Factors affecting 0, transfer in sheep and rabbit
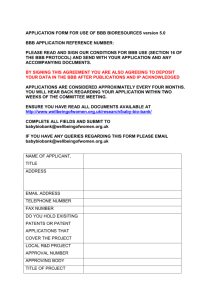
advertisement

AMERICAN JOURNAL OF PHYSIOLOGY Vol. 229, No. 4, October 1975. Prinied in U.S.A. Factors affecting 0, transfer in sheep and rabbit placenta perfused in situ GORDON Department G. POWER AND FITZGERALD JENKINS of Physiology, School of Medicine, Loma Linda University, Loma Linda, POWER,GORDON G., AND FITZGERALD JENKINS. Factors a$ecting US transfer in sheep and rabbit placenta perfused in situ. Am. J. Physiol. 229(4): 1147-1153. 1975-111 these experiments we have studied three factors that affect placental 02 transfer. The fetal artery of an isolated cotyledon of the sheep placenta (or one of the umbilical arteries in flow studies in rabbits) was perfused in situ with blood of varying Pop and at different flow rates while the ewe was administered varying inspired 02 concentrations. Measurements were made of the Paz of inflowing and outflowing umbilical blood, and the 02 transfer rate was calculated by the Fick principle. Changes in individual factors could be studied, since most compensations tending to maintain normal 02 delivery were not operative in the isolated preparation. Results indicate that a 20% change in umbilical arterial Paz, a 14q/‘, change in umbilical blood flow, and a 20 yO change in maternal arterial Paz would be equivalent in causing a 10% change in placental 02 transfer. Small changes in umbilical arterial Pea are sufficient to maintain the rate of placental 02 transfer equal to the rate of fetal consumption. Maternal arterial Paz becomes progressively more critical to fetal oxygenation as its level falls. The experimental results are compared to those predicted by a mathematical model of placental exchange. isolated cotyledon; umbilical and uterine blood flow and Peg SINCE THE PIONEERING WORK of Barcroft, Barron, and Huggett and their co-workers (1-3, 13), a variety of factors affecting placental exchange have been studied in sheep and other animals as well as man. Many investigators have obtained samples of blood flowing to and from the placenta under physiologic conditions and sought to describe placental transfer as it operates during normal fetal life (14, 21). These studies have contributed substantially to our understanding of the basic mechanisms of placental transfer. Oxygen transfer, for example, has been shown to depend on the inflowing oxygen tensions in uterine and umbilical arteries, maternal and fetal blood flow rates, and the placental diffusing capacity (17). The importance of these factors, furthermore, has been found to vary in different species and at different times during gestation (I). There are two major drawbacks using results of such studies in attempting to understand placental exchange quantitatively. In the first place, the importance of individual factors is difficult to assess because compensations in the intact animal tend to mask the effects of primary changes. For example, at high altitude not only will maternal arterial oxygen tension fall, but other factors, such as hemoglobin levels and blood flow rates, will change as well, thereby California 92354 partially masking the efYects of the primary change (4, 15). And second, there is the difficulty that venous blood samples-critical in the analysis of placental transfer-constitute collections of blood draining different areas of the entire placenta which do not necessarily accurately reflect the transfer taking place in any single exchange unit. Thus, admixture of shunted blood (22) as well as that blood draining from units with different relationships of maternal and fetal blood flows (25, 26) and diffusing capacity (23), and oxygen consumption (6), will distort the accuracy of venous values (18, 24). While changes of a given factor will affect the placental end-capillary values in a single unit, the change may not be accurately reflected by the venous values+ We have sought to minimize these problems in these experiments by isolating a cotyledon of the placenta and perfusing its umbilical circulation in situ with blood of known and accurately controlled flow rates and 02 tensions. We have also varied maternal arterial 02 tensions by administering various concentrations of inspired 02. Thus, the present data describe the consequences of varying three of the primary determinants of placental 02 transfer one at a time while avoiding the effects of compensatory changes in the