Journal of Perinatology (2006) 26, 93–99
r 2006 Nature Publishing Group All rights reserved. 0743-8346/06 $30
www.nature.com/jp
ORIGINAL ARTICLE
New insights into spontaneous intestinal perforation using a
national data set: (1) SIP is associated with early indomethacin
exposure
JT Attridge1, R Clark2,4, MW Walker2,3 and PV Gordon1,4
1
University of Virginia Children’s Hospital, Charlottesville, VA, USA; 2Pediatrix Medical Group Inc., Sunrise, FL, USA and 3The
Children’s Hospital, Greenville Hospital System, Greenville, SC, USA
Background: Spontaneous intestinal perforation (SIP) is increasingly
common in the premature infant and is associated with significant
morbidity. Indomethacin use has been implicated as a co-risk factor for SIP
when combined with glucocorticoids, but previous evidence argued against
indomethacin being an independent risk factor when used prophylactically.
Objectives: (1) To establish a homogeneous cohort of SIP patients in a
national data set and to contrast them to patients with surgical
necrotizing enterocolitis (NEC). (2) To test the hypothesis that early postnatal indomethacin is independently associated with SIP.
Methods: A large de-identified data set was retrospectively queried by
diagnosis, and then multiple antenatal and post-natal variables were
tested by both univariate and multivariate analysis to identify associations
with SIP. Sub-analyses were also performed to look at the timing of drug
administration.
Results: There were 2105 patients evaluated in the data set. Patients
were divided into matched controls (n ¼ 581), those with SIP without
report of NEC (n ¼ 633) and those with NEC requiring surgery
(n ¼ 891). Infants with SIP were more likely to have a patent ductus
arteriosus and more likely to be treated with vasopressors than either
control or NEC patients. Compared to infants with NEC, patients with SIP
were smaller, less mature and required more support. SIP was also
diagnosed earlier than NEC (median of 7 vs 15 days). Patients with SIP
were more likely to be treated with indomethacin, hydrocortisone or both
on days of life 0–3 than controls.
Conclusions: (1) Surgical NEC and SIP have significant differences in
presentation, demographics and morbidity. (2) A detailed look at drug
timing revealed that early post-natal indomethacin is independently
associated with SIP.
Correspondence: Dr PV Gordon, University of Virginia, Box 800386, Charlottesville, VA 22908,
USA.
E-mail address: pvg4n@virginia.edu
4
These authors contributed equally to the design, oversight and publication of this project,
and should be considered co-senior authors for the purpose of citation.
Received 15 August 2005; revised 18 October 2005; accepted 21 October 2005; published online
1 December 2005
Journal of Perinatology (2006) 26, 93–99. doi:10.1038/sj.jp.7211429;
published online 1 December 2005
Keywords: steroids; neonate; necrotizing enterocolitis; intestinal
perforation; indomethacin
Introduction
Spontaneous intestinal perforation (SIP), also known as focal
small bowel perforation, is an acquired form of neonatal bowel
disease that is distinct from necrotizing enterocolitis (NEC) and has
been documented within the low-birth-weight population for over
20 years.1–4 Despite this history, distinguishing SIP from NEC in
large clinical databases has not been straightforward and there
have been no previous examinations of SIP that use a nationally
available neonatal database. We sought to accomplish this in the
Pediatrix Medical Group (Pediatrix) community by making the
diagnostic categories of SIP and NEC mutually exclusive within its
electronic administrative database. Our purpose was twofold: first,
to test the hypothesis that SIP and NEC are significantly different in
their demographics, presentation and outcomes, and second, to
create a database large enough for complex analyses of risk factors.
