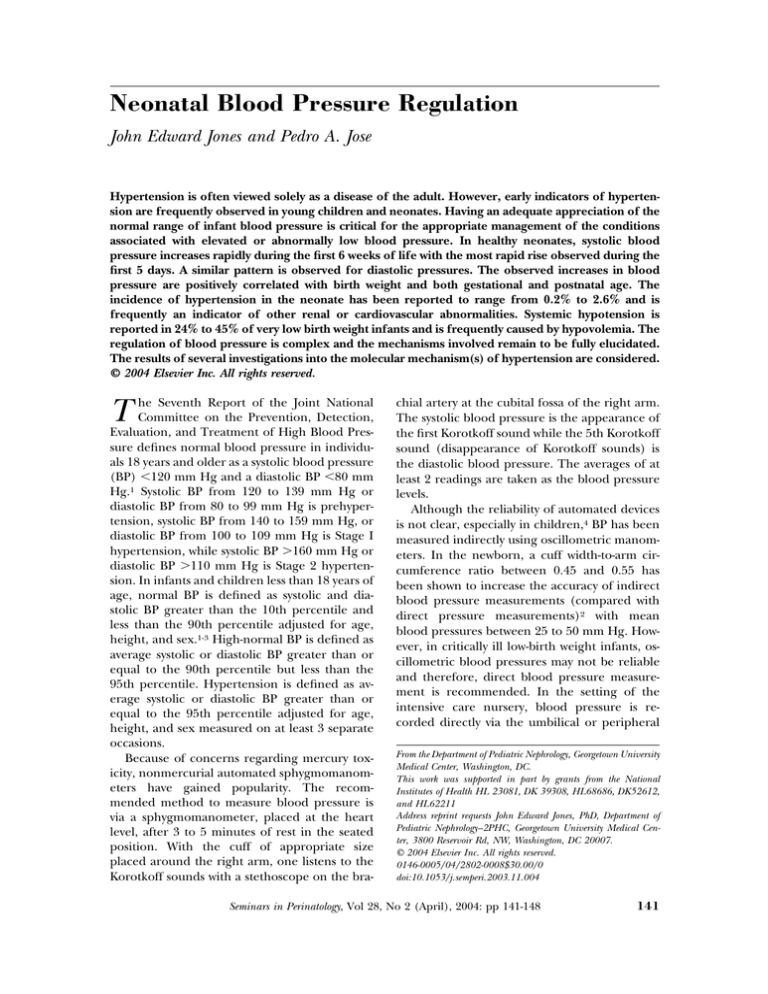
Neonatal Blood Pressure Regulation
John Edward Jones and Pedro A. Jose
Hypertension is often viewed solely as a disease of the adult. However, early indicators of hypertension are frequently observed in young children and neonates. Having an adequate appreciation of the
normal range of infant blood pressure is critical for the appropriate management of the conditions
associated with elevated or abnormally low blood pressure. In healthy neonates, systolic blood
pressure increases rapidly during the first 6 weeks of life with the most rapid rise observed during the
first 5 days. A similar pattern is observed for diastolic pressures. The observed increases in blood
pressure are positively correlated with birth weight and both gestational and postnatal age. The
incidence of hypertension in the neonate has been reported to range from 0.2% to 2.6% and is
frequently an indicator of other renal or cardiovascular abnormalities. Systemic hypotension is
reported in 24% to 45% of very low birth weight infants and is frequently caused by hypovolemia. The
regulation of blood pressure is complex and the mechanisms involved remain to be fully elucidated.
The results of several investigations into the molecular mechanism(s) of hypertension are considered.