system. Although the problem of uneven distribution could not be avoided entirely, it was reduced by studying a single cotyledon of the placenta. METHODS Cross-bred ewes were studied at 110-135 days gestation (term about 147 days) under spinal anesthesia (20 mg Pontocaine) and barbiturate sedation (6 mg/kg pentobarbital). A catheter was inserted into a carotid artery under local anesthesia (Xylocaine) to monitor maternal blood pressure and to collect samples for arterial oxygen tension measurements. A tracheostomy was performed and the ewe allowed to breathe air or other gas mixtures spontaneously from a Douglas bag. The abdomen was opened and one of the uterine horns through a midline incision, containing a number of cotyledons was exposed. (The sheep placenta consists of 60-120 discrete cotyledons implanted over the uterine caruncle&) The uterus was incised, and the uterine wall lying opposite the incision was invaginated into the wound so as to expose one of the cotyledons lying some distance from the incision. Membranes were gently stripped from the vessels. A plastic catheter (PE-90) was inserted into the artery, and a second catheter (PE-90 or PE-60) was placed in the vein supplying the single cotyledon. The preparation is illustrated schematically in Fig. 1. G. 1148 MATERNAL PRESSURE ART. PUMP 11 OUTFLOW UMBILICAL INFLOW AND OUTFLOW PRESSURE SENSORS 1. Schematic diagram of perfusion of isolated cotyledon. A syringe pump perfuses maternal blood at constant rate through an umbilical artery supplying a single cotyledon. Inflowing and outflowing samples of blood are taken for analysis of respiratory gas tensions, and pH and vascular pressures are monitored with transducers. Bulk of placenta is undisturbed and fetus remains in utero. G. POWER AND F. JENKINS lated as the product of fetal perfusion rate (known from the pump setting and calibration) and the arteriovenous 02 content difference. Hemoglobin dissociation curves corrected for pH and temperature were used to convert Paz to oxyhemoglobin saturation. An average curve for the two types of sheep hemoglobin was used (19), and the oxygen tension at half-saturation for rabbit hemoglobin was taken as 31.6 mmHg (pH 7.4,38”C). RESULTS AND DISCUSSION FIG. Heparinized maternal blood was used to perfuse the cotyledon after it had been equilibrated with various gas mixtures in swirl tonometers at 37 “C. Perfusion was begun at 1.6 ml/min from a calibrated syringe infusion pump (Harvard Instrument Co., Millis, Mass., model 972). This flow rate, roughly one-third of normal, was chosen as standard because it resulted in inflow blood pressures in the normal range of 60 mmHg, i.e., the resistance to blood flow was about 3 times greater than normal in the artificially perfused organ. Settling of red cells was prevented by rotating a magnetically driven stirring bar inside the perfusion syringe. Before entering the placenta, blood was passed through a cotton wool filter to remove small particulate matter. Collateral and small secondary vessels were tied off to isolate the circulation to the cotyledon. This was verified by I) temporarily stopping the perfusion to test whether the outflow of blood ceased completely and 2) demonstrating in separate control experiments that the rate of outflow was equal (+5 %) to the rate of pump perfusion. The isolated cotyledon was returned to within the uterine cavity and the abdominal incision closed. Rabbits were studied at 27-29 days of gestation (term 30 days) under barbiturate anesthesia (20 mg/kg pentobarbital). The fetus was delivered through an incision in the antimesenteric border of the uterus, and one of the two umbilical arteries was perfused in situ while effluent blood was collected from an umbilical vein. Other umbilical vessels were tied off. Blood was drawn from a second adult rabbit to provide adequate quantities for perfusion. In rabbits, blood was passed through a temperature-controlled water jacket at 38°C before entering the placenta, but in sheep warming of blood was not considered necessary, since the cotyledon lay within the maternal abdomen. Samples of blood flowing to and from the cotyledon were collected in glass capillary tubes of 0.18 ml volume, and maternal arterial samples were collected in heparinized glass syringes. Samples were placed in ice and later analyzed for Paz, Pcoz, and pH with a Radiometer blood gas analyzer (model BMS3). Control studies showed less than 1 mmHg Pop change per