Renal Potassium Handling in Healthy and Sick
Newborns
Hao Zhou* and Lisa M. Satlin†
Growing infants must maintain a state of positive Kⴙ balance, a task accomplished, in large part, by
the kidney. The distal nephron is uniquely adapted to retain total body Kⴙ early in life. The
magnitude and direction of net Kⴙ transport in the cortical collecting duct (CCD), the segment
responsible for the final renal regulation of Kⴙ balance in the adult, reflect the balance of opposing
fluxes of Kⴙ secretion and Kⴙ absorption. Evidence now indicates that the low capacity of the
neonatal CCD for Kⴙ secretion is due, at least in part, to a relative paucity of conducting Kⴙ channels
in the urinary membrane. A relative excess of Kⴙ absorption in this nephron segment may further
reduce net urinary Kⴙ secretion. Under conditions prevailing in vivo, the balance of fluxes in the CCD
likely contributes to the relative Kⴙ retention characteristic of the neonatal kidney.
© 2004 Elsevier Inc. All rights reserved.
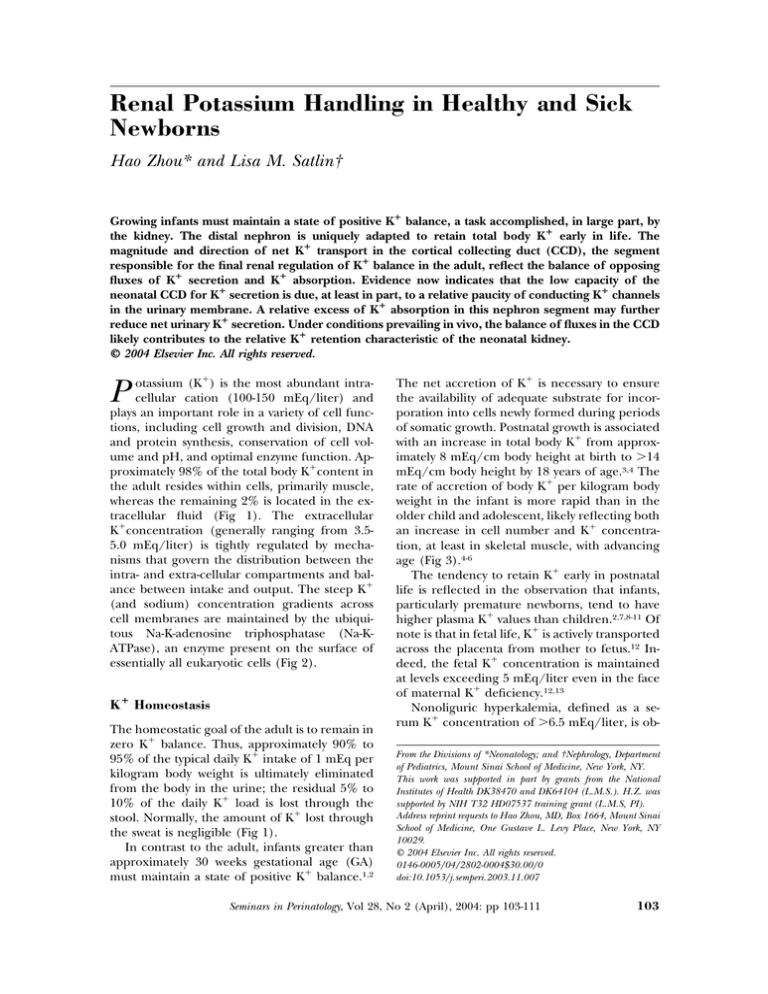
otassium (K⫹) is the most abundant intracellular cation (100-150 mEq/liter) and
plays an important role in a variety of cell functions, including cell growth and division, DNA
and protein synthesis, conservation of cell volume and pH, and optimal enzyme function. Approximately 98% of the total body K⫹content in
the adult resides within cells, primarily muscle,
whereas the remaining 2% is located in the extracellular fluid (Fig 1). The extracellular
K⫹concentration (generally ranging from 3.55.0 mEq/liter) is tightly regulated by mechanisms that govern the distribution between the
intra- and extra-cellular compartments and balance between intake and output. The steep K⫹
(and sodium) concentration gradients across
cell membranes are maintained by the ubiquitous Na-K-adenosine triphosphatase (Na-KATPase), an enzyme present on the surface of
essentially all eukaryotic cells (Fig 2).
P
Kⴙ Homeostasis
The homeostatic goal of the adult is to remain in
zero K⫹ balance. Thus, approximately 90% to
95% of the typical daily K⫹ intake of 1 mEq per
kilogram body weight is ultimately eliminated
from the body in the urine; the residual 5% to
10% of the daily K⫹ load is lost through the
stool. Normally, the amount of K⫹ lost through
the sweat is negligible (Fig 1).