© 2004 Elsevier Inc. All rights reserved.
he Seventh Report of the Joint National
Committee on the Prevention, Detection,
Evaluation, and Treatment of High Blood Pressure defines normal blood pressure in individuals 18 years and older as a systolic blood pressure
(BP) ⬍120 mm Hg and a diastolic BP ⬍80 mm
Hg.1 Systolic BP from 120 to 139 mm Hg or
diastolic BP from 80 to 99 mm Hg is prehypertension, systolic BP from 140 to 159 mm Hg, or
diastolic BP from 100 to 109 mm Hg is Stage I
hypertension, while systolic BP ⬎160 mm Hg or
diastolic BP ⬎110 mm Hg is Stage 2 hypertension. In infants and children less than 18 years of
age, normal BP is defined as systolic and diastolic BP greater than the 10th percentile and
less than the 90th percentile adjusted for age,
height, and sex.1-3 High-normal BP is defined as
average systolic or diastolic BP greater than or
equal to the 90th percentile but less than the
95th percentile. Hypertension is defined as average systolic or diastolic BP greater than or
equal to the 95th percentile adjusted for age,
height, and sex measured on at least 3 separate
occasions.
Because of concerns regarding mercury toxicity, nonmercurial automated sphygmomanometers have gained popularity. The recommended method to measure blood pressure is
via a sphygmomanometer, placed at the heart
level, after 3 to 5 minutes of rest in the seated
position. With the cuff of appropriate size
placed around the right arm, one listens to the
Korotkoff sounds with a stethoscope on the bra-
T
chial artery at the cubital fossa of the right arm.
The systolic blood pressure is the appearance of
the first Korotkoff sound while the 5th Korotkoff
sound (disappearance of Korotkoff sounds) is
the diastolic blood pressure. The averages of at
least 2 readings are taken as the blood pressure
levels.
Although the reliability of automated devices
is not clear, especially in children,4 BP has been
measured indirectly using oscillometric manometers. In the newborn, a cuff width-to-arm circumference ratio between 0.45 and 0.55 has
been shown to increase the accuracy of indirect
blood pressure measurements (compared with
direct pressure measurements)2 with mean
blood pressures between 25 to 50 mm Hg. However, in critically ill low-birth weight infants, oscillometric blood pressures may not be reliable
and therefore, direct blood pressure measurement is recommended. In the setting of the
intensive care nursery, blood pressure is recorded directly via the umbilical or peripheral
From the Department of Pediatric Nephrology, Georgetown University
Medical Center, Washington, DC.
This work was supported in part by grants from the National
Institutes of Health HL 23081, DK 39308, HL68686, DK52612,
and HL62211
Address reprint requests John Edward Jones, PhD, Department of
Pediatric Nephrology–2PHC, Georgetown University Medical Center, 3800 Reservoir Rd, NW, Washington, DC 20007.
© 2004 Elsevier Inc. All rights reserved.
0146-0005/04/2802-0008$30.00/0
doi:10.1053/j.semperi.2003.11.004
Seminars in Perinatology, Vol 28, No 2 (April), 2004: pp 141-148
141
142
Jones and Jose
artery catheter. Although the length and size of
the tubing can influence the recorded blood
pressure, 3.5F and 5F umbilical artery catheters
have been shown to adequately reflect the “correct” blood pressure. The site where blood pressure is being measured has to be kept in mind,
especially in conditions in which blood pressures
in the lower and upper extremities or even between the 2 upper extremities may differ (eg,
location of the coarctation of the aorta).
Regulation of Blood Pressure
Blood pressure is generally expressed as the
product of cardiac output and peripheral resistance. However, the relationship between pressure and flow in blood vessels is not linear and
the control mechanisms for pressure regulation
involve more than simply a direct change in
either cardiac output or peripheral resistance.5,6
Blood flow through a vessel is determined by 2
primary factors: the amount of pressure forcing
the blood through the vessel, and the resistance
to flow. The resistance to flow in a blood vessel is
best described as impedance because this takes
into account inertial properties and viscosity of
blood elastic properties of blood vessels, and the
variable geometries of blood vessels during phasic flow. One of the most important factors influencing the flow through the arteries is the
vessel diameter, because the conductance is proportional to the fourth power of the diameter.
Therefore, flow is influenced more by changes
in vascular resistance than by pressure changes.
The short-term adjustment and long-term
control of blood pressure are supplied by a hierarchy of pressure controls. The cardiovascular
reflexes are the most rapidly acting pressure
control mechanisms. They are activated within
seconds and the effects may last a few minutes to
a few days. The pressure controls acting with
intermediate rapidity include capillary fluid
shifts, stress relaxation, and hormonal control
(eg, catecholamines, angiotensin II, vasopressin). These systems, like the cardiovascular reflexes, function to buffer acute changes in pressure. Long-term control is afforded by long-term
regulation of body fluids.