hour in the capillary tubes while awaiting analysis. The reason this change was small may be attributed to the low range of Paz under study. Corrections were applied where necessary. Hemoglobin content was determined as cyanmethemoglobin. The net 02 transfer rate across the placenta was calcu- Eff& of varying matmid arterial 0xygcn tension. Oxygen, air, a.nd vari .OUS Nz-air mixtures were administered in random sequence to six ewes for 3- to IO-min intervals. The inspired gases achieved maternal arterial 02 tensions ranging from 27 to 340 mmHg. During this interval, the isolated cotyledon was perfused at constant flow rate (1.6 ml/min) with blood of constant Paz (8-10 mmHg). At the end of the interval, maternal arterial, umbilical arterial, and umbilical venous blood samples were taken simultaneously and analyzed for respiratory gases and pH. Figure 2 shows the effect of varying maternal arterial PO* on oxygen transfer rate. Figure 3 shows the effect of 10 02 EXCHANGE RATE t 8ML/MIN l . . * L 100 MATERNAL ARTERIAL 300 I 200 Pa2 I (MM HGI on maternal arterial POZ. FIG. 2. Dependence of 02 exchange Thirty-eight determinations were obtained on 6 sheep, an average of 6 determinations from each. Curvilinear regression shown as solid line shown has form: was fit to data to minimize sum of squares. Curve ‘ciro2 = -22.5 + 9.38 (In Mat POZ) - 0.733 (In Mat Po~)~, which fit data significantly better than simple linear or quadratic forms. 750 OUTFLOW I2 pO2 (MM HG) -40 MAT. PO2 0.5 -loi l c 1 MATERNAL 100 * ARTERIAL 200 1 PO2 I 300 (MM HG) FIG. 3. Dependence of outflow Paz on maternal arterial POZ. Regression curve fit to data has form: outflow POT = - 75.2 + 36.9 (ln Mat Paz) - 3.04 (In Mat Po~)~, a form which fit data significantly better than linear or quadratic regressions. O2 TRANSFER IN PERFUSED 1149 PLACENTA maternal Po2 on outflowing (umbilical venous) POT.Results for all experiments are shown as data points. Curvilinear regressions were found to fit the data significantly better than linear regressions (27). The curves shown in the figures were fitted through the data to minimize the sum of squares, and the form of each curve is given in the legends. A comparison of the data curves with predictions of a theoretical model is given below. The average oxygen transfer rate for the single cotyledon rose roughly 40 % as maternal PO:! increased from 100 to 340 mmHg. Umbilical venous Pox rose about 25 % for this maternal change. These increases are not exceptionally large, probably due to the shape of the oxyhemoglobin saturation curve. Decrements in maternal PO;!below normal levels became progressively more detrimental to 0, transfer. At a maternal Po2 of 50 mmHg (73 % saturation), for example, umbilical venous POT was about 23 mmHg, and the 02 exchange rate had decreased to less than 0.03 ml/min, a 40-50 % reduction. These relatively large changes are probably greater than would be observed in the intact animal or human, since most compensatory mechanisms that maintain 02 transfer were not operative in the isolated cotyledon. Control experiments to examine whether these results could be attributed to progressive deterioration in the function of the cotyledon are described below. Effects of varying umbilical Jkw rate. Fetal vessels supplying the cotyledon were perfused at Aow rates ranging from 0.22 to 4.0 ml/min in sheep and from 0.05 to 2.3 ml/min in rabbits. About 10 different flow rates were studied randomly in each of 10 ewes and 5 rabbits. Figure 4 shows the effects of varying fetal flow on the 02 tensions of blood leaving the cotyledon in sheep; results for rabbits were similar. To consolidate the results of changes in flows in the various preparations-some of which were more efficient in gas exchange than others-we have normalized the data by plotting 02 tension measured relative to the 02 tension measured in that preparation at a standard flow. Regression curves are again shown. -2 OUTFLOW 1.5 ’ PO2 PO2 MEASURED Po2AT STANDARD FLOW : . l 05 FETAL I 1 COTYLEDONARY 2 I BLOOD FLOW ML/MIN 3 1 4 I FIG. 4. Dependence of outflow POT on fetal cotyledonary flow. An average of 10 determinations are shown for each of 10 sheep. Data are normalized so that different preparations may be compared. Outflow POT is expressed relative to outflow PO* found in that preparation when fetal flow was 1.6 ml/min. Curvilinear regression shown through data is of form: outflow Po2 (relative to standard) = 1.33 - 0.73 (Fet flow) + 0.18 (Fet Aow)~. 