In contrast to the adult, infants greater than
approximately 30 weeks gestational age (GA)
must maintain a state of positive K⫹ balance.1,2
The net accretion of K⫹ is necessary to ensure
the availability of adequate substrate for incorporation into cells newly formed during periods
of somatic growth. Postnatal growth is associated
with an increase in total body K⫹ from approximately 8 mEq/cm body height at birth to ⬎14
mEq/cm body height by 18 years of age.3,4 The
rate of accretion of body K⫹ per kilogram body
weight in the infant is more rapid than in the
older child and adolescent, likely reflecting both
an increase in cell number and K⫹ concentration, at least in skeletal muscle, with advancing
age (Fig 3).4-6
The tendency to retain K⫹ early in postnatal
life is reflected in the observation that infants,
particularly premature newborns, tend to have
higher plasma K⫹ values than children.2,7,8-11 Of
note is that in fetal life, K⫹ is actively transported
across the placenta from mother to fetus.12 Indeed, the fetal K⫹ concentration is maintained
at levels exceeding 5 mEq/liter even in the face
of maternal K⫹ deficiency.12,13
Nonoliguric hyperkalemia, defined as a serum K⫹ concentration of ⬎6.5 mEq/liter, is obFrom the Divisions of *Neonatology; and †Nephrology, Department
of Pediatrics, Mount Sinai School of Medicine, New York, NY.
This work was supported in part by grants from the National
Institutes of Health DK38470 and DK64104 (L.M.S.). H.Z. was
supported by NIH T32 HD07537 training grant (L.M.S, PI).
Address reprint requests to Hao Zhou, MD, Box 1664, Mount Sinai
School of Medicine, One Gustave L. Levy Place, New York, NY
10029.
© 2004 Elsevier Inc. All rights reserved.
0146-0005/04/2802-0004$30.00/0
doi:10.1053/j.semperi.2003.11.007
Seminars in Perinatology, Vol 28, No 2 (April), 2004: pp 103-111
103
104
Zhou and Satlin
Figure 1. Regulation of K⫹
balance in the adult. External
K⫹ balance is maintained by
the urinary (90%-95%) and
gut (5%-10%) excretion of
the daily K⫹ intake of ⬃1
mEq/kg/day in the typical
adult. Internal K⫹ balance depends on the distribution of
this cation between the extracellular fluid compartment (ECF) and the vast intracellular storage reservoirs
provided by muscle, liver,
erythrocytes and bone.
served in 30% to 50% of very low birth weight
(VLBW) infants, in the absence of K⫹ intake,
during the first 48 hours of life, but not in
mature infants or VLBW infants after 72 hours
of age.10,11 This biochemical observation reflects
a shift of K⫹ from the intra- to the extra-cellular
fluid space, possibly related to Na-K pump failure, as well as a limited renal K⫹ secretory capacity, as discussed below.10,11,14 Prenatal steroid
treatment may prevent nonoliguric hyperkalemia by upregulating Na-K-ATPase pump activity
in the fetus, thereby stabilizing the cell membrane to prevent a shift of K⫹ out of cells.15
Kⴙ Intake and Output
Figure 2. Generic cell model. The cellular uptake of
K⫹ and maintenance of a high cell K⫹ concentration
depend, in large part, on the activity of the ubiquitously expressed membrane-bound Na-K-ATPase
pump, which transports Na⫹ out and K⫹ into cells (in
a 3:2 ratio, respectively), at the expense of hydrolysis
of ATP.
In the adult, urinary K⫹ excretion varies considerably, depending in large part on dietary intake. Typically, adults that consume an average
American diet that contains more sodium (Na⫹)
than K⫹ excrete urine with a Na⫹-to-K⫹ ratio
greater than one.7 Although breast milk and
commercially available infant formulas generally
provide Na⫹ to K⫹ in a ratio of approximately
0.5 to 0.6, the urinary Na⫹ to K⫹ ratio in the
newborn typically exceeds one.7,9 Whereas a
high urinary Na⫹ to K⫹ ratio in the premature
infant may reflect the salt wasting characteristic
of newborns ⬍34 weeks GA,1,2,16,17 this finding
in the full-term newborn may be explained by a
greater requirement for K⫹ over Na⫹ during
growth and/or a relative hyporesponsiveness of
the neonatal kidney to mineralocorticoid activity.2,18
105
Renal Potassium Handling
Table 1. Factors, Relevant to the Infant, that
Acutely Regulate the Redistribution of K⫹ Between
the Intra- and Extra-cellular Space
Effect on cell
uptake of K⫹
Figure 3. Relationship between total body K⫹ (g)
and height (cm) for infants and children. The rate of
accretion of body K⫹ in the neonate is more rapid
than in later childhood, likely reflecting both an increase in cell number and K⫹ concentration, at least
in skeletal muscle, with advancing age.3,4
Regulation of Kⴙ Balance by
Redistribution
The daily dietary intake of K⫹ in the adult generally approaches or exceeds the total K⫹ normally present within the extracellular fluid space
(Fig 1). Although K⫹ balance in the adult ultimately depends on the timely renal elimination
of dietary intake, the renal excretion of K⫹ is
relatively sluggish, requiring from 6 to 12 hours
to be accomplished. Life-threatening hyperkalemia is not generally observed during this interval
due to the rapid (within minutes) hormonallymediated translocation of extracellular K⫹ into
cells, a response mediated by the Na-K-ATPase
(Fig 2). The hormonal, as well as other chemical
and physical factors that acutely influence K⫹
redistribution, are listed in Table 1.