The low systolic blood pressure at birth, due
to low cardiac output and peripheral resistance,
increases rapidly in the first 6 weeks of life (especially in the first 5 days), remains at a constant
level until age 6 years, and increases gradually
until age 18 years. The pattern is similar for
diastolic blood pressure except that there is a
slight decrease in diastolic blood pressure in the
first 6 months of life (relative to the blood pressure in the first week of life). The transient
decrease in diastolic blood pressure in the first 6
months of life is associated with a low intestinal
vascular resistance, mediated by nitric oxide.7
The increase in blood pressure with age in preterm infants occurs as a function of postconceptional age. After 70 years of age, systolic BP
continues to increase but diastolic BP may decrease.
The increase in blood pressure with age is
caused by a rise in both cardiac output and total
peripheral resistance. The age-related changes
in vascular resistance are selective since in the
perinatal period there is a rapid fall in resistance
in the lungs, small intestines, brain, and the
kidney. Moreover, the increase in regional blood
flow with age cannot be accounted for by an
increase in blood pressure. Indeed, in the immediate perinatal period, the increases in regional blood flow with postnatal age is independent of blood pressure.8 In the newborn, cardiac
output is increased mainly by accelerating heart
rate. The high heart rate may be due to differential sympathetic and parasympathetic effects,
hypersensitivity of the cardiac receptors, and peripheral vasodilatation. The low precapillary resistance and low venous capacitance are conducive to high systemic blood flow per unit body
weight, and provide increased tissue perfusion
for growth.
Blood Pressure in Healthy Full-term
Infants
Having an adequate appreciation of the normal
range of infant BP is crucial for the appropriate
management of conditions associated with elevated or low BP. Numerous studies have been
conducted in an attempt to determine the range
of BPs and rate of change in term and pre-term
infants. Although there are few studies documenting the changes in BP with postconceptional age in the first few hours and days of life,
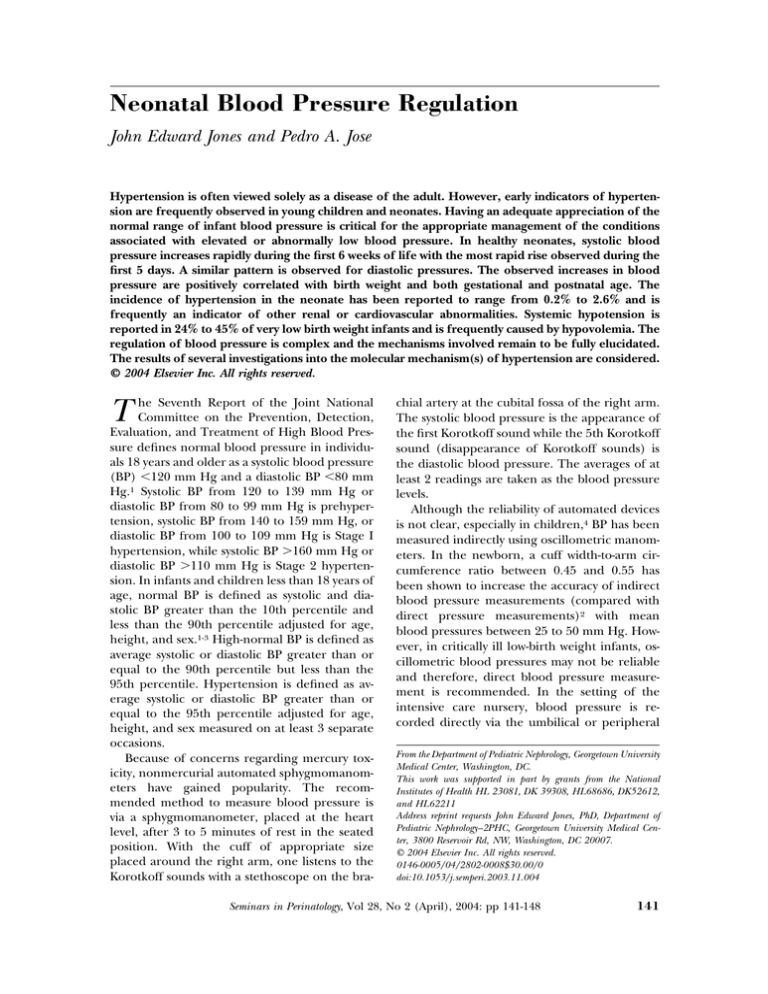
blood pressure is positively correlated with birth
weight and both gestational and postnatal age
with a marked increase in the first 5 days of
postnatal life.2 A nomogram for BP as a function
143
Neonatal Blood Pressure Regulation
of gestational age and birth weight in the first 3
days of life has been constructed.2 The fact that
BP is about 6 to 10 mm Hg higher in awake than
in sleeping babies is not factored in this nomogram. These data mirror those of an earlier
study9 in which the BP of infants was monitored
during the first 96 hours after birth, (see Table
1). BP at three years of age correlated with
length rather than weight. Indeed, the nomograms of BP have height as an important variable.3 In adults, systolic BP is higher in the lower
than in the upper extremities. However, in
healthy newborns, calf BP has been reported to
be 1 to 3 mm Hg lower than arm blood pressures. Calf BPs begin to exceed arm blood pressures by 6 months of age.