02 EXCHANGE RATE io2 MEASURED to2 AT STANDARD FLOW FETAL COTYLEDONARY FLOW ML/MIN 5. Dependence of 02 exchange on fetal cotyledonary flow. 02 exchange is expressed relative to standard for that preparation when flow was 1.6 ml/min, a time when 02 exchange averaged 0.05 ml 02/min. Regression curve is of form: v02 (relative to standard) = 0.074 + 2.55 (Fet flow) - 1.62 (Fet flo~)~. FIG. Figure 4 shows that outflowing Paz tended to increase at slower flow rates. This was an anticipated finding, since fetal end-capillary Paz should increase as the ratio of maternal to fetal flow increases (17). This follows since more 02 is supplied relative to the capacity of fetal blood to transport it away from the placenta, and therefore final equilibrium is attained at a higher Po2. In fact, ignoring placental 02 consumption, fetal outflowing PO:! should theoretically approach maternal arterial Paz at very slow fetal flow rates. This result was observed in two of the rabbits studied. In two sheep, results were anomalous; however, in that outflowing PO:! fell at low flow rates. This may have been because I) al .arger fraction of the total OxYge n delivered to the platen ta 1s metabolized by placental tissue at low flows, and 2) distribution becomes more uneven between fetal flow and surface area for exchange at low flows, with a consequent fall in the efficiency of O2 exchange. Thus, a larger fraction of fetal flow might pass through regions remote from the exchange areas. Blood remains for a relatively short interval of time in the exchanging vessels at high flow rates. If a diffusional limitation to 02 exchange were present, it should have become apparent once a certain flow rate had been exceeded by an abruptly decreasing Paz in fetal effluent blood (17), other things being equal. The present data gave no hint of such a change and hence do not support any diffusional limitation of 02 transfer. Figure 5 shows the effect of fetal flow on the 02 exchange rates. Again the data are normalized so the results from different preparations can be included together. Effects of varying umbilical arterial 02 tension. The cotyledon was perfused simultaneously with blood from two infusion pumps. The output from each of the pumps was mixed together before entering the placenta. One syringe contained blood with a low oxygen tension (PO, = 10 mmHg, Pco:! = 40 mmHg, pH = 7.4) and the other blood with a higher oxygen tension (PO, = 50 mmHg, Pcoz = 40 mmHg, pH = 7.4). By varying Aow rates of the two pumps independently, the PO, of the inflowing blood could be varied while total flow and Pcoz were held constant. G. G. POWER l . . 1.5 02 EXCHANGE RATE i0, MEASURED $AT STANDARD INFLOW PO2 INFLOW PO2 IOL 20I l 30 MM HG SO 40 I FIG. 6. Dependence of 02 exchange on inflow (umbilical arterial) Paz. An average of 14 determinations is shown from each of 5 sheep. 02 exchange is expressed relative to average 02 exchange for that preparation when inflow Paz is 15 mmHg. A linear regression fit data as well as other curves, with form: vo2 (relative to standard) = 1.25 0.0305 (inflow PO& OUTFLOW PO2 PO2 AND F. JENKINS rate. The same type of divergent response was noted with changes in umbilical flows. Indeed, the only change in fetal hemodynamics that would seem able to increase both outflowing Paz and 02 transfer rate simultaneously would be a more uniform distribution of fetal placental blood flow, such that it more closely parallels maternal flow distribution and/or the available surface for gas exchange. Control experiments. The sequence of studying d&rent flow rates and 02 tensions was random and varied from one preparation to another in an effort to minimize systematic errors. To further evaluate possible errors which might have been caused by progressive deterioration in the function of the cotyledon, we carried out a series of control experiments in another group of five sheep. The cotyledon was perfused at constant flow rate with the same blood for 1.5 h while the ewe breathed air. Inflowing and outflowing blood samples were collected about every 15 min. Results for one sheep are shown in Fig. 8 and, as can be seen, outflowing Paz and 02 exchange rate remained generally constant. As an average for all sheep, the PO:! of outflowing blood remained within 4 mmHg (k SD) of initial levels during the l-2 h of perfusion. Thus, it would seem that the 02 transfer function of the cotyledon was