Physiologic
plasma K concentration
1
2
insulin
catecholamines
␣-agonists
-agonists
Pathologic
acid-base balance
acidosis
alkalosis
hyperosmolality
cell breakdown
1
2
1
2
1
2
1
1 cell efflux
1 cell efflux
In newborns, the renal K⫹ clearance is low, even
when corrected for their low glomerular filtration rate.1,7 In response to exogenous K⫹ loading, infants like adults, can excrete K⫹ at a rate
that exceeds its filtration,20 indicating the capacity for net tubular secretion. However, the rate
of K⫹ excretion expressed either per unit body
weight or kidney weight in infants and young
animals subject to exogenous K⫹ loading is less
than that observed in older animals.20
In a longitudinal prospective study of 23- to
31-week GA infants, the fractional excretion of
K⫹ fell by half between 26 and 30 weeks GA, a
developmental change that was not accompanied by a significant change in absolute urinary
Regulation Of Kⴙ Balance Through Renal
Excretion
The processes involved in renal K⫹ handling
include filtration, reabsorption, and secretion
(Fig 4).7,19 Filtered K⫹ is reabsorbed almost entirely in proximal segments of the nephron; urinary K⫹ excretion, at least in the adult, is accomplished by K⫹ secretion in the distal segments of
the nephron.
It is now well established that the neonatal
kidney contributes to K⫹ retention early in life.
Figure 4. Sites of K⫹ transport along successive tubular segments of the fully differentiated nephron. Arrows identify the direction of net K⫹ transport as
either out of (reabsorption) or into (secretion) the
urinary fluid. See text for details. (Reprinted with
permission.56).
106
Zhou and Satlin
K⫹ excretion.1 Given that the filtered load of K⫹
increased almost 3-fold during this same time
interval, the constancy of renal K⫹ excretion
could best be explained by a developmental increase in the capacity of the kidney for K⫹ reabsorption.1
In general, the limited K⫹ excretory capacity
of the immature kidney becomes clinically relevant only under conditions of K⫹excess. As
stated earlier, under normal circumstances,
K⫹retention by the newborn kidney is appropriate and is required for multiple cellular processes including somatic growth.
Sites of Kⴙ Transport Along the Nephron
K⫹ is freely filtered at the glomerulus (Fig 4).
Studies in both suckling and adult animals indicate that approximately 65% of the filtered load
of K⫹ is reabsorbed along the proximal tubule
(Fig 4).19,21,22 Reabsorption is passive in this segment, closely following water reabsorption. Only
⬃10% of the filtered load of K⫹ reaches the
early distal tubule of the adult, indicating that a
significant amount of K⫹ has been reabsorbed in
the intervening segments, specifically across the
thick ascending limb of the loop of Henle
(TALH; Fig 4).19 In contrast, up to 35% of the
filtered load of K⫹ reaches the distal tubule of
the newborn rat.21 This suggests that postnatal
maturation of the TALH is characterized by a
developmental increase in its capacity for K⫹
reabsorption. The additional observations that
both the diluting capacity and TALH Na-K-
ATPase activity also increase after birth are consistent with this notion.23,24
K⫹ reabsorption in the TALH is mediated by
a Na-K-2Cl cotransporter that translocates one
K⫹ ion into the cell accompanied by one
Na⫹and two chloride ions (Fig 5A). Transporter
activity is ultimately driven by the basolateral
Na-K-ATPase, which generates and maintains a
low intracellular Na⫹ concentration and thus a
chemical gradient favoring Na⫹ entry at the apical membrane. Activity of the Na-K-2Cl transporter requires the presence of a K⫹ conductance in the apical (urinary) membrane to
recycle K⫹ across this membrane, thus ensuring
an abundant supply of substrate for the cotransporter. Diuretics such as furosemide and bumetanide that inhibit the Na-K-2Cl cotransporter
block K⫹ (as well as Na⫹) reabsorption at this
site and uncover K⫹ secretion, leading to profound urinary K⫹ losses.
The K⫹ channel present in the urinary membrane of the TALH (and cortical collecting duct;
see below) is believed to be encoded by the
ROMK gene.19,25,26 Loss-of-function mutations
in ROMK lead to antenatal Bartter syndrome,
also known as the hyperprostaglandin E syndrome, which is characterized by severe renal
salt and fluid wasting, consistent with a pattern
of impaired TALH function.27 The typical presentation includes polyhydramnios, premature
delivery, and life-threatening episodes of dehydration during the first week of life. This group
of patients also has severe growth failure, hypercalciuria, and early-onset nephrocalcinosis.