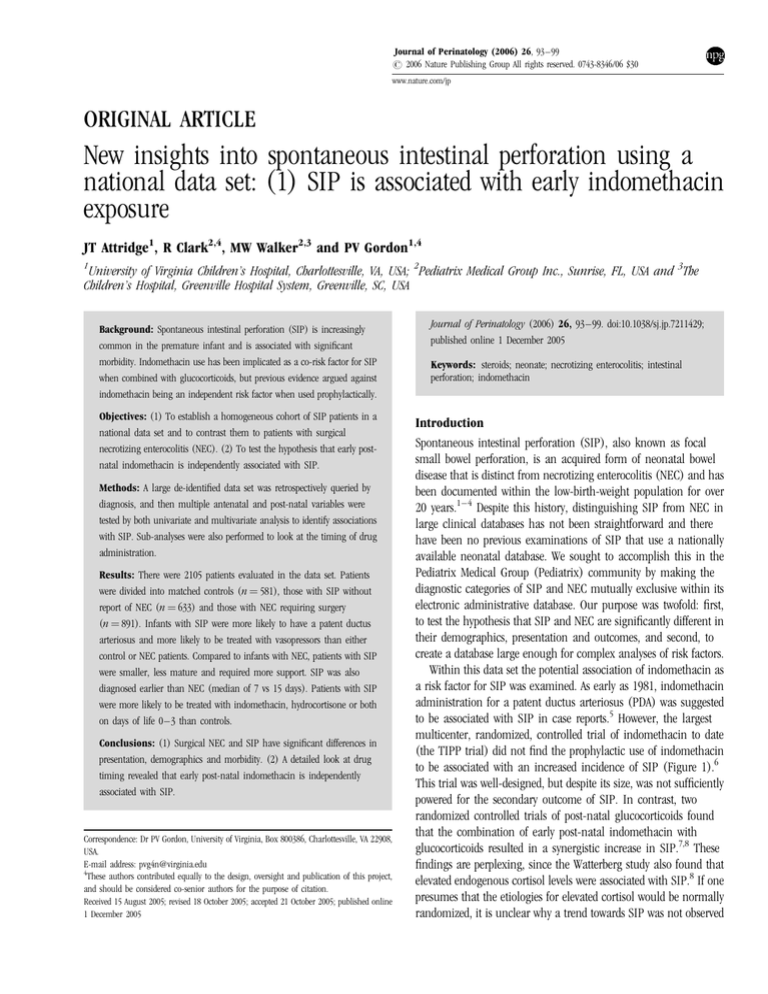
Within this data set the potential association of indomethacin as
a risk factor for SIP was examined. As early as 1981, indomethacin
administration for a patent ductus arteriosus (PDA) was suggested
to be associated with SIP in case reports.5 However, the largest
multicenter, randomized, controlled trial of indomethacin to date
(the TIPP trial) did not find the prophylactic use of indomethacin
to be associated with an increased incidence of SIP (Figure 1).6
This trial was well-designed, but despite its size, was not sufficiently
powered for the secondary outcome of SIP. In contrast, two
randomized controlled trials of post-natal glucocorticoids found
that the combination of early post-natal indomethacin with
glucocorticoids resulted in a synergistic increase in SIP.7,8 These
findings are perplexing, since the Watterberg study also found that
elevated endogenous cortisol levels were associated with SIP.8 If one
presumes that the etiologies for elevated cortisol would be normally
randomized, it is unclear why a trend towards SIP was not observed
Insight into spontaneous intestinal perforation
J Attridge et al
94
Figure 1 Graph of odds ratios for SIP with indomethacin or
indomethacin þ glucocorticoids in three prospective multicenter,
randomized, controlled trials. The TIPP trial (Schmidt et al.6)
demonstrates no effect of prophylactic indomethacin (n ¼ 68 cases of
SIP/1202 total enrollment). The NICHD trial (Stark et al.7)
demonstrates a significant effect with indomethacin and dexamethasone, both given within the first 24 h of life (n ¼ 18 cases of SIP/220
total enrollment). The PROPHET trial (Watterberg et al.8) demonstrates
a significant effect with indomethacin and early post-natal
hydrocortisone (n ¼ 21 cases of SIP/360 total enrollment). Sixty-three
percent of all indomethacin was given within the first 48 h within the
PROPHET trial. The odds ratios for the TIPP trial are the same as
published. The odds ratios for the NICHD and PROPHET trials are
calculated based on comparison cohorts created by combining patients
treated with study drug and indomethacin against all other study
patients.
in the TIPP trial. We hypothesized that an independent association
between early post-natal indomethacin and SIP would be detected
in our data set, which contains a larger SIP cohort than all
currently published reports of SIP.