maintained within 20 % of initial levels during the time period of the study. After 2-3 h of perfusion, signs of extravasation and edema appeared in some of the cotyledons and inflow pressure increased. The experiment was ended when these changes were considered to have become significant. MEASURED PD2 AT STANDARD INFLOW PO2 FIG. 7, Dependence of outflow POT on inflow Paz. Outflow Paz is expressed relative to average outflow Pas for that preparation when inflow Pea is 15 mmHg. Best fit data curve is of form: outiow POS (relative to standard) = 0.85 + 0.0047 (inflow POZ) + 0.0004 (inflow PO,) .2 An average of 14 different 02 tensions were studied in random sequence in each of 5 sheep. The effects of varying umbilical Paz on transfer rate are shown in Fig. 6 and the effect on placental outflowing Paz is shown in Fig. 7, It may be seen that both 02 transfer rate and outflowing POZ are sensitive to small changes in umbilical arterial Po2, For example, a 20 % fall in umbilical arterial Po2 below normal (15 mmHg) resulted in a 13 % increase in 02 transfer rate. Since umbilical arterial PO:! varies a few millimeters Hg from day to day in unanesthetized sheep (7), the data suggest that these changes would be associated with sizeable variations in the transfer function of the placenta for oxygen. It is of interest that changes in umbilical arterial PO:! resulted in changes in both 02 transfer rate and outflowing POTwith the responses occurring in opposite directions- That is to say, decreases in umbilical arterial Pop increased umbilical venous Paz at the expense of lowering the 02 transfer COMMENT Rdatiw imfortance of factors aecting placental 02 transfer. This will depend upon how sensitive 02 transfer is to changes in various factors, their normal range of variation, and the time course of their change. The present experiments characterize the dependence of 02 transfer on maternal arterial Po2, fetal flow rate, and fetal inflowing Paz. Of these three, 02 transfer is found to be most sensitive to a given percent-50 MM HG -30 -10 -to 02 EXCHANGE RATE ML/MlN .,/‘-*-‘-.,- 0-m X IO2 5 c 01 L 20 MINUTES I 8. Control study showing that exchange rates do not vary appreciably FIG. sion. 4. L L inflow and outflow during initial 60 60 ! and 02 min of perfuPOT O2 TRANSFER IN PERFUSED 1151 PLACENTA age change in umbilical blood flow. For example, to accomplish a 10 % rise in 02 transfer, there would be required a 20 % change in umbilical artery PO*, a 20 % change in maternal arterial Paz and a 14 % change in umbilical flow (values estimated from the slopes of the data fit curves). Of the three factors umbilical arterial Paz is of particular interest because it is affected by the metabolic rate of the intact fetus. That is to say, inflowing Paz in the umbilical arteries is a consequence of oxygen extraction by the fetal tissues, on the one hand, and a major determinant of placental 02 transfer, on the other hand. The level of umbilical arterial Pop thereby directly links fetal needs and 02 delivery. The present data show that a change of only 3 mmHg in umbilical arterial Paz will cause a 10 % change in transfer rate. As noted above, moment-to-moment and day-to-day fluctuations in Pea of this magnitude are measured (7, 2 1). These fluctuations suggest the possibility that umbilical arterial Paz is continually seeking a level that causes placental 02 transfer to equal fetal 02 consumption, as, of course, it must in the long term. If this is so, adjustments in placental 02 transfer would require no more than the 5-10 s required for blood to recirculate between placenta and peripheral tissues. Such a homeostatic mechanism would not require energy expenditure by the fetus nor neural control reflexes. The data, therefore, permit the hypothesis that umbilical arterial Pas is a critical link in the passive regulation of placental 02 transfer. While other factors are of undoubtedly great importance over the long term, they are probably of lesser importance over the short term for a variety of reasons. An example is umbilical blood Aow. Elsner (personal communication) finds in radiotelemetry experiments in unanesthetized sheep that umbilical blood flow remains remarkably constant during rest as well as exhausting maternal exercise. This constancy speaks against a short-term regulatory role for umbilical blood flow. Other arguments supporting a constancy of flow have been discussed by Faber (11) A constant flow and hence