ization and subsequent renal embolism.
Thrombosis has been found in 81% percent of
infants with indwelling umbilical artery catheters. A high incidence of hypertension is also
found in infants with bronchopulmonary dysplasia (43%). Rarer causes may be secondary to
neonatal pharmacotherapy (eg, steroids) and
maternal drug use (eg, cocaine).12 Many hypertensive infants subsequently become normotensive by 1 year of age and most babies no longer
need antihypertensive therapy by 2 years of age.
However, there are also reports of significant
morbidity and mortality related to hypertension.
The drugs to use in the neonatal period have not
been standardized and many have not been officially approved for use in this age group. It has
been suggested that in the absence of symptoms
and/or organ involvement, blood pressure less
than 99th percentile should not be treated with
drugs.
Treatment. There are no drugs approved for
the treatment of neonatal hypertension.12 However, there are some prospective reports on the
use of several antihypertensive agents. For example, nicardipine, given as an intravenous infusion (0.5 g/kg/min) decreased blood pressure
by about 20%.13 There are case reports of the
use of angiotensin converting enzyme inhibitors
in the treatment of hypertension in the newborn. Enalaprilat can be given intravenously at a
dose of 15 g/kg/min over a 5- to 10-minute
period and can be repeated every 8 to 24 hours.
Oral enalapril and captopril (0.01 mg/kg as a
starting dose) have also been used. Some drugs
Systemic Hypertension
The definition of hypertension (⬎95th percentile) in infants and children, patterned from
adults with essential hypertension, has been criticized for lack of biological significance.1,3,10 In
the first week of life, the 95th percentile level of
systolic blood pressure is 95 to 96 mm Hg and
104-113 mm Hg from 2 to 6 weeks of age.11 The
incidence of hypertension in the newborn period has been reported to vary from 0.2% to
2.6%. Hypertension in the newborn is often an
indicator of other renal (thrombosis/infarction,
parenchymal disease, obstructive uropathy) or
cardiovascular-related problems (patent ductus
arteriosus, coarctation of the aorta). Older literature suggests that the risk of developing hypertension is increased by umbilical artery catheter-
Table 1. Mean Blood Pressures (MBP) and 10th Percentiles by Birth Weight and Postnatal Age
Hours Postnatal Age
Birth Weight
(grams)
3
12
24
36
48
60
72
84
96
500
600
700
800
900
1000
1100
1200
1300
1400
1500
35/23
35/24
36/24
36/25
37/25
38/26
38/27
39/27
39/28
40/28
40/29
36/24
36/25
37/25
37/26
38/26
39/27
39/27
40/28
40/29
41/29
42/30
37/25
37/26
38/26
39/27
39/27
40/28
40/29
41/29
41/30
42/30
43/31
38/26
39/27
39/28
40/28
40/29
41/29
42/30
42/30
43/31
43/32
44/32
39/28
40/28
42/29
41/29
42/30
42/31
43/31
43/32
44/32
44/33
45/33
41/29
41/29
42/30
42/31
43/31
43/32
44/32
45/33
45/33
46/34
46/35
42/30
42/31
43/31
44/32
44/32
45/33
45/34
46/34
46/35
47/35
48/36
43/31
44/32
44/32
45/33
45/34
46/34
46/35
47/35
48/36
48/36
49/47
44/33
45/33
45/34
46/34
47/35
47/35
48/36
48/37
49/37
49/38
50/38
NOTE. The first set of numbers is the MBP at the given weight and postnatal age and the second figure is the tenth percentile.