Figure 5. K⫹ (and Na⫹) transport pathways in the fully differentiated nephron. The major transport proteins
involved in K⫹ and Na⫹ transport are shown for the (A) thick ascending limb of Henle (TALH) and cortical
collecting duct, a nephron segment comprised of (B) principal and (C) intercalated cells. See text for details
regarding the transport pathways shown. (Reprinted with permission.56).
Renal Potassium Handling
Under baseline conditions in the adult, regulated K⫹ secretion by the distal tubule and the
cortical collecting duct (CCD) (Fig 4) contributes prominently to urinary K⫹ excretion, which
can approach 20% of the filtered load.19 In contrast to the high rate of K⫹ secretion observed in
CCDs isolated from adult rabbits and studied
when perfused at physiological flow rates in
vitro, segments isolated from neonatal animals
show no significant net K⫹ transport until after
the third week of postnatal life.28 By 6 weeks of
age, the rate of net K⫹ secretion in the CCD is
comparable to that observed in the adult.28
These results indicate that the low rates of K⫹
excretion characteristic of the newborn kidney
are due, at least in part, to a low K⫹ secretory
capacity of the CCD.
The CCD is comprised of 2 cell populations.
Principal cells (Fig 5B) reabsorb Na⫹ and secrete K⫹, whereas intercalated cells (Fig 5C)
primarily function in acid-base homeostasis but
can reabsorb K⫹ in response to dietary K⫹ restriction or metabolic acidosis. Thus, the direction and magnitude of net K⫹ transport in this
segment represents the balance of K⫹ secretion
and absorption, opposing processes mediated by
principal and intercalated cells, respectively.
Kⴙ secretion. K⫹ secretion in the CCD is accomplished by a two-step process. First, K⫹ is actively
taken up into the principal cell at the basolateral
membrane in exchange for Na⫹, a process mediated by the Na-K-ATPase (Fig. 5B). The high
intracellular K⫹ concentration and lumen-negative voltage within the CCD, generated by apical
Na⫹ entry across epithelial Na⫹ channels
(ENaCs) and its electrogenic basolateral extrusion, create an electrochemical gradient that favors the passive diffusion of cell K⫹ into the
luminal fluid through apical K⫹-selective channels. The small conductance secretory K⫹ (SK)
channel, encoded by the ROMK gene, is considered to mediate baseline K⫹ secretion in this
nephron segment.19,25,26 In sum, K⫹ secretion in
the CCD requires Na⫹ absorption (to establish
the electrochemical gradient) and the presence
of K⫹-selective channels in the urinary membrane. Any factor that enhances the electrochemical driving force or increases the apical
membrane permeability to K⫹ will favor K⫹ secretion.
The limited capacity of the neonatal CCD for
baseline net K⫹ secretion appears not to be due
107
to an unfavorable electrochemical gradient. Although Na-K-ATPase activity in the neonatal collecting duct is only ⬃50% of that measured in
the mature nephron,24,29 intracellular K⫹ concentration in this secretory epithelium at birth is
comparable to that measured in the adult (presumably reflecting a relative paucity of membrane K⫹ channels early in life).30 The rate of
net Na⫹ absorption in the CCD at 2 weeks of age
is ⬃60% of that measured in the adult and is not
considered to be limiting for K⫹ secretion.28
Cumulative evidence now suggests that the postnatal increase in CCD K⫹ secretory capacity is
due to a developmental increase in number of
SK channels, reflecting an increase in transcription and translation of functional ROMK channel proteins.31,32 Molecular analyses demonstrate that ROMK mRNA and protein are first
detectable in the second week of postnatal life in
the rodent, immediately preceding the appearance of functional channels and K⫹secretion in
this segment.32
Kⴙ absorption. The distal nephron of K⫹-depleted adults may reabsorb K⫹. This process is
mediated by a hydrogen, potassium adenosine
triphosphatase (H-K-ATPase), an enzyme,
present at the apical membrane of acid-base
transporting intercalated cells, that exchanges a
single K⫹ for a proton (Fig 5C). Fluorescent
functional assays identify significant activity of
the apical H-K-ATPase in neonatal intercalated
cells, suggesting that the collecting duct is
poised to retain urinary K⫹ early in life.33 As
stated earlier, clearance studies in premature
infants of ⬍30 weeks GA suggest a developmental increase in the capacity of the kidney for K⫹
reabsorption.1 Similar studies in saline-expanded dogs provide indirect evidence for a
diminished secretory and enhanced reabsorptive capacity of the immature distal nephron to
K⫹.34
Luminal and Peritubular Factors that
Regulate Net Kⴙ Transport in the CCD
Naⴙ delivery and absorption. As predicted from
the principal cell model (Fig 5B), the magnitude
of Na⫹ absorption determines the electrochemical driving force for K⫹ diffusion into the lumen. The dependence of K⫹ secretion on distal
Na⫹ delivery becomes evident at tubular fluid
Na⫹concentrations of less than 30 mEq/liter, a
108
Zhou and Satlin
value below which K⫹ secretion falls sharply.35,36
In vivo measurements of the Na⫹ concentration
in distal tubular fluid generally exceed 35
mmol/L both in adult and suckling rats and
thus would not be expected to restrict distal
K⫹secretion.37
Extracellular volume expansion or administration of many diuretics (osmotic diuretics, carbonic anhydrase inhibitors, loop and thiazide
diuretics) is accompanied by an increase in urinary excretion of both Na⫹ and K⫹. The kaliuresis is mediated not only by the increased
delivery of Na⫹to the distal nephron, but also by
the increased tubular fluid flow rate, which maximizes the chemical driving forces, as described
below, favoring K⫹ secretion. Other K⫹-sparing
diuretics, such as amiloride and triamterine,
block distal Na⫹ reabsorption, which reduces
the electrical potential gradient favoring K⫹ secretion.