Methods
The de-identified administrative data set
Clinical data on these neonates were recorded during the time that
care was provided in the NICU (as described previously).9
Admission, discharge and daily progress notes were generated using
a computer-assisted tool, and the data were stored in an electronic
database. These data were then consolidated within the Pediatrix
data warehouse where they were de-identified, made HIPAA
compliant and configured into tables that could be joined and
queried for statistical analyses. The use of the data reported here
and certification of the data as de-identified was approved by the
University of Virginia Human Investigation Committee
(Charlottesville, VA, USA) and the Wichita Medical Research and
Education Foundation (Wichita, KS, USA).
Data on estimated gestational age represented the best estimate
based on both obstetrical data and neonatal examination. Data on
mother’s race were based on the options contained in the database:
white, black, Hispanic, Native American and Asian populations.
The study cohort
A retrospective cohort of neonates from the Pediatrix de-identified
administrative data set was assembled in order to compare
neonates diagnosed with intestinal perforation to a control group.
This was accomplished by searching for all reports of ‘NEC’,
‘perforated bowel’, ‘ileal perforation’ and/or ‘isolated perforation
Journal of Perinatology
Figure 2 Schematic demonstrating our cohort selection strategy for
SIP and surgical necrotizing enterocolitis (NEC). The control cohort
was matched for weight (within 40 g, 0.02 to þ 0.02), gestational
age and gender with that of the SIP cohort. Not shown are 59 gastric
perforations in our database, which were excluded from this study.
of the bowel’ within specific tables: ‘Patients’, ‘Admissions’,
‘Medications’ and ‘Diagnoses’. Based on this search, each patient
was assigned to one of four diagnostic groups: isolated or ileal
perforation with no report of NEC (generally diagnosed by surgical
record), perforated bowel with no report of NEC, NEC with
perforation and NEC with a report of surgical treatment (see
Figure 2).
Statistical evaluation of these groups showed that neonates with
isolated and ileal perforations, and those with bowel perforation but
no report of NEC were statistically the same for each of the
demographic and treatment characteristics we describe (data not
shown). Similarly, neonates with NEC that required surgical
intervention were very similar to neonates with NEC and a report of
perforation. It became apparent that a third distinctive group of
neonates was present in the data set – those with bowel perforation
and a report of a major anomaly. These patients were excluded
from subsequent analyses.
A control group was identified to define the risk factors
associated with isolated bowel perforation by matching a random
sample of controls to the patients with a report of isolated or ileal
perforations. Patients were matched by gestational age, birth weight
(within 40 g, 0.02 to þ 0.02) and gender. This matching
algorithm was designed to allow us to evaluate the effect of medical
intervention on the occurrence of bowel perforations.
To evaluate the use of medications previously reported to be
associated with bowel perforation,8,10–14 the ‘Medications’ table
was queried for any report of ‘hydrocortisone’, ‘dexamethasone’ or
‘indomethacin’ within each of the first 14 days of life in both
control and perforation cohorts to look at each day of exposure.
Insight into spontaneous intestinal perforation
J Attridge et al
95
This search strategy allowed us to compare the drug exposures
antecedent to perforation and to compare them with the matched
control cohort within discrete windows of exposure. For early
(defined as 0–3 days of life) and intermediate (4–7 days of life)
windows of drug exposure, direct comparisons were performed
(e.g., 0–3 days vs 0–3 days and 4–7 days vs 4–7 days) as the
cohorts remained comparable in size (with the intermediate
window losing 20% of the SIP cohort due to incidence of
perforations in the early window). However, for our 2-week
exposure window, there was no time of diagnosis to retrospectively
search from in the control group. Had we simply started at day 0 in
the SIP cohort, we faced the issue of increasing patient drop-out
(statistical censoring of data). To address these issues, we employed
the following strategy: for the control group, days of life 0–14 were
queried for a report of the medications of interest, and for the SIP
group, the 14-day window prior to diagnosis was queried (or back
until day of life 0). Fourteen days was chosen after examining the
distribution of SIP diagnosis. Two standard deviations worth of SIP
occurred within 0–14 days, thus providing a well-matched
temporal overlap between the two cohorts and blanketing the
clinical window during which SIP is most prevalent.