Reprinted with permission.9
144
Jones and Jose
used to treat hypertensive emergencies in older
children and adults that should probably be
avoided include diazoxide, nifedipine, and sodium nitroprusside. The duration and magnitude of action of diazoxide and nifedipine may
be unpredictable; thiocyanate levels in the newborn may be unreliable as an indicator of nitroprusside toxicity.14 -adrenergic blockers may
need to be avoided because many newborns with
hypertension have chronic lung disease.
Systemic Hypotension
Systemic hypotension has been reported to be
present in 24% to 45% of very low birth weight
infants.15 In the treatment of neonatal hypotension, blood pressure is the primary endpoint.
However, intact organ blood flow autoregulation is best thought to define the physiologic
range of blood pressure.16 The effects of ductal
and atrial shunts on left and right ventricular
output, respectively, have marked influences on
systemic flow. Because flow to the upper body,
including the brain, is not affected by ductal and
atrial shunts in the premature babies in the perinatal period, superior vena cava flow (SVC) has
been claimed to be a better end point than
blood pressure in the management of hypotensive preterm infants. Indeed, SVC flow correlated well with middle cerebral artery flow and
peri/intraventricular hemorrhage.17,18 SVC is
measured by color Doppler sonography and the
lower limits of normal has been defined as 30,
34, 42, and 46 mL/kg/min respectively at 5, 12,
24, and 48 hours of age.
Systemic hypotension in preterm infants is
caused predominantly by absolute hypovolemia,
as well as abnormal regulation of peripheral vascular resistance (eg, septic shock), and myocardial dysfunction, alone or in combination. Even
in the absence of definitive evidence of hypovolemia, the initial treatment of hypotension usually includes fluid administration (normal saline
given at 10-20 mL/kg over 15-30 minutes). If
blood pressure or SVC flow is not normalized,
pressor agents are added to the treatment. The
agent of choice to increase cardiac output,
blood pressure, or systemic blood flow in the
preterm neonate is not yet settled.16-18 By using
SVC flow as the primary end point, dobutamine
was deemed more beneficial than dopamine in
increasing systemic blood flow.19 However,
death rates and peri/intraventricular hemorrhage were not different between the 2 treatment groups.
Inotropes and Receptors
Dobutamine. (⫹)-dobutamine is a 1-adrenergic agonist and ␣1-adrenergic antagonist, while
(-)-dobutamine is ␣1-adrenergic agonist and
10⫻ less potent than (⫹)-dobutamine as a 1adrenergic receptor agonist. Clinically used dobutamine has both enantiomers. Thus, depending upon which receptor is stimulated, cardiac
output may increase but blood pressure may
decrease. The 2-adrenergic agonist properties
of dobutamine,20 by dilating systemic arteries
may contribute to the decrease in blood pressure.
␣1-Adrenergic receptors. Mammals express 3 ␣1adrenergic receptors: ␣1A (designated as ␣1C
when it was originally cloned), ␣1B, and ␣1D.
␣1A and ␣1D but not ␣1B adrenergic receptors
have been shown to regulate adult blood pressure.21-24 Vascular beds may have receptor subtype specificity. The ␣1A receptor subtype may
govern the contraction of renal and caudal arteries, whereas ␣1D adrenergic receptors may
regulate the contraction of the aorta, femoral,
iliac, and superior mesenteric arteries. Hypertrophy in neonatal cardiac myocytes is mediated
primarily by ␣1A and ␣1B adrenergic receptors.
Aortic hypertrophy, on the other hand, is primarily due to the actions of the ␣1D adrenergic
receptors.