Na⫹ delivered to the distal nephron is generally accompanied by chloride. Chloride reabsorption, which occurs predominantly via the
paracellular pathway, tends to reduce the lumen-negative potential that would otherwise
drive K⫹ secretion. When Na⫹ is accompanied
by an anion less reabsorbable than chloride,
such as bicarbonate (as in proximal renal tubular acidosis), -hydroxybutyrate (in diabetic ketoacidosis) or carbenicillin (during antibiotic
therapy), luminal electronegativity is maintained, thereby eliciting more K⫹ secretion than
occurs with a comparable Na⫹ load delivered
with chloride.
Tubular fluid (urinary) flow rate. K⫹ secretion in
the mature CCD is strongly stimulated by an
increase in urinary flow rate, as follows volume
expansion or administration of diuretics. However, the developmental appearance of flowstimulated K⫹ secretion, studied in single rabbit
CCDs, does not appear until the 5th week of
postnatal life, ⬃2 weeks after baseline K⫹ secretion is first detected (Fig 6).28,38 Recent evidence
suggests that flow-dependent K⫹ secretion is mediated by a stretch- and calcium-activated highconductance maxi-K channel.38,39 Maxi-K channel mRNA and protein are not consistently
detected in the CCD until the 4th week of life,38
suggesting that the postnatal appearance of flowdependent K⫹ secretion is determined by the
transcriptional and/or translational regulation
of expression of maxi-K channels in the distal
Figure 6. Relationship between postnatal age (in
weeks) and net K⫹ secretion (pmol/min.mm) in
CCDs isolated from rabbits and microperfused in vitro
at increasing luminal (urinary) flow rates. The presumed range of physiologic flow rates is indicated by
the stippled area. All segments were perfused and
bathed in a solution simulating an ultrafiltrate of
adult rabbit plasma. No significant net K⫹ transport
was detected in segments isolated from 2-week-old
animals. By 4 weeks of age, the rate of baseline net K⫹
secretion in tubules perfused at physiological slow
flow rates was similar to that observed in adult (ⱖ6week-old) animals. Whereas an increase in tubular
fluid flow rate significantly stimulated net K⫹ secretion in CCDs isolated from adult animals, flow was
without effect in the first month of life. Means ⫾ SE.
nephron. It should also be noted that the higher
the urinary flow rate in the distal nephron, the
slower the rate of rise of tubular fluid K⫹ concentration as secreted K⫹ is rapidly diluted in
urine of low K⫹ concentration. Maintenance of a
relatively low tubular fluid K⫹ concentration
maximizes the K⫹ concentration gradient and
thus chemical driving force favoring net K⫹ secretion.
Kⴙ intake. The adult kidney responds to an
increase in K⫹ intake with an increase in urinary
K⫹ excretion within ⬃1 to 2 days.40 The adaptation to a high-K⫹ diet is associated with an increase in density of conducting apical SK channels in the CCD within 6 hours.41 Apical Na⫹
channel and basolateral Na-K pump activity also
increase under these same conditions, changes
expected to enhance the electrochemical gradient favoring K⫹ secretion.42 The increases in SK
channel activity and K⫹ secretion are not medi-
Renal Potassium Handling
ated by an increase in circulating levels of mineralocorticoids alone, but depend upon a high
plasma K⫹ concentration.40 High plasma K⫹ levels have been suggested to lead to release an as
yet unidentified kaliuretic hormone from the
central nervous system through a reflex involving receptors in the gut or portal vein.43
When K⫹ intake is chronically reduced, K⫹
secretion by principal cells falls, in the absence
of any change in density of apical SK channels in
the CCD,40 whereas K⫹ reabsorption by intercalated cells is stimulated.44 Stimulation of H-KATPase activity in intercalated cells results not
only in K⫹ retention, but also urinary acidification and metabolic alkalosis.