constant pressure would tend to maintain water balance between mother and fetus, other things being equal. In brief, the fetus would avoid becoming dehydrated during periods of increased 02 transport. Over the long term, of course, the situation is altogether different. Here umbilical flow increases several orders of magnitude as the fetus grows and 02 transport increases in accord with fetal needs. Other factors affecting placental 02 transfer probably change too slowly to have an important regulatory function. For instance, changes in hemoglobin concentration and the oxygen affinity of fetal blood would require several hours or days to affect 02 delivery appreciably. Nor is there any presently known mechanism for maternal placental flow or other maternal adaptations to respond to the level of fetal oxygenation. If oxygen requirements of the fetus do vary over the short term while umbilical flow is reasonably constant, then fetal tissues must withstand intervals of time when they receive blood with less than average 02 content. One might suspect adaptations to maintain 02 utilization in vital organs, including a redistribution of blood flow throughout the body and changes in the number of functioning capillaries per unit of tissue. In contrast to adult tissues, these adaptations have not been extensively studied in the fetus. Comparison with computer model predictions. We used a marhematicaf model to compare experimental results with those predicted theoretically. The model assumes difftision of 02 between parallel capillaries with uniform diameter, equal length, and uniform concurrent maternal and fetal flow as described previously ( 12). We varied each factor one at a time in the model while keeping others constant to assess its effects without compensatory changes occurring in the rest of the system In constructing the predicted model curves, we used averages for the experimental values for maternal and fetal hemoglobin concentrations (10.7 and 10.8 g/100 ml, respectively), maternal inflowing Paz (90 mmHg), fetal inflowing POT (12 mmHg) and fetal flow rate (1.6 ml/min), placental diffusing capacity (0.04 ml/min X mmHg) and placental tissue 02 consumption (6 ml/min X kg). These values were assumed ‘to remain constant during an experiment. Because maternal flow to the isolated cotyledon was unknown, we predicted a family of curves covering a range of maternal flows from 0.5 to 3 ml/min, some lo-50 % of estimated normal. It was in this low range that data and predicted results tended to agree, a not unreasonable finding since uterine surgery is known to lower maternal blood flow to the uterus. Since the computer predictions were for different, arbitrary (and low) maternal flows’, any agreement between experimental and theoretical results is not meaningful in absolute terms. The predicted trends as contrasted to experimental data remain valid points of comparlson. In Fig. 9 the curves fit to the experimental data are plotted again as solid lines, and they may be compared to the results predicted by the theoretical model shown as interrupted lines. In Fig. 9, A, B, and D the model predictions may be seen to follow the data satisfactorily. In these instances, in fact, the model predictions fit the data as well as the regression curves within statistical limits (27) if maternal flows were such as to give the best model fit. In other instances, however, the model proved somewhat inadequate quantitatively. For example, as shown in Fig. 9 E, the model predicted that outflowing Paz should rise more \L --. 1 : I?0 MATERNAL - CURVE 2op 1 I,6 3.; FET. COTYLEDON FLOW **.**.-. FIT TO DATA MODEL PD2 r c 1 115 FET. INFLOW 3: PO2 PREDfCTlON 9; Comparison of data-fit curve,s with predictions of a mathematical model of placental oxygen exchange. Slopes of interrupted and continuous lines should be compared as a test of agreement between experimental data and model; comparison in absolute terms is not possible because arbitrary (and low) maternal flows were assumed in making model predictions. FIG. 1152 G. sharply at low flow rates and fall more sharply at high flow rates than it actually did. There was a small but significant reduction (P < 0.05) in the sum of squares between the best data fit curve and the best model prediction curve (assuming maternal flow of 1.3 ml/min). There was also a small but significant difference between model and experimental data in Fig. 9, C and F. Because of these