Univariate analysis
Study populations were compared using both univariate and
bivariate techniques. Continuous variables (estimated gestational
age and birth weight) were evaluated with two-tailed t-tests.
Categorical variables (e.g., race and gender) were evaluated with a
two-tailed w2 test. Nonparametric continuous data were assessed
with a Kruskal–Wallis analysis of variance.
Multivariate analysis
After univariate analysis, multivariate logistic regression was used
to identify factors independently associated with a diagnosis of SIP
without NEC (patients with perforation compared to matched
controls). The demographic variables found by univariate analysis
to be significantly different for the two groups (P<0.1) were used
in the logistic regression analysis. Variables were entered into the
model with a stepwise selection (P-value for entry and retention
<0.1). Multivariate analysis was also used to assess for
independence between drugs that were found to be associated with
a diagnosis of SIP when given within the same treatment window.
Results
Creation of the data set
Between January 1, 1996 and June 1, 2004, care was provided by
clinicians affiliated with Pediatrix to 227 711 neonates (see
Electronic Supplement A). Using search techniques, we identified
1779 patients with a report of perforation or NEC treated surgically.
Neonates with reports of gastric perforation and major congenital
anomalies (n ¼ 255) were excluded. Major anomalies associated
with a report of bowel perforation were heart anomalies (n ¼ 61),
cystic fibrosis (n ¼ 26), gastroschisis (n ¼ 23), intestinal atresia
(n ¼ 23), Hirschsprung disease (n ¼ 13), chromosomal
abnormality (n ¼ 14), multiple congenital anomalies (n ¼ 11),
galactosemia (n ¼ 7), hydrops fetalis (n ¼ 7), omphalocele
(n ¼ 4), thalassemia (n ¼ 4) and diaphragmatic hernia (n ¼ 3).
These exclusions left a total of 1524 patients with perforations.
There was no significant change in the combined reported
incidence of acquired bowel disease (i.e., there was no change in
the incidence of the sum of cases of NEC and SIP) over time and
there was no significant change in the reported incidence of cases
(NEC or perforated bowel without NEC) over time (Electronic
Supplement A). However, there was an increase in the use of the
term, ‘isolated perforation’, and a decrease in the use of the terms,
‘bowel perforation with no report of NEC’, over time (data not
shown).
Comparison of SIP to matched control and NEC cohorts
(Table 1 and Electronic Supplement B)
When compared to matched controls for demographic variables,
neonates with SIP were more often outborn, less often received
antenatal steroids; more often reported to have had a PDA and be
treated for it, and more likely to have received vasopressor support.
Infants with SIP also had significantly higher mortality than
matched controls.
When compared to neonates with surgical NEC, infants with SIP
were smaller and more immature, were diagnosed earlier in life
(median age ¼ 7 vs 15 days), were more often diagnosed with a
PDA requiring treatment and were more likely to have received
surfactant vasopressors and assisted ventilation. Infants with NEC
also had significantly higher mortality than infants with SIP. When
compared to control patients (all variables in Table 1 and
Electronic Supplement B evaluated), the factors found in
multivariate analysis to be independently associated with SIP were
being outborn, a report of a PDA as a diagnosis, a report of the use
of pressors within 14 days of birth (controls) or within 14 days of
the diagnosis of SIP (Table 2).