␣2-Adrenergic receptors. Mammals express three
␣2-adrenergic receptors: ␣2A/D, ␣2B, and
␣2C.21 The ␣2A adrenergic receptors mediate
the majority of the classical effects of ␣2 adrenergic stimulation (auto receptor function and
decrease in blood pressure). The ␣2B-adrenergic receptors, in contrast, are predominantly
found outside of the central nervous system at
extrajunctional or postsynaptic sites, produce vasoconstriction and thus counteract the hypotensive effects of ␣2A adrenergic receptor stimulation. The ␣2C-adrenergic receptors do not have
cardiovascular effects but may play a role in
mediating the hypothermic response.
-Adrenergic receptors.21,25-27 The disruption of either the 1 or the 2-adrenergic receptor, both,
or even the 1, 2, and 3-adrenergic receptors,
does not affect heart rate or resting blood pres-
Neonatal Blood Pressure Regulation
sure in mice. Mice that lack the 1-adrenergic
receptor are unresponsive to cardiac -adrenergic receptor stimulation, suggesting that neither
2- nor 3-adrenergic receptors play a role in
the inotropic or chronotropic responses in the
mouse. The hypotensive response to isoproterenol, however, is impaired in both 1 and
2-adrenergic null mice. The 3-adrenergic receptors do not have major effects on the cardiovascular system. An allelic variant of ␣2C (⌬322325) with 1 adrenergic receptor (Arg389) may
increase the risk of heart failure in blacks,28 but
the role these variants may play in the newborn
is not known.
Dopamine. Presynaptic/junctional and postsynaptic/junctional or extrasynaptic dopamine receptors are found in many organs and vascular
beds. Dopamine receptors have also been described in the heart but their function is at
present unknown.29,30 Dopamine also modulates
fluid and sodium intake, via its actions in the
kidney and gastrointestinal tract, and by the regulation of cardiovascular centers that control the
functions of the heart, arteries, and veins. Abnormalities in dopamine production and receptor function accompany a high percentage of
human essential hypertension and several forms
of rodent genetic hypertension. Allelic variants
of genes that encode the regulators of the dopamine receptors, alone or in combination with
genetic variants that encode regulatory proteins
of the renin angiotensin system, are associated
with human essential hypertension.31,32
Dopamine receptors. The circulating levels of dopamine are in the picomolar range and are far
too low to stimulate its own or other receptors.33
Dopamine stimulates its own receptors at nanomolar concentrations. At low micromolar concentrations, dopamine also stimulates -adrenergic receptors, but at 4 to 16 times the
concentration of dobutamine. At low to high
micromolar concentrations, dopamine may also
occupy ␣-adrenergic and serotonin receptors.
Variants of dopamine receptors can affect their
function. There are two classes of dopamine
receptors; the D1-like receptors which are the D1
and D5 receptors (also known as D1A and D1B,
respectively, in rodents) and the D2-like receptors–the D2, D3, and D4. The D1-like receptors
are vasodilatory while the D2-like receptors are
mediators of vasodilation or vasoconstriction depending upon the starting vascular resistance.
145
When vascular resistance is high, the D2-like receptors act as vasodilators by the inhibition of
norepinephrine release. However, when vascular resistance is low, D2-like receptors mediate
vasoconstriction probably via the D3 receptor.33
G protein-coupled receptor kinases. Variations in the
expression or function of G protein-coupled receptor kinases (GRK) have been found to affect
the function of the -adrenergic and dopamine
receptors.34,35 The effect of these variations on
responses in the newborn is unknown. Increased
activity of GRK2 in blood vessels and in the heart
decreases the function of G protein-coupled receptors, including 1- and 2-adrenergic receptors. We have reported that variants of GRK4 are
responsible for the decreased responsiveness of
the D1 dopamine receptor in the kidney in essential hypertension.32,36 Because GRK4 is not
expressed in vascular smooth muscle cells GRK4
gene variants may not be responsible for any
decreased effects of D1 receptors in the newborn. However, GRK4 is expressed in the heart
(unpublished data). As noted, individuals that
are homozygous for ␣2C ⌬322-325-adrenergic
receptor may be at increased risk of developing
heart failure.28 Although the ␣2C ⌬322-325-adrenergic receptor has decreased function, the
disruption of the ␣2C-adrenergic receptor in
mice does not lead to any cardiovascular phenotype. It is possible that increased activity of
GRK2, GRK4, and GRK5 in the heart which is
developmentally-related or acquired may be responsible for decreased effects of inotropic
agents in the newborn.