Acid-base balance. Disorders of acid-base homeostasis can alter tubular K⫹ secretion. Acute
metabolic acidosis reduces cell K⫹ concentration and leads to a reduction in urine pH, which
in turn inhibits apical SK/ROMK channel activity.45,46 The net effect is a fall in urinary K⫹
excretion.47 Chronic metabolic acidosis has variable effects on urinary K⫹excretion. In chronic
metabolic acidosis, K⫹ secretion is influenced by
modifications of the glomerular filtrate (eg,
chloride and bicarbonate concentration), tubular fluid flow rate, and circulating aldosterone
levels.
Both acute respiratory alkalosis and metabolic alkalosis result in increases in urine pH
and K⫹ excretion. The alkalosis-induced stimulation of K⫹ secretion reflects 2 direct effects on
principal cells: 1) stimulation of basolateral K⫹
uptake and 2) an increase in the permeability of
the apical membrane to K⫹ due to an increase in
duration of time the SK/ROMK channels remain open.19
Mineralocorticoids. The role of aldosterone in
stimulating K⫹ secretion in the fully differentiated CCD is well established.48,49 In the adult,
the mineralocorticoid-induced stimulation of renal K⫹ secretion is considered to be due primarily to an increase in the electrochemical driving
force favoring K⫹ exit across the apical membrane, generated by stimulation of apical Na⫹
entry and reabsorption.
Aldosterone action requires its initial binding
to the mineralocorticoid receptor, followed by
translocation of the hormone-receptor complex
to the nucleus where specific genes are stimulated to code for physiologically active proteins.
Cellular effects within the fully differentiated
109
CCD include increases in the density of active
ENaC Na⫹ channels, due to recruitment of intracellular channels to the apical membrane, de
novo synthesis of ENaC subunits and activation
of pre-existing channels.50,51 Aldosterone also
stimulates Na,K-ATPase activity through both recruitment of intracellular pumps and increased
total amounts of Na pump subunits.52 The net
effect of these actions is the stimulation of net
Na⫹ absorption, leading to an increase in lumen
negative transepithelial voltage, thereby facilitating net K⫹ secretion. The effects of aldosterone
on ENaC and, to some extent, the Na-K pump
appear to be indirect, mediated by aldosteroneinduced proteins.53
Plasma aldosterone concentrations in the premature infant and newborn are high compared
to those in the adult.2,54 The density of aldosterone binding sites, receptor affinity, and degree
of nuclear binding of hormone-receptor appear
to be similar in mature and immature rats.18 Yet,
clearance studies in fetal and newborn animals
demonstrate a relative insensitivity of the immature kidney to the hormone, presumably due to
a postreceptor phenomenon.2,18,55 Measurements of the transtubular potassium gradient
(urine K⫹ concentration divided by the urineto-plasma osmolality ratio), an index of the K⫹
secretory capacity of the distal nephron, have
been reported to be lower in 27 than 30-week
GA preterm infants followed over the first 5
weeks of postnatal life.9 The low transtubular
potassium gradient has been attributed to a state
of relative hypoaldosteronism,9 but may also reflect the absence of K⫹ secretory transport pathways (ie, channel proteins).
Summary
Infants greater than approximately 30 weeks GA
and young children must maintain a state of
Table 2. Luminal and Peritubular Factors that
Increase Net K⫹ Secretion in the Distal Nephron
Luminal:
Na⫹ delivery and absorption
Tubular fluid flow rate
Peritubular:
K⫹ intake
alkalosis
hormones (mineralocorticoids)
110
Zhou and Satlin
positive K⫹ balance for somatic growth. The kidney is the primarily organ responsible for regulation of external K⫹ balance. Kidneys of fullterm newborn humans and animals conserve
K⫹. The CCD within the distal nephron is
uniquely adapted to retain total body K⫹ early in
life. In contrast to the brisk net K⫹ secretion
detected in single CCDs isolated from adult animals, CCDs isolated from newborns show no net
K⫹ secretion during the few weeks of postnatal
life. The magnitude and direction of net K⫹
transport in the CCD reflect the balance of opposing fluxes of K⫹ secretion and K⫹ absorption, mediated by principal and intercalated
cells, respectively. Evidence now indicates that
the low capacity of the CCD for K⫹ secretion
early in life is due to a limited capacity of principal cells for K⫹ secretion, reflecting, at least in
part, a relative paucity of conducting K⫹ (SK/
ROMK and maxi-K) channels in the urinary
membrane. A relative excess of K⫹ absorption by
adjacent intercalated cells in this nephron segment may further reduce net urinary K⫹ secretion. Under conditions prevailing in vivo, the
balance of fluxes mediated by these 2 cell types
likely contributes to the relative K⫹ retention
characteristic of the neonatal kidney.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
References
1. Delgado MM, Rohatgi R, Khan S, et al: Sodium and
potassium clearances by the maturing kidney: Clinicalmolecular correlates. Pediatr Nephrol 18:759-767, 2003
2. Sulyok E, Nemeth M, Tenyi I, et al: Relationship between
maturity, electrolyte balance and the function of the
renin-angiotensin-aldosterone system in newborn infants. Biol Neonate 35:60-65, 1979
3. Butte NF, Hopkinson JM, Wong WW, et al: Body composition during the first 2 years of life: An updated
reference. Pediatr Res 47:578-585, 2000
4. Flynn MA, Woodruff C, Clark J, et al: Total body potassium in normal children. Pediatr Res 6:239-245, 1972
5. Dickerson JWT, Widdowson EM: Chemical changes in
skeletal muscle during development. Biochem J 74:247257, 1960
6. Rutledge MM, Clark J, Woodruff C, et al: A longitudinal
study of total body potassium in normal breastfed and
bottle-fed infants. Pediatr Res 10:114-117, 1976
7. Satlin LM: Regulation of potassium transport in the
maturing kidney. Semin Nephrol 19:155-165, 1999
8. Rodriguez-Soriano J, Vallo A, Castillo G, et al: Renal
handling of water and sodium in infancy and childhood:
A study using clearance methods during hypotonic saline diuresis. Kidney Int 20:700-704, 1981
9. Rodriguez-Soriano J, Ubetagoyena M, Vallo A: Transtubular potassium concentration gradient: A useful test to
21.