Analysis of pharmacologic variables between SIP and controls
Associations between SIP and individual drug interventions were
assessed in four separate treatment windows between the control
and SIP cohorts (Table 3A): antenatal, day of life 0–3, day of life
4–7 and day of life 0–14 for control vs 14 days prior to diagnosis
for SIP. In the antenatal window, we were only able to derive
antenatal steroids by report, but there was a significant reduction
in antenatal steroid exposure in the SIP cohort when compared to
controls. In the early window (days of life 0–3), indomethacin and
hydrocortisone were both found to be associated with SIP by
univariate analysis. This association did not hold true for either
indomethacin or hydrocortisone when comparing exposure during
days of life 4–7. Within the 14-day windows, infants with SIP were
Journal of Perinatology
Insight into spontaneous intestinal perforation
J Attridge et al
96
Table 1 Demographic and discharge data
Variable
Control (Cont)
Perforation (SIP)
26
0.83
0.04
5
8
39
129
198
509
Race, n (%)
Black
Hispanic
White
131 (23.1)
118 (20.8)
298 (52.6)
140 (22.9)
126 (20.6)
307 (50.2)
241 (28.5)
218 (25.8)
340 (40.2)
Delivered by C-section, n (%)
351 (60.6)
379 (60.1)
494 (55.9)
Discharge type, n (%)
Died
Home
Transfer
Transfer of service
93
377
81
28
(16.1)
(65.1)
(14)
(4.8)
137
322
123
49
(21.7)
(51)
(19.5)
(7.8)
316
385
147
43
(35.5)
(43.2)
(16.5)
(4.8)
X
Y
(0–8.5)
(49–92.5)
(0–49)
(2–75.3)
17
92.5
12
78
(10–31.5)
(66–117)
(4–59)
(30–104.5)
27
96
34
105
(15–47.5)
(65–123)
(13–94)
(48–139)
X
X
2
72
16
16
Table 2 Factors independently associated with SIP (SIP vs matched
controls)
Variable
Odds ratio (CI)
P-value
Outborn
Report of PDA
Dopamine or dobutaminea
2.34 (1.7–3.2)
1.52 (1.1–2.0)
1.47 (1.1–1.9)
<0.0001
0.0032
0.0041
Early treatment (0–3 days)
Indomethacin
Hydrocortisone
1.86 (1.4–2.5)
1.77 (1.2–2.8)
<0.0001
0.0113
CI ¼ confidence interval; PDA ¼ patent ductus arteriosus.
a
Reported within first 14 days after birth for control and within 14 days of diagnosis for
SIP group.
again more often exposed to indomethacin and to hydrocortisone.
Finally, the pharmacologic factors found in multivariate analysis to
be independently associated with SIP (when compared to control
patients) were use of pressors within 14 days prior to the diagnosis
Journal of Perinatology
26
0.81
0.02
5
7
40
136
220
473
633
(24–28)
(0.67–1.05)
(0.68 to 0.64)
(3–7)
(6–9)
(6.4)
(23.8)
(34.8)
(75.1)
27
0.94
0.16
6
8
43
197
346
667
891
(25–30)
(0.71–1.35)
(0.9 to 0.5)
(3–7)
(6–9)
(4.9)
(24.6)
(38.8)
(74.9)
SIP vs Cont
Number of patients, n
Estimated gestational age (weeks), median (25th–75th percentile)
Birth weight (kg), median (25th–75th percentile)
Birth weight Z-score, median (25th–75th percentile)
Apgar score at 1 min, median (25th–75th percentile)
Apgar score at 5 min, median (25th–75th percentile)
Apgar score at 5 min p3, n (%)
Multiple gestation, n (%)
Female, n (%)
Inborn, n (%)
Age at discharge, median (25–75th percentile)
Died
Home
Transfer
Transfer of service
581
(24–28)
(0.69–1.06)
(0.41 to 0.55)
(3–7)
(6–9)
(6.8)
(23.3)
(34.1)
(87.6)
NEC (NEC)
SIP vs NEC
X
X
X
Y
X
Y
X
Y
X
for SIP (as compared to the 14 days after birth for controls);
indomethacin exposure in the first 3 days of life and
hydrocortisone exposure in the first 3 days of life.