Cardiac output, blood pressure, and vascular sensitivity
and reactivity to catecholamines with age. As stated, the
increase in blood pressure with age is due to a
rise in both cardiac output and total peripheral
resistance. Age-related changes in vascular resistance are selective since in the perinatal period
there is a rapid fall in resistance in the lungs,
small intestines, brain, and the kidneys while
resistance increases in the femoral vessels.37 The
increase in femoral resistance with age is probably related to both an increase in vascular reactivity to vasoconstrictors and developmental alterations in vascular smooth muscles.
␣-adrenergic receptors. The positive inotropic effect of ␣-adrenergic receptor stimulation is less
in the newborn (rabbits and rats) than in the
adult.38 In contrast, the positive chronotropic
effect of ␣-adrenergic receptor stimulation in
146
Jones and Jose
the newborn is greater in neonatal puppies than
adult dogs.39 The neonatal renal and cerebral
circulations are also more sensitive to ␣-adrenergic stimulation in dogs, pigs, guinea pigs, and
baboons.40,41 The increased ␣-adrenergic receptor effects are correlated with increased ␣-adrenergic receptor density and post receptor events
that may be vessel specific.41,42 It is possible that
the changes in ␣-adrenergic receptor responsiveness with maturation are mediated by the
differential maturation of ␣-adrenergic receptor
subtypes, signal transduction, or effector proteins. However, except in the rat,43 the molecular biological class of these receptors during development has not been studied.
-adrenergic receptors. In the heart, responses to
-adrenergic stimulation increase with age.
However, in many species the myocardial -adrenergic response is associated with a decrease
in -adrenergic density.42,44-47 The decline in
cardiac -adrenergic receptor density with age is
accompanied by an increase in maximum adenylyl cyclase response to -adrenergic stimulation.
However, the neonatal heart is resistant to -adrenergic receptor desensitization compared to
the adult that is not caused by decreased function of GRK2; agonist treatment actually produces sensitization.47 This would suggest, the
decreased -adrenergic effect in the neonates is
not due to increased activity of GRK2.
During the newborn period, in several vascular beds, 2-adrenergic vasodilatory effects are
enhanced.48,49 These changes in renal -adrenergic responsiveness have been correlated with
-adrenergic receptor density in the dog.49 However, these studies were limited because the
-adrenergic receptors were not characterized at
the molecular level and studies in premature
infants were not performed (similar to the drawbacks of the ␣-adrenergic receptor studies).
Dopamine receptors. Dopamine increases renal
blood flow without affecting cerebral hemodynamics in preterm infants.50 The effect of dopamine on intestinal blood flow in this age group
is not consistent. In contrast to the apparent
ability of dopamine to increase renal blood flow
in the preterm human, in other mammals (dog,
pig, and rabbit), the renal vasodilatory effect of
dopamine and the coupling of D1-like receptors
to their effector proteins is less in the young
compared to the adult.51-54 We would like to
suggest that the increase in renal blood flow with
dopamine in the newborn humans may arise, in
part, by occupation of renal -adrenergic receptors.48,49 Serotonin also variably affects renal
blood flow, depending upon the receptor subtype involved and species. Because serotonin-2
receptors induce renal vasodilation, via nitric
oxide, and the nitric oxide effect is increased in
the newborn kidney, a dopaminergic action on
serotonin receptors may also explain the ability
of dopamine to increase renal blood flow in the
newborn. These effects and the increase in cardiac output and systemic pressure with dopamine may explain the ability of dopamine to
increase renal blood flow in the newborn, in
spite of the “immaturity” of dopamine receptor
function. In endotoxin shock in piglets, dopamine caused a greater deterioration in renal
function than volume replacement alone.55
Corticosteroids. Many preterm neonates (humans and baboons) may fail to complete the
complex adrenal adaptive response that occurs
at birth and develop adrenal insufficiency.56 Hydrocortisone has been shown to increase arterial
pressure in hypotensive preterm neonates resistant volume expansion and vasopressor therapy.57 This pressor-resistant hypotension could
be caused by down-regulation of adrenergic receptor abundance or function and a relative or
absolute adrenal insufficiency. Therefore, measurement of cortisol levels in volume-and pressor-resistant infants may identify those with cortisol deficiency as a contributing factor to their
hypotension.
