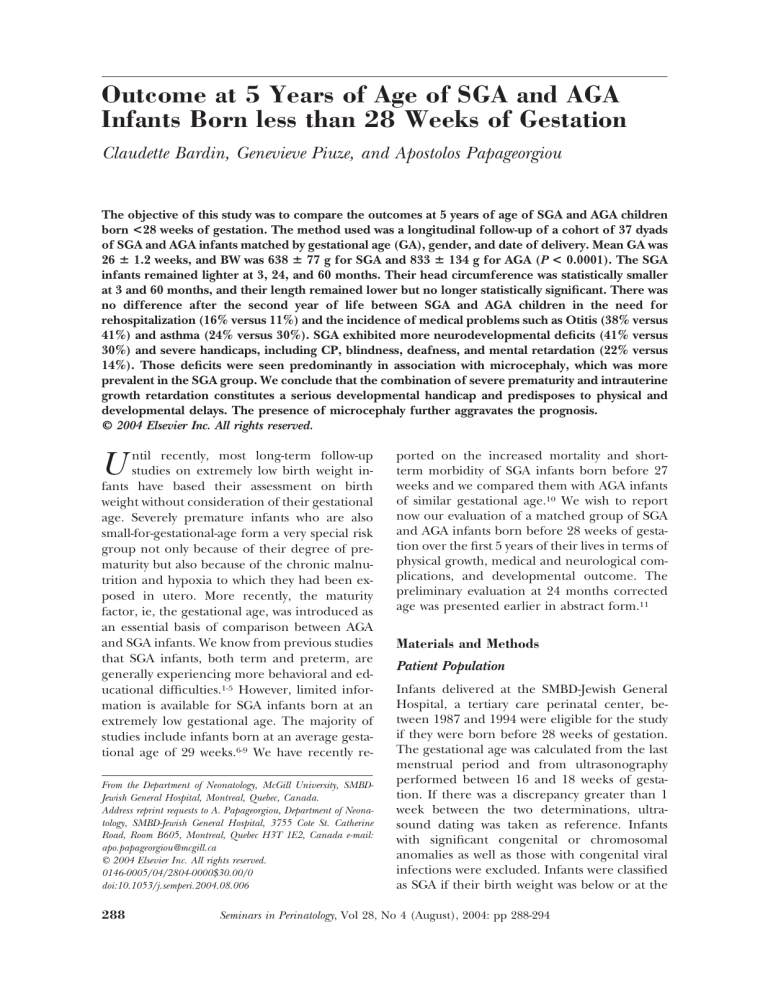
Outcome at 5 Years of Age of SGA and AGA
Infants Born less than 28 Weeks of Gestation
Claudette Bardin, Genevieve Piuze, and Apostolos Papageorgiou
The objective of this study was to compare the outcomes at 5 years of age of SGA and AGA children
born <28 weeks of gestation. The method used was a longitudinal follow-up of a cohort of 37 dyads
of SGA and AGA infants matched by gestational age (GA), gender, and date of delivery. Mean GA was
26 ⴞ 1.2 weeks, and BW was 638 ⴞ 77 g for SGA and 833 ⴞ 134 g for AGA (P < 0.0001). The SGA
infants remained lighter at 3, 24, and 60 months. Their head circumference was statistically smaller
at 3 and 60 months, and their length remained lower but no longer statistically significant. There was
no difference after the second year of life between SGA and AGA children in the need for
rehospitalization (16% versus 11%) and the incidence of medical problems such as Otitis (38% versus
41%) and asthma (24% versus 30%). SGA exhibited more neurodevelopmental deficits (41% versus
30%) and severe handicaps, including CP, blindness, deafness, and mental retardation (22% versus
14%). Those deficits were seen predominantly in association with microcephaly, which was more
prevalent in the SGA group. We conclude that the combination of severe prematurity and intrauterine
growth retardation constitutes a serious developmental handicap and predisposes to physical and
developmental delays. The presence of microcephaly further aggravates the prognosis.