differences there are likely to be errors of inadequacies in the assumptions of the model. These might include the facts that the model takes no account of I) changes in the distribution pattern of flows at different flow rates, 2) differences in 02 con sumption by p lacental t issue at vario us oxygen tensions, and 3) changes in maternal flow as fetal flow varies. Additional studies will be needed before the model can be improved in these regards. Figure 9 shows that differences between predicted and experimental results were generally small. By and large , the present data were found compatible with a model assuming a concurrent pattern of flow in exchan ge vessels with little or limitation. The data were no t sufficiently n .o diffusional closely grouped, however, that it was possible to exclude crosscurrent, countercurrent, and other flow patterns combined with diffusional limitations. Thus, other models may fit the data equally well, and many previous theoretical analyses have been presented (5, 9, 10, 16, 20) whose results may be compared with the experimental data given here. Advmtuges and disadvantages of isolated, perfused cotyledon. Advantages include 1) the blood used for perfusion contains a constant and readily measured concentration of respiratory gases, electrolytes, hormones, and vasopressors. Thus, the preparation is free from systemic changes caused by release of catecholamines, falling pH, and low glucose levels that are known to follow fetal surgery. 2) Umbilical flow rate is constant, since it comes from an infusion pump. Changes in vascular pressure, therefore, are a reliable index of changes in resistance to placental blood flow, an important advantage in analyzing pressure-flow relationships. 3) The fetal lamb remains in utero and within the maternal abdomen, reducing traction on the uterine vessels and thereby minimizing the changes in maternal blood flow due to G. POWER AND F. JENKINS surgery. This is an advantage over isolated perfused preparations reported previously (8). All umbilical flow is directed to an “end-capillary” vascular bed and collateral flow, such as that supplying surrounding membranes, is eliminated. There are several disadvantages and these include: 1) there is no method known to measure maternal flow to the isolated cotyledon. We attempted to insert catheters in these tiny maternal vessels but were unsuccessful. Rather it is necessary to assume that maternal flow remains constant throughout an experiment, an assumption justified by the finding of nearly constan t res pira tory gas tensions in outflowing fetal blood during long con trol periods. 2) Umbilical vessels constrict where catheters are placed in them, and there is a high resistance to blood flow. High flow resistance may also have been caused by poorly understood changes in the microvasculature as reported in other artificially perfused organs. In fact, we had to limit fetal flows to about 30 % of normal in order to keep vascular pressures in a normal range. 3) When maternal blood is used to perfuse the umbilical circulation, allowance is required for its lesser oxygen affinity. With due caution regarding these disadvantages, the preparation should prove helpful in studying transplacental movements not only of oxygen but also a variety of other organic and inorganic substances, the possible hormonal controls involved, and the changes during gestation. The authors express their appreciation to John Bankhead and Peter Yuen for expert technical assistance. This study was supported by the Lalor Foundation, United Cerebral Palsy Foundation, and the National Institute of Child Health and Human Development Grant HD 04394. Computational aid was given by the Scientific Computation Center, School of Medicine, Loma Linda University, which is partially supported by National Institutes of Health Grant FR-00276. This study was presented in part at the Meeting of the Federation of American Societies for Experimental Biology at Chicago, Ill., in April, 1971, G. G. Power is the recipient of Public Health Service Research Career Development Award J-K4 H.D. 02,253. Received for publication 13 May 1974. REFERENCES J., J, A. KENNEDY, AND M. F. MASON. Oxygen in the blood of the umbilical vessels of the sheep. J. Physiol., London 97: 347-356, 1940. 