22.
23.
24.
25.
26.
27.
28.
estimate renal aldosterone bio-activity in infants and
children. Pediatr Nephrol 4:105-110, 1990
Lorenz JM, Kleinman LI, Markarian K: Potassium metabolism in extremely low birth weight infants in the first
week of life. J Pediatr 131:81-86, 1997
Sato K, Kondo T, Iwao H, et al: Internal potassium shift
in premature infants: Cause of nonoliguric hyperkalemia. J Pediatr 126:109-113, 1995
Serrano CV, Talbert LM, Welt LG: Potassium deficiency
in the pregnant dog. J Clin Invest 43:27, 1964
Dancis J, Springer D: Fetal homeostasis in maternal malnutrition: potassium and sodium deficiency in rats. Pediatr Res 4:345-351, 1970
Stefano JL, Norman ME, Morales MC, et al: Decreased
erythrocyte Na,K,-ATPase activity associated with cellular
potassium loss in extremely low birth weight infants with
nonoliguric hyperkalemia. J Pediatr 122:276-284, 1993
Omar SA, DeCristofaro JD, Agarwal BI, et al: Effect of
prenatal steroids on potassium balance in extremely low
birth weight neonates. Pediatr 106:561-567, 2000
Al-Dahhan J, Haycock GB, Chantler C, et al: Sodium
homeostasis in term and preterm neonates. I. Renal
aspects. Arch Dis Child 58:335-342, 1983
Al-Dahhan J, Haycock GB, Nichol B, et al: Sodium homeostasis in term and preterm neonates. III. Effect of
salt supplementation. Arch Dis Child 59:945-950, 1984
Stephenson G, Hammet M, Hadaway G, et al: Ontogeny
of renal mineralocorticoid receptors and urinary electrolyte responses in the rat. Am J Physiol 247:F665-671,
1984
Giebisch G: Renal potassium transport: mechanisms and
regulation. Am J Physiol 274:F817-833, 1998
Tuvdad F, McNamara H, Barnett H: Renal response of
premature infants to administration of bicarbonate and
potassium. Pediatrics 13:4-16, 1954
Lelievre-Pegorier M, Merlet-Benichou C, Roinel N, et al:
Developmental pattern of water and electrolyte transport in rat superficial nephrons. Am J Physiol 245:F1521, 1983
Solomon S: Absolute rates of sodium and potassium
reabsorption by proximal tubule of immature rats. Biol
Neonate 25:340-351, 1974
Zink H, Horster M: Maturation of diluting capacity in
loop of Henle of rat superficial nephrons. Am J Physiol
233:F519-524, 1977
Schmidt U, Horster M: Na-K-activated ATPase: Activity
maturation in rabbit nephron segments dissected in
vitro. Am J Physiol 233:F55-60, 1977
Palmer LG: Potassium secretion and the regulation of
distal nephron K channels. Am J Physiol 277:F821-825,
1999
Zhou H, Tate SS, Palmer LG: Primary structure and
functional properties of an epithelial K channel. Am J
Physiol 266:C809-824, 1994
International Collaborative Study Group for Bartter-like
Syndromes: Mutations in the gene encoding the inwardly-rectifying renal potassium channel, ROMK, cause
the antenatal variant of Bartter syndrome: Evidence for
genetic heterogeneity. Hum Mol Gen 6:17-26, 1997
Satlin LM: Postnatal maturation of potassium transport
in rabbit cortical collecting duct. Am J Physiol 266:F5765, 1994
Renal Potassium Handling
29. Constantinescu AR, Lane JC, Mak J, et al: Na-K-ATPasemediated basolateral rubidium uptake in the maturing
rabbit cortical collecting duct. Am J Physiol Renal
Physiol 279:F1161-1168, 2000
30. Satlin LM, Evan AP, Gattone VH, et al: Postnatal maturation of the rabbit cortical collecting duct. Pediatr
Nephrol 2:135-145, 1988
31. Satlin LM, Palmer LG: Apical K⫹ conductance in maturing rabbit principal cell. Am J Physiol 272:F397-404,
1997
32. Zolotnitskaya A, Satlin LM: Developmental expression of
ROMK in rat kidney. Am J Physiol 276:F825-836, 1999
33. Constantinescu A, Silver RB, Satlin LM: H-K-ATPase activity in PNA-binding intercalated cells of newborn rabbit cortical collecting duct. Am J Physiol 272:F167-177,
1997
34. Kleinman LI, Banks RO: Segmental nephron sodium
and potassium reabsorption in newborn and adult dogs
during saline expansion. Proc Soc Exp Biol Med 173:
231-237, 1983
35. Good DW, Wright FS: Luminal influences on potassium
secretion: Sodium concentration and fluid flow rate.