Summary
Great caution should be exercised when comparing the BP measurements obtained in different studies. Measurement of blood pressures in
neonates, especially the low birth weight and
pre-term neonates, is extremely difficult. The
maturation of receptors (adrenergic, dopaminergic, and serotonergic receptors) that regulate cardiac and vascular function affects the
response of the newborn to inotropes and vasoactive agents acting on these receptor subtypes.
It is also possible that nonresponsiveness to
these drugs may not only be related to “immaturity” but also because of the presence of gene
variants that produce receptors with decreased
function and may cause an increase or a decrease in blood pressure. Additionally, func-
Neonatal Blood Pressure Regulation
tional immaturity of the adrenal glands may
cause refractory hypotension, which is independent of dopamine and adrenergic receptor function.
19.
20.
References
1. Chobanian AV, Bakris GL, Black HR, et al: The seventh
report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High
Blood Pressure. JAMA 289:2560-2572, 2003
2. Nuntnarumit P, Yang W, Bada-Ellzey HS: Blood pressure
measurements in the newborn. Clin Perinatol 26:981996, 1999
3. National High Blood Pressure Education Program
Working Group on Hypertension Control in Children
and Adolescents: Update on the 1987 Task Force Report
on High Blood Pressure in Children and Adolescents. A
working group report from the National High Blood
Pressure Education Program. Pediatrics 98:649-658,
1996
4. Barker ME, Shiell AW, Law CM: Evaluation of the Dinamap 8100 and Omron M1 blood pressure monitors
for use in children. Paediatr Perinat Epidemiol 14:179186, 2000
5. Guyton AC: Arterial Pressure and Hypertension, Philadelphia, PA, Saunders, 1980
6. Tibby SM, Murdoch IA: Monitoring cardiac function in
intensive care. Arch Dis Child 88:46-52, 2003
7. Reber KM, Nankervis CA, Nowicki PT: Newborn intestinal circulation. Physiology and pathophysiology. Clin
Perinatol 29:23-39, 2002
8. Yanowitz TD, Yao AC, Pettigrew KD, et al: Postnatal
hemodynamic changes in very-low-birthweight infants.
J Appl Physiol 87:370-380, 1999
9. Watkins AM, West CR, Cooke RW: Blood pressure and
cerebral haemorrhage and ischaemia in very low birthweight infants. Early Hum Dev 19:103-110, 1989
10. Goonasekera CD, Dillon MJ: Measurement and interpretation of blood pressure. Arch Dis Child 82:261-265,
2000
11. Watkinson M: Hypertension in the newborn baby. Arch
Dis Child Fetal Neonatal Ed 86:F78-F81, 2002
12. Flynn JT: Neonatal hypertension: diagnosis and management. Pediatr Nephrol 14:332-341, 2000
13. Milou C, Debuche-Benouachkou V, Semama DS, et al:
Intravenous nicardipine as a first-line antihypertensive
drug in neonates. Intensive Care Med 26:956-958, 2000
14. Gilboa N, Urizar RE: Severe hypertension in newborn
after pyeloplasty of hydronephrotic kidney. Urology 22:
179-82, 1983
15. Al-Aweel I, Pursley DM, Rubin LP, et al: Variations in
prevalence of hypotension, hypertension, and vasopressor use in NICUs. J Perinatol 21:272-278, 2001
16. Seri I: Circulatory support of the sick preterm infant.
Semin Neonatol 6:85-95, 2001
17. Kluckow M, Evans N: Low systemic blood flow in the
preterm infant. Semin Neonatol 6:75-84, 2001
18. Evans N, Kluckow M, Simmons M, et al