© 2004 Elsevier Inc. All rights reserved.
ntil recently, most long-term follow-up
studies on extremely low birth weight infants have based their assessment on birth
weight without consideration of their gestational
age. Severely premature infants who are also
small-for-gestational-age form a very special risk
group not only because of their degree of prematurity but also because of the chronic malnutrition and hypoxia to which they had been exposed in utero. More recently, the maturity
factor, ie, the gestational age, was introduced as
an essential basis of comparison between AGA
and SGA infants. We know from previous studies
that SGA infants, both term and preterm, are
generally experiencing more behavioral and educational difficulties.1-5 However, limited information is available for SGA infants born at an
extremely low gestational age. The majority of
studies include infants born at an average gestational age of 29 weeks.6-9 We have recently re-
U
From the Department of Neonatology, McGill University, SMBDJewish General Hospital, Montreal, Quebec, Canada.
Address reprint requests to A. Papageorgiou, Department of Neonatology, SMBD-Jewish General Hospital, 3755 Cote St. Catherine
Road, Room B605, Montreal, Quebec H3T 1E2, Canada e-mail:
apo.papageorgiou@mcgill.ca
© 2004 Elsevier Inc. All rights reserved.
0146-0005/04/2804-0000$30.00/0
doi:10.1053/j.semperi.2004.08.006
288
ported on the increased mortality and shortterm morbidity of SGA infants born before 27
weeks and we compared them with AGA infants
of similar gestational age.10 We wish to report
now our evaluation of a matched group of SGA
and AGA infants born before 28 weeks of gestation over the first 5 years of their lives in terms of
physical growth, medical and neurological complications, and developmental outcome. The
preliminary evaluation at 24 months corrected
age was presented earlier in abstract form.11
Materials and Methods
Patient Population
Infants delivered at the SMBD-Jewish General
Hospital, a tertiary care perinatal center, between 1987 and 1994 were eligible for the study
if they were born before 28 weeks of gestation.
The gestational age was calculated from the last
menstrual period and from ultrasonography
performed between 16 and 18 weeks of gestation. If there was a discrepancy greater than 1
week between the two determinations, ultrasound dating was taken as reference. Infants
with significant congenital or chromosomal
anomalies as well as those with congenital viral
infections were excluded. Infants were classified
as SGA if their birth weight was below or at the
Seminars in Perinatology, Vol 28, No 4 (August), 2004: pp 288-294
SGA and AGA Infants Follow-Up
3rd percentile, using the Usher and McLean
grid of intrauterine growth, constructed from
infants born in the province of Quebec and
extrapolated to 24 weeks.12
Eighty-six SGA and 318 AGA infants satisfied
the criteria described above. Of those, 46 (53%)
SGA and 241 (76%) AGA infants survived and
were available for follow-up (P ⬍ 0.0001).
Study Design
The 46 SGA survivors were matched with 46
AGA survivors according to gender, gestational
age within 2 days, and delivery date within 12
months to account for possible changes in neonatal care. Of the initial cohort of 46 SGA–AGA
dyads that had a full evaluation at 24 months of
corrected age, 37 dyads (80%) completed the
evaluation at 5 years of age. The perinatal data
and evaluation at 24 months of those children
who did not complete the 5-year evaluation were
similar to those of the study cohort.
Outcome Variables
Information pertaining to the pregnancy, the
delivery, and the NICU stay was collected from
the mothers’ and infants’ charts.
Infants were seen at regular intervals in the
neonatal follow-up clinic: at 3, 6, 12, and 24
months of corrected age, and yearly thereafter.
The following outcome measures were collected
from the follow-up charts:
• Medical history
• Social history
• Anthropometric measurements were plotted
on standard growth curves for boys and girls and
expressed as Z-scores. Microcephaly was defined
as head circumference below the 5th percentile
for age corrected gestation.
• Physical and neurological assessment was performed by a developmental pediatrician. Hearing screening was performed at 3 months corrected age using auditory brainstem response,
with further audiologic evaluation as needed.
Vision screening was performed at about 12
months corrected age and before school entry.