Using univariate analysis, the effect of combination therapy
(both indomethacin and any glucocorticoid) was evaluated
(Table 3B). When examining early exposure (days 0–3),
indomethacin in combination with glucocorticoids was found to be
significantly associated with SIP. This association was lost in the 2week window. In multivariate analysis, we were not able to
demonstrate an interaction between exposure to both indomethacin
and hydrocortisone and the occurrence of SIP. This may have been
due to the fact that concurrent use of indomethacin and steroids
was rare outside of the early window within the SIP cohort.
We also note that the effect of early post-natal dexamethasone
on neurodevelopment was widely publicized during the time period
these data were collected. In comparison to the previous study
using this data set, the use of early post-natal dexamethasone was
much lower during this epoch.9 This practice trend limited the
ability to test for an association between dexamethasone and SIP,
Insight into spontaneous intestinal perforation
J Attridge et al
97
Table 3 Perforations associated with (A) Timing of individual drugs and (B) drug combinations
Control (Cont)
Perforation (prior to Dx; SIP)
SIP vs Cont
581
633
Pp0.05
Antenatal drug exposure
Antenatal steroids reported, n (%)
373 (65)
368 (58.1)
Y
Early (1/2 the median time to diagnosis) drug exposure: days of life 0–3
Any report of indomethacin, n (%)
Any report of hydrocortisone, n (%)
Any report of dexamethasone, n (%)
158 (27.2)
36 (6.2)
13 (2.2)
273 (43.1)
78 (12.3)
23 (3.6)
X
X
43 (7.4)
9 (1.6)
2 (0.0)
32 (5.1)
12 (1.9)
16 (2.5)
Days of life 0–14
222 (38.2)
61 (10.4)
42 (7.2)
14 days prior to SIPa
280 (44.2)
97 (15.3)
63 (10)
(A) Timing of individual drugs
Number of patients, n
Intermediate drug exposure: days of life 4–7
Any report of indomethacin, n (%)
Any report of hydrocortisone, n (%)
Any report of dexamethasone, n (%)
Any drug exposure (87.3% of SIP occurred in the first 15 days)
Any report of indomethacin, n (%)
Any report of hydrocortisone, n (%)
Any report of dexamethasone, n (%)
(B): Drug combinations
Early drug exposure: days of life 0–3
Indomethacin and steroids both, n (%)
Indomethacin alone, n (%)
Steroids alone, n (%)
Neither, n (%)
Any drug exposure
Indomethacin and steroids both, n (%)
Indomethacin alone, n (%)
Steroids alone, n (%)
Neither, n (%)
17
141
31
392
(2.9)
(24.3)
(5.3)
(67.5)
Day of life 0–14
59 (10.2)
163 (28.1)
34 (5.9)
325 (55.9)
58
215
42
318
X
X
(9.2)
(34)
(6.6)
(50.2)
X
X
Y
14 days prior to SIPa
93 (14.7)
187 (29.5)
57 (9)
296 (46.8)
Y
X ¼ Pp0.05 where the trend is greater in the SIP cohort; Y ¼ Pp0.05 where the trend is less in the SIP cohort.
a
The window of 14 days prior to SIP is based on the date of reported diagnoses and is limited to 14 days or the number of days of life prior to diagnosis if less than 14.
but also potentially prevented dexamethasone, which has been a
dominant risk factor in the literature, from being an over-riding
confounder of other variables.
Discussion
The study of SIP has been challenging. Much of what we know
about risk factors for SIP has been derived either from retrospective
single-center studies or prospective randomized trials that were
stopped because SIP was an undesirable outcome. In addition, the
potential for diagnostic confusion between SIP and NEC has
delayed the application of national databases towards studying this
disease. We sought to advance the understanding of SIP by creating
a large, nationally derived database using the Pediatrix electronic
administrative note system.
Our first objective was to test for differences in demographics,
presentation and mortality between SIP and surgical NEC cohorts.