2. BARRON, D. H. Some aspects of the transfer of oxygen across the syndesmochorial placenta of the sheep. Yale J. 113ioZ. Med. 24: 169490, 1951-1952. Supplementary observations 3. BARRON, D. H., AND G. ALEXANDER. on the oxygen pressure gradient between the maternal and fetal bloods of sheep. Yale J. Biol, Med. 25 : 61-66, 1952. 4, BARRON, D. H., J, METCALFE, G. MESCHIA, W. HUCKABEE, A. HELLEGERS, AND EL PRYSTOWSKY. Adaptations of pregnant ewes and their fetuses to high altitude. Symp* Bysiol. Effects High Altitude, 1. BARCROFT, Interkaken, Switzerland, 1963. 5. BARTELS, H., AND W. MOLL. Passage of inert substances and oxygen in the human placenta. P’uegers Arch. 280: 165-l 77, 1964. 6. CAMPBELL, A. G. M., G. S. DAWES, A. P. FISHMAN, A. I. HYMAN, AND G, B. JAMES. The oxygen consumption of the placenta and foetal membranes in the sheep. J. Physiol.,’ London 182: 439-464, 1966. 7. COMLINE, R. S., AND M. SILVER. Daily changes in foetal and maternal blood of conscious pregnant ewes, with catheters in umbilical and uterine vessels. J. Physiol., London 209 : 567-586, 1970. 8. DANCIS, J. The perfusion Proc, 23 : 701-784, 1964. 9. FABER, J+ J. Application transfer 1969. of inert materials of guinea pig placenta of the theory of heat in placentas. Circulation in situ. exchangers Res. 24: Federation to the 22 l-234, 10. FABER, J. J., AND F. M. HART. The rabbit placenta as an organ of diffusion al exchange. Circulation Res. 19 : 8 16-833, 1966. 11. FABER, J. J. Regulation of fetal placental blood flow. In : Respit-atory Gas Exchange in the Placenta, edited by L. D. Longo and H. BarteIs. Bethesda, Md. : National Institutes of Health, 1972. 12. HILL, E,, P., G, G. POWER, AND L. D. LONGO. A mathematical model of placental 02 transfer with consideration of hemoglobin reaction rates. Am. J. Physiol. 222 : 72 l-729, 1972. 13, HUGGETT, A. ST.G. Foetal blood-gas tensions and gas transfusion through the placenta of the goat. J. Physiol., London 62: 373-384, 1927. 14. KAISER, I. H., AND J* N. CUMMINGS. Hydrogen ion and hemoglobin concentration, carbon dioxide and oxygen content of blood of the pregnant ewe and fetal lamb. J. A#. Physiol. 10: 484-492, 1957, 15. KAISER, I. H., J, N. CUMMINGS, S. R. M. REYNOLDS, AND J. P. MARBARGER. Acclimatization response of the pregnant ewe and O2 TRANSFER 16. 17. 18. 19. 20. 21. IN PERFUSED 1153 PLACENTA fetal lamb to diminished ambient pressure. J. &Z. Physiol. 13 : 171-178, 1958. LAMPORT, H. The transport of oxygen in the sheeps placenta: the diffusion constant of the placenta. Yale J. Biol. Med. 27 : 26-34, 1954-1955. LINGO, 1;. ID., E. P. HILL, AND G. G, POWER. Theoretical analysis of factors affecting placental 02 transfer. Am. J. Physiol. 222: 730-739, 1972. LONGO, L. II., M. DELIVORIA-PAPADOPOULOS, G. G. POWER, E. P. HILL, AND R, E. FORSTER II. Diffusion equilibration of inert gases between maternal and fetal placental capillaries. Am. J. physiol. 219: 561-569, 1970. MESCHIA, G., A. HELLEGERS, J. N. BLECHNER, A. S. WOLKOFF, AND D. H. BARRON. A comparison of the oxygen dissociation curves of the bloods of maternal, fetal and newborn sheep at various pHs. Quart. J, Exptl. Physiol. 46 : 95- 100, 196 1. MESCHIA, G., F. C. BATTAGLIA, AND P. D. BRUNS. Theoretical and experimental study of transplacental diffusion. J. A#d. Physiol. 22 : 1171-l 178, 1967. MESCHIA, G., J. R. COTTER, C. S. BREATHNACH, AND D. H. BARRON. The hemoglobin, oxygen, carbon dioxide and hydrogen 22. 23. 24. 25. 26. 27. ion concentrations in the umbilical bloods of sheep and goats as sampled via indwelling plastic catheters. Quart. J. Exptl. Physiol. 50: 185-195, 1965, METCALFE, J., W. MOLL, H. BARTELS, P. HILPERT, AND J. T. PARER. Transfer of carbon monoxide and nitrous oxide in the artificially perfused sheep placenta, Circulation Res. 16 : 95- 101, 1965. POWER, G. G., E:, P. HILL, AND L. D. LONGO. Analysis of uneven distribution of diffusing capacity and blood flow in the placenta. Am. J. Physioi. 222: 740-746, 1972. POWER, G, G., AND L. D. LONGO. Graphical analysis of maternal and fetal exchange of 02 and CQ. J. Appl. Physiol. 26 : 38-47, 1969. POWER, G. G., L. D. LONGO, N. N. WAGNER, JR., D. E. KUHL, AND R. E. FORSTER II. Uneven distribution of maternal and fetal placental blood flow, as demonstrated using macroaggregates, and its response to hypoxia. J, Clin. Invest. 46 : 2053-2063, 1967. RANKIN, J., G. MESCHIA, E. L. MAKOWSKI, AND F. C. BATTAGLLZA. Macroscopic distribution of blood flow in the sheep placenta. Am. J. Physiol. 219: 9-16, 1970. SNEDECOR, G. W., AND W. G. COCHRAN. Statistid Methods (6th ed.). Ames: Iowa State Univ. Press, 1967, p. 455.