• The Griffith Mental Developmental Scale administered by trained personnel was used at 6,
12, and 24 months corrected age and the Stanford-Binet Index at 5 years. If the developmental
289
pediatrician judged it necessary, the children
were also referred and evaluated by a pediatric
psychologist between 3 and 5 years of age, unaware of the child’s medical history.
Children were classified as normal if they had
a normal neurodevelopmental evaluation at age
5 years. In the normal group were included infants with amblyopia, refractive errors, mild
hearing deficit, or speech delay not requiring
therapy. Children were classified as having mild
to moderate neurodevelopmental impairment if
they had mild to moderate cognitive deficit, seizure disorder, abnormal neurological examination but not cerebral palsy, behavior disturbance, and speech delay requiring therapy.
Children were considered as having a severe
impairment if they had cerebral palsy, legal
blindness defined as severe visual impairment
meeting the criteria for state compensation,
hearing loss requiring hearing aids, or severe
mental retardation.
A child was diagnosed as having global delay
if he/she had a deficit in more than one sphere
of development.
Statistical Analysis
The data were analyzed by using the Graph Pad
InStat Software. Differences on categorical variables were analyzed by 2 statistics or Fisher’s
exact test if cell sizes were less than 5. Student’s
t test was used for continuous variables. MannWhitney U-statistic was used for nonparametric
data. A P value ⬍0.05 was considered significant.
Results
Population Profile
There were 11 boys and 26 girls in each study
group of SGA and AGA infants. Each group had
a mean gestational age of 26 ⫾ 1.2 weeks, with a
birth weight of 638 ⫾ 77 g for the SGA infants
and 833 ⫾ 134 g for the AGA infants (P ⬍
0.0001). SGA infants also had a lower mean
length (32.7 ⫾ 1.8 versus 33.8 ⫾ 2.6) and head
circumference (23.0 ⫾ 1.3 versus 23.8 ⫾ 0.5)
than the AGA infants, but the means were above
the 3rd percentile for gestational age. There was
a greater incidence of preeclampsia in the mothers of SGA infants, and these infants were more
depressed at birth. The SGA infants required
290
Bardin, Piuze, and Papageorgiou
significantly longer ventilatory support (53 versus 32 days for AGA infants, P ⬍ 0.05) and
oxygen supplementation (82 versus 55 days for
AGA infants). At a postmenstrual age of 36
weeks, 22 SGA and 8 AGA infants were still
oxygen-dependent. The incidence of intraventricular hemorrhage (IVH), of periventricular
leukomalacia (PVL), and ventricular dilation
were similar in the two groups. Retinopathy of
prematurity (ROP) was more frequent and severe in the SGA group. Twenty SGA infants had
stage ⱖIII ROP versus only 2 AGA infants.
Growth Pattern
The growth parameters for the two groups, from
3 months corrected age until 5 years, are presented in Figs 1, 2, and 3. The AGA children
caught up in weight and length by 5 years of age
(z-score ⫽ 0). The SGA children remained
lighter and shorter than the AGA children.
Their growth curves paralleled those of the AGA
infants, but at a lower z-score, and did not
catch-up to a z-score of 0 by age 5 years.
The head circumference z-score for both SGA
and AGA children declined during the first 24
months, followed by stabilization, and mild improvement. However, the head circumference
curve for the SGA children remained below that
of the AGA children. At 5 years of age, 38% of
SGA children and 16% of AGA children had
microcephaly. We also noted that severe retinopathy of prematurity (Stage ⱖIII) was associated
Figure 1. Weight at 3 and 24 months corrected age
and at 60 months expressed as mean Z-score. Change
over time.
Figure 2. Length at 3 and 24 months corrected age
and at 60 months expressed as mean Z-score. Change
over time.
with poor head growth. Overall, 10/22 (45%)
children with severe ROP had microcephaly.
Medical Health
Following discharge from the NICU, the medical and surgical problems of the two groups were
practically similar, as indicated in Table 1. More
than 50% of children SGA and AGA required
hospitalization at least once during the first 2
years of life, the main indications being respiratory (bronchiolitis, pneumonia, reactive airway
disease) and surgical (minor surgical proce-
Figure 3. Head circumference at 3 and 24 months
corrected age and at 60 months expressed as mean
Z-score. Change over time.
291
SGA and AGA Infants Follow-Up
Table 1. Medical Health during the First 5 Years
of Life
Need for Rehospitalization
0-24 months
2-5 years
Asthma/Reactive Airway
Disease
0-24 months
2-5 years
Otitis Media
0-24 months
2-5 years
SGA
(n ⫽ 37)
AGA
(n ⫽ 37)
19 (51%)
6 (16%)
22 (59%)
4 (11%)
9 (24%)
9 (24%)
7 (19%)
11 (30%)
24 (65%)
14 (38%)
23 (62%)
15 (41%)
dures: hernia repair, placement of pressureequalizing [PE] tubes). Between 2 and 5 years of
age, the incidence of otitis media and the need
for rehospitalization dropped significantly in
both groups. However, the incidence of reactive
airway disease, which was also similar in both
groups, has not declined after the second year of
life.
Neuro-Sensory Outcome (Table 2)
Dystonia, defined as abnormality in muscle tone,
was frequently diagnosed during the first year of
life, and more so in the SGA group, 67% versus
43% for the AGA group. At 24 months, 7 SGA
(19%) and 3 AGA (8%) children had been assigned the diagnosis of cerebral palsy, a finding
confirmed at 5 years of age. Among the SGA
children, 1 had spastic quadriplegia, 5 had spastic diplegia, and 1 had hemiplegia. In the AGA
group, there was 1 child with spastic quadriplegia and 2 children with spastic diplegia.
Eleven SGA (30%) and 8 AGA (22%) children had refractory errors requiring correction.
Severe visual deficit (legal blindness) was diagnosed in 3 SGA (8%) and 1 AGA (3%) children.
Hearing deficit affected 5 SGA (14%) and 3
AGA (8%) children, with two in each group
requiring the use of hearing aids. At 5 years, 11
SGA (30%) and 9 AGA children (24%) were
diagnosed with speech delay.
General Developmental Index (Table 3)
Both the mean and the median General Developmental Index (GDI) decreased over the observation period for both the SGA and AGA
Table 2. Neurosensory Outcomes at 5 Years of Age
Cerebral Palsy
Spastic quadriplegia
Spastic diplegia
Hemiplegia
Vision
Legal blindness
Other visual impairment
Hearing
Hearing aids
Hearing deficit
SGA
(n ⫽ 37)
AGA
(n ⫽ 37)
1 (2.7%)
5 (13.5%)
1 (2.7%)
1 (2.7%)
2 (5.4%)
0
3 (8.1%)
11 (29.7%)
1 (2.7%)
3 (8.1%)
2 (5.4%)
5 (13.5%)
2 (5.4%)
3 (8.1%)
children without much change in the range of
GDI.
Neuro-Developmental Outcome (Table 4)
Twenty-two SGA (59%) and 26 AGA (70%) children were evaluated to be developing normally
at 5 years of age, without any deficit. Among the
7 SGA children with mild to moderate impairment, 1 child had mild to moderate global delay,
3 had features of hyperactivity, 2 had mild cognitive delay, and 1 had abnormal behavior and
speech delay. In the AGA group, 6 children had
mild-moderate impairment: one had moderate
global delay and 5 had features of hyperactivity.
Eight SGA and 5 AGA children were classified
as being severely impaired. The mildest case in
the SGA group had cerebral palsy and hyperactivity features. The other SGA children had multiple severe deficits and handicaps. Generally,
the severity in the AGA group was less pronounced than that in the SGA group: 1 child was
blind, but otherwise normal, 1 had behavior
problems with hearing aids and speech delay, 1
Table 3. General Development Index (GDI):
Change over Time
Mean
SGA
AGA
Median
SGA
AGA
Range
SGA
AGA
6 months
12 months
24 months
5 years
102 ⫾ 7
103 ⫾ 7
95 ⫾ 7
97 ⫾ 7
94 ⫾ 4
96 ⫾ 4
90 ⫾ 6
92 ⫾ 5
103
103
96
97
95
97
91
94
77-110
78-115
77-112
80-121
75-110
78-115
68-105
70-110
292
Bardin, Piuze, and Papageorgiou
had cerebral palsy and speech delay, 1 had severe development delay with cerebral palsy, and
1 had mild developmental delay with hearing
aids and speech delay.