We found that infants with surgical NEC were of older gestation,
larger, less likely to be Caucasian and presented with their
diagnoses at significantly later days of life than infants with SIP.
Conversely, infants with SIP were more likely to have a PDA and to
receive treatment for it, more likely to receive surfactant and more
likely to require pressors. All of these are expected complications of
the more premature infant. Both NEC and SIP patients suffered
significantly greater mortality than the control cohort, but surgical
NEC patients had significantly greater mortality when compared to
SIP patients. When taken together, these findings paint two very
Journal of Perinatology
Insight into spontaneous intestinal perforation
J Attridge et al
98
distinct clinical pictures and confirm the hypothesis that NEC and
SIP are different diseases. This is despite the fact that they both
occur with similar prevalence in low birth weight infants.
Our second objective was to utilize our refined SIP data set to
examine drug associations with SIP. The available literature
suggests that prophylactic indomethacin exposure is not associated
with SIP as an independent variable (reviewed in Figure 1).6
However, when combined with early post-natal glucocorticoid
exposure, the available literature paradoxically suggests that
indomethacin exposure in the first days of life is associated with
SIP.7,8
SIP patients were more likely to have received indomethacin
during days 0–3 of life, but there was no such association in the
subsequent window from days of life 4–7. Within the 14-day
window, indomethacin was found to be significantly associated
with SIP; however, this association is difficult to evaluate since
87.3% of the 14-day indomethacin was administered during the
early window. Multivariate analysis confirmed that indomethacin
was an independent variable when administered within the 0- to 3day window.
Hydrocortisone was also found to be associated with SIP during
days 0–3 by both univariate and multivariate analysis, as was the
presence of a PDA, and the need for pressors within 14 days prior to
perforation. Conversely, antenatal steroid use was less prevalent in
the group of infants with SIP. We also found an association
between outborn birth status and SIP. This is the second
multicenter study to demonstrate these associations (outborn status
and less likely to have received antenatal steroids).8,15 The neonatal
transport environment remains one of the most physiologically
stressful situations for ELBW infants. Taken together, these
variables suggest a role that endogenous adrenocorticoid stress may
be as important as exogenous administration of glucocorticoids.
While many of these variables could be postulated to be cotraveling with increased severity of illness and associated with
intestinal hypoperfusion, being outborn seems an unlikely
associate. Since cortisol levels were not available in this data set, we
cannot rule out the possibility that our observed association
between indomethacin and SIP is dependent upon elevated
endogenous cortisol levels.
Indomethacin was also associated with SIP when combined with
steroids in the 0- to 3-day window by univariate analysis. The
persistent co-traveling of indomethacin, with markers of
glucocorticoid exposure or their effect, provides a potential
explanation for the uncommon frequency of SIP despite the high
rate of indomethacin exposure. In essence, a two-hit phenomenon
may be required for the genesis of SIP, thereby explaining why all
ELBW infants who receive indomethacin do not perforate.
There are limitations to this data set. First, this database is
retrospective and cannot be used to directly test causality. Second,
this data set is one of reported variables and not of actual
laboratory and pharmacy values. The inability to capture antenatal
Journal of Perinatology
indomethacin exposure is one such manifestation of this
limitation.
The strength of this study is that it represents a large cohort of
SIP cases (greater than all of those currently published added
together), and thus is well powered for investigation of multiple
variables. In addition, this is the first national data set to
demonstrate a cohort of SIP patients distinct from surgical NEC
patients (including those with NEC and perforation).
In summary, SIP is a distinct clinical disease entity from that of
surgical NEC and was diagnosed almost as frequently in preterm
infants during the last 3 years in our data set (see Electronic
Supplement A). We found that SIP patients were more likely to be
exposed to early post-natal indomethacin and had multiple
associations that clustered around stress-related and cortisolinfluencing variables. Our findings are consistent with a harmful
synergism hypothesis involving both early post-natal indomethacin
and glucocorticoids in the etiology of SIP.