Am J Physiol 236:F192-205, 1979
36. Stokes JB: Potassium secretion by cortical collecting tubule: relation to sodium absorption, luminal sodium
concentration, and transepithelial voltage. Am J Physiol
241:F395-402, 1981
37. Aperia A, Elinder G: Distal tubular sodium reabsorption
in the developing rat kidney. Am J Physiol 240:F487-491,
1981
38. Woda CB, Miyawaki N, Ramalakshmi S, et al: Ontogeny
of flow-stimulated potassium secretion in rabbit cortical
collecting duct: Functional and molecular aspects. Am J
Physiol Renal Physiol 285:F629-639, 2003
39. Woda CB, Bragin A, Kleyman TR, et al: Flow-dependent
K⫹ secretion in the cortical collecting duct is mediated
by a maxi-K channel. Am J Physiol Renal Physiol 280:
F786-793, 2001
40. Rabinowitz L, Sarason RL, Yamauchi H, et al: Time
course of adaptation to altered K intake in rats and
sheep. Am J Physiol 247:F607-617, 1984
41. Palmer LG, Frindt G: Regulation of apical K channels in
rat cortical collecting tubule during changes in dietary K
intake. Am J Physiol 277:F805-812, 1999
42. Palmer LG, Antonian L, Frindt G: Regulation of apical K
and Na channels and Na/K pumps in rat cortical col-
43.
44.
45.
46.
47.
48.
49.
50.
51.
52.
53.
54.
55.
56.
111
lecting tubule by dietary K. J Gen Physiol 104:693-710,
1994
Rabinowitz L: Aldosterone and potassium homeostasis.
Kidney Int 49:1738-1742, 1996
Wingo CS, Cain BD: The renal H-K-ATPase: Physiological significance and role in potassium homeostasis.
Annu Rev Physiol 55:323-347, 1993
Boudry JF, Stoner LC, Burg MB: Effect of acid lumen pH
on potassium transport in renal cortical collecting tubules. Am J Physiol 230:239-244, 1976
Xu H, Yang Z, Cui N, et al: Molecular determinants for
the distinct pH sensitivity of Kir1.1 and Kir4.1 channels.
Am J Physiol Cell Physiol 279:C1464-1471, 2000
Stanton BA, Giebisch G: Effects of pH on potassium
transport by renal distal tubule. Am J Physiol 242:F544551, 1982
Schwartz GJ, Burg MB: Mineralocorticoid effects on cation transport by cortical collecting tubules in vitro. Am J
Physiol 235:F576-585, 1978
Bonvalet JP: Regulation of sodium transport by steroid
hormones. Kidney Int 65:S49-56, 1998
Pacha J, Frindt G, Antonian L, et al: Regulation of Na
channels of the rat cortical collecting tubule by aldosterone. J Gen Physiol 102:25-42, 1993
Masilamani S, Kim GH, Mitchell C, et al: Aldosteronemediated regulation of ENaC alpha, beta, and gamma
subunit proteins in rat kidney. J Clin Invest 104:R19-23,
1999
Ikeda U, Hyman R, Smith TW, et al: Aldosterone-mediated regulation of Na⫹, K⫹-ATPase gene expression in
adult and neonatal rat cardiocytes. J Biol Chem 266:
12058-12066, 1991
Stockand JD: New ideas about aldosterone signaling in
epithelia. Am J Physiol Renal Physiol 282:F559-576, 2002
Van Acker KJ, Scharpe SL, Deprettere AJ, et al: Reninangiotensin-aldosterone system in the healthy infant and
child. Kidney Int 16:196-203, 1979
Aperia A, Broberger O, Herin P, et al: Sodium excretion
in relation to sodium intake and aldosterone excretion
in newborn pre-term and full-term infants. Acta Paediatr
Scand 68:813-817, 1979
Benchimol C, Satlin LM: Potassium transport in the
fetus and neonate, in Polin RA, Fox WW, Abman SH
(eds): Fetal and Neonatal Physiology (ed 3). Philadelphia, PA, Elsevier Science, 2003