In view of the significant increase in the number of children with microcephaly over time, we
also examined the effect of microcephaly on the
overall assessment of SGA and AGA children.
As shown in Table 5, inappropriate head
growth was associated with abnormal development, both in SGA and AGA children. Among
the 20 children with microcephaly, 14 (70%)
had developmental delay, of which 8 (40%) had
severe impairment and 6 (30%) had mild to
moderate impairment. Only 6 (30%) children
were considered to have normal development.
In contrast, among the 54 children with normal
head growth, 11 (20%) had developmental delays, of whom 5 (9%) had severe impairment
and 6 (11%) had mild-moderate impairment.
The same Table indicates the incidence of severe ROP among infants with head circumference below or above the 5th percentile in the
neonatal period.
Discussion
Premature infants born SGA form a group of
infants at greater risk for severe perinatal morbidities when compared with AGA infants of
similar gestational age. The data of the present
cohort are in line with our earlier observations
on SGA infants born ⬍27 weeks of gestation,10 as
well as with those more recently published.13-15
Our follow-up to 5 years of age shows that the
overall growth of SGA children remains suboptimal, with only mild catch-up in length, when
compared with the AGA children. The SGA children as a group remain smaller in all dimensions
compared with children born AGA. Gutbrod
and coworkers,16 reported similar findings for
SGA and AGA children born at an average gestational age of 32 weeks. Similar findings have
Table 4. Neurodevelopmental Assessment
Normal
Mild-moderate impairment
Severe impairment
SGA
(n ⫽ 37)
AGA
(n ⫽ 37)
22 (59%)
7 (19%)
8 (22%)
26 (70%)
6 (16%)
5 (14%)
also been reported for term SGA infants.8,17,18
The SGA–AGA difference may be explained in
part by the chronic intrauterine hypoxic state of
the SGA infants, which may have altered their
potential for future growth, and in part by their
more difficult neonatal course.
Compared with the standard term population, SGA children experience only minimal
catch-up in weight, while AGA children reach a
z-score of 0 by 5 years of age. Although height
significantly improved in both groups, especially
over the first 2 years of life, AGA children did
attain the 0 z-score, while SGA attained a score
of – 0.5. However, of greater concern is the decline in head circumference z-scores in both
SGA and AGA children over the first 2 years of
life, without significant recovery. At 5 years, 38%
of SGA and 16% of the AGA children had a head
circumference below the 5th percentile. We
could not correlate this observed decline in
head growth with the use of either antenatal or
postnatal steroids, nor could we explain the decline in on the basis of postnatal nutritional
factors. Recently, Brandt and coworkers19 suggested that head catch-up growth may be promoted by high-energy nutrient intakes in the
first days of life. Overall, only 22/37 (59%) SGA
children exceeded the 5th percentile on all
three growth parameters at 5 years, compared
with 30/37 (81%) AGA children. Our data on
SGA children are in agreement with the results
of Monset-Couchard and de Bethmann for SGA
children of birth weight under 1000 g.20 Sixtyfive percent of them had catch-up growth in all
three growth parameters at a median age of 9
years.
In terms of general health, because the SGA
children had a higher incidence of chronic lung
disease (59% versus 21% for AGA), we would
have expected a greater incidence and severity
of reactive airway disease or asthma in early
childhood, as compared with the AGA children.
This was not the case, as also was suggested by
Amin and coworkers.8 It is reassuring to see that
the need for hospitalization decreased dramatically after the first 2 years of life, as also noted by
Yu and coworkers.21The incidence of visual impairment was higher among SGA infants (Table
2) as was the incidence of severe ROP during the
neonatal period, an observation also reported
previously.11
When we evaluated the neurological out-
293
SGA and AGA Infants Follow-Up
Table 5. Microcephaly (HC ⬍5TH percentile)
Delayed Development
Severe ROP (Stage ?III)
HC ⬍5th Percentile (n ⫽ 20)
HC ⬎ 5th Percentile (n ⫽ 54)
P
14 (70%)
11 (55%)
11 (20%)
11 (20%)
0.0002
0.008
come, we found that the deficits were greater in
the SGA children, despite a similar baseline incidence of IVH and PVL. There are conflicting
reports in the literature on the incidence of
cerebral palsy in SGA children. A large European study5 reported an increased incidence of
cerebral palsy in SGA children, especially in infants born after 32 weeks of gestation, but not so
clearly in those born before 32 weeks. Similar
findings were presented by Latal and coworkers,22 using a cutoff point for SGA at the 10th
percentile. Hutton and coworkers9 and Veelken
and coworkers23 suggest that CP in very premature SGA children is related to prematurity and
not to weight at birth. However, Hutton concludes that intrauterine growth restriction is a
risk factor for minor neurological abnormalities
independent of gestational age.
Five of our six SGA children with cerebral
palsy had a head circumference below the 5th
percentile. This association of CP and small
head circumference has also been described by
Watemberg and coworkers.24
The General Developmental Index and IQ
were not different between the two groups of
children when the severely affected children in
both groups were excluded. Hutton and coworkers,9 in a group of children born ⬍32 weeks
gestation, concluded that the intellectual quotient (IQ) was positively correlated with birth
weight ratio. Robertson4 described similar academic performance, once children with disabilities were excluded, but noted more hyperactive
behavior among SGA children.
The negative effect of subnormal head
growth on cognitive ability has been extensively
reported in the literature.3,19,25-27 More recently,
Peterson and coworkers28 reported on the negative effect of reduced brain volume on neurodevelopmental outcome at 20 months corrected
age among prematurely born infants.
Finally, it appears that the overall neurodevelopmental delay among SGA children is more
severe than that of AGA children. This is in
keeping with previously published data.3 How-
ever, in contrast, Amin and coworkers8 did not
find differences in major neurodevelopmental
disabilities at age 3 years between SGA and AGA
children of mean gestational age of 30 weeks.
Conclusion
At 5 years of age, children born SGA and extremely premature, are at higher risk for neonatal and childhood difficulties compared with
AGA children of similar gestational age. Overall,
at 5 years of age, very premature children born
SGA remain smaller in all growth parameters
than their AGA counterparts. They tend to exhibit more neurodevelopmental deficits (41%
versus 30%) and severe handicaps, including
CP, blindness, deafness, and mental retardation
(22% versus 14%). Those deficits are seen predominantly in association with microcephaly,
which is more prevalent in the SGA group.
References
1. Markestad T, Vik T, Ahlsten G, et al: Small-for-gestational-age (SGA) infants born at term: Growth and development during the first year of life. Acta Obstet Gynecol
Scand Suppl 165:93-101, 1997
2. Ruys-Dudok van Heel I, de Leeuw R: Clinical outcome of
small for gestational age preterm infants. J Perinat Med
17:77-83, 1989
3. McCarton CM, Wallace IF, Divon M, et al: Cognitive and
neurological development of the premature, small for
gestational age infant through age 6: Comparison by
birth weight and gestational age. Pediatrics 98:11671178, 1966
4. Robertson CMT, Etches PC, Kyle JM: Eight-year school
performance and growth of preterm, small for gestational age infants: A comparative study with subjects
matched for birth weight or for gestational age. J Pediatr
116:19-26, 1990
5. Jarvis S, Glinianaia SV, Torrioli MG, et al: Cerebral palsy
and intrauterine growth in single births: European collaborative study. Lancet 362:1106-1111, 2003
6. Pena IC, Teberg AH, Finello KM: The premature small
for gestational age infant during the first year of life:
comparison by birth weight and gestational age. J Pediatr 113:1066-1073, 1988
7. Sung IK, Vohr B, Oh W: Growth and neurodevelopmental outcome of very low birth weight infants with intra-
294
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
Bardin, Piuze, and Papageorgiou
uterine growth retardation: Comparison with control
subjects matched by birth weight and gestational age.
J Pediatr 123:618-624, 1993
Amin H, Singhal N, Sauve RS: Impact of intrauterine
growth restriction on neurodevelopmental and growth
outcomes in very low birth weight infants. Acta Paedriatr
86:306-314, 1997
Hutton JL, Pharoah POD, Cook RWI, et al: Differential
effects of preterm birth and small gestational age on
cognitive and motor development. Arch Dis Child Fetal
Neonatal Ed 76:F75-F81, 1997
Bardin C, Zelkowitz P, Papageorgiou A: Comparison of
outcomes of SGA and AGA infants born between 24 and
27 weeks gestation. Pediatrics 100:1-5, 1997
Bardin C, Papageorgiou A: The first two years of life of
SGA infants born ⬍28 weeks of gestation. Pediatr Res
41:191A, 1997
Usher R, McLean F: Intrauterine growth of live born
Caucasian infants at sea level: Standards obtained from
measurements in 7 dimensions of infants born between
25 and 44 weeks of gestation. J Pediatr 74:901-910, 1969
Regev RH, Lusky A, Dolfin T, et al: Excess mortality and
morbidity among small for gestational age premature
infants: A population-based study. J Pediatr 143:186-191,
2003
Lal MK, Manktelow BN, Draper ES, et al: Chronic lung
disease of prematurity and intrauterine growth retardation: a population-based study. Pediatrics 111:483-487,
2003
Zaw W, Gagnon R, da Silva O: The risk of adverse
neonatal outcome among preterm small for gestational
age infants according to neonatal versus fetal growth
standards. Pediatrics 111:1273-1277, 2003
Gutbrod R, Wolke D, Soehne B, et al: Effects of gestation
and birth weight on the growth and developments of
very low birth weight small for gestational age infants: A
matched group comparison. Arch Dis Child Fetal Neonatal Ed 82:F208-F214, 2000
Hediger ML, Overpeck MD, Maurer KR, et al: Growth of
infants and young children born small or large for gestational age: Findings from the Third National Health
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
and Nutrition Examination Survey. Arch Pediatr Adolesc
Med 152:1225-1231, 1998
Strauss RS, Dietz WH: Effects of intrauterine growth
retardation in premature infants on early childhood
growth. J Pediatr 130:95-102, 1997
Brandt I, Sticker EJ, Lentze MJ: Catch-up growth of head
circumference of very low birth weight, small for gestational age preterm infants and mental development to
adulthood. J Pediatr 142:463-468, 2003
Monset-Couchard, de Bethmann O: Catch-up growth in
166 small for gestational age premature infants weighing
less than 1000 g at birth. Biol Neonate 78:161-167, 2000
Yu VY, Manlapaz ML, Tobin J, et al: Improving health
status in extremely low birth weight children between
two and five years. Early Hum Dev 30:229-239, 1992
Latal-Hajanl B, Von Sieventhal K, Kovari H, et al: Postnatal growth in VLBW infants: Significant association
with neurodevelopmental outcome. J Pediatr 143:163170, 2003
Veelken N, Stollhoff K, Claussen M: Development and
perinatal risk factors of very low birth weight infants.
Small versus appropriate for gestational age. Neuropediatrics 23:102-107, 1992
Watemberg N, Silver S, Lerman-Sagie T: Significance of
microcephaly among children with developmental disabilities. J Child Neurol 18:117-122, 2002
Hack M, Breslau N, Weissman B, et al: Effect of very low
birth weight and subnormal head size on cognitive abilities at school age. N Engl J Med 325:231-237, 1991
Frisk V, Amsel R, Whyte HE: The importance of head
growth patterns in predicting the cognitive abilities and
literacy skills of small for gestational age children. Dev
Neuropsychol 22:565-593, 2002
Wood NS, Marlow N, Costeloe K, et al: Neurological and
developmental disability after extremely preterm birth.
N Engl J Med 343:378-384, 2000
Peterson BS, Anderson AW, Ehrenkranz R, et al: Regional brain volumes and their later neurodevelopmental correlates in term and preterm infants. Pediatrics
111:939-948, 2003