Acknowledgments
Dr Gordon was supported by NIH NIDDK Grant 1KO8DK/HD61553-01. We are
grateful to Sheryl Mroz and Sarabeth Gordon, MS for their editorial support and to
all the caregivers within Pediatrix for their daily attentiveness to the electronic
note system.
References
1 Alpan G, Eyal F, Vinograd I, Udassin R, Amir G, Mogle P et al. Localized
intestinal perforations after enteral administration of indomethacin in
premature infants. J Pediatr 1985; 106: 277–281.
2 Aschner JL, Deluga KS, Metlay LA, Emmens RW, Hendricks-Munoz KD.
Spontaneous focal gastrointestinal perforation in very low birth weight
infants. J Pediatr 1988; 113: 364–367.
3 Scholz TD, McGuinness GA. Localized intestinal perforation following
intravenous indomethacin for patent ductus arteriosus. J Pediatr
Gastroenterol Nutr 1988; 7: 773–775.
4 Meyer CL, Payne NR, Roback SA. Spontaneous, isolated intestinal
perforations in neonates with birth weight less than 1000 g not associated
with necrotizing enterocolitis. J Pediatr Surg 1991; 26: 714–717.
5 Nagaraj HS, Sandhu AS, Cook LN, Buchino JJ, Groff DB. Gastrointestinal
perforation following indomethacin therapy in very low birth weight infants.
J Pediatr Surg 1981; 16: 1003–1007.
6 Schmidt B, Davis P, Moddemann D, Ohlsson A, Roberts RS, Saigal S et al.
Long-term effects of indomethacin prophylaxis in extremely-low-birthweight infants. N Engl J Med 2001; 344: 1966–1972.
7 Stark AR, Carlo WA, Tyson JE, Papile LA, Wright LL, Shankaran S et al.
Adverse effects of early dexamethasone in extremely-low-birth-weight
infants. National institute of child health and human development neonatal
research network. N Engl J Med 2001; 344: 95–101.
8 Watterberg KL, Gerdes JS, Cole CH, Aucott SW, Thilo EH, Mammel MC et al.
Prophylaxis of early adrenal insufficiency to prevent bronchopulmonary
dysplasia: a multicenter trial. Pediatrics 2004; 114: 1649–1657.
Insight into spontaneous intestinal perforation
J Attridge et al
99
9 Guthrie SO, Gordon PV, Thomas V, Thorp JA, Peabody J, Clark RH.
Necrotizing enterocolitis among neonates in the United States. J Perinatol
2003; 23: 278–285.
10 Fujii AM, Brown E, Mirochnick M, O’Brien S, Kaufman G. Neonatal
necrotizing enterocolitis with intestinal perforation in extremely premature
infants receiving early indomethacin treatment for patent ductus arteriosus.
J Perinatol 2002; 22: 535–540.
11 Garland JS, Alex CP, Pauly TH, Whitehead VL, Brand J, Winston JF et al. A
three-day course of dexamethasone therapy to prevent chronic lung disease
in ventilated neonates: a randomized trial. Pediatrics 1999; 104: 91–99.
12 Vermont Oxford Network Steroid Study Group. Early postnatal dexamethasone therapy for the prevention of chronic lung disease. Pediatrics 2001;
108: 741–748.
13
14
15
Gordon P, Rutledge J, Sawin R, Thomas S, Woodrum D. Early
postnatal dexamethasone increases the risk of focal small bowel
perforation in extremely low birth weight infants. J Perinatol 1999; 19:
573–577.
Gordon PV, Young ML, Marshall DD. Focal small bowel perforation: an
adverse effect of early postnatal dexamethasone therapy in extremely low
birth weight infants. J Perinatol 2001; 21: 156–160.
Watterberg KL. Weighing statistical certainty against ethical, clinical, and
biologic expediency: the contributions of the Watterberg trial tip the scales in
the right direction: in reply. Pediatrics 2005; 115: 1447.
Supplementary information is available on the Journal of Perinatology website (http://www.nature.com/jp)
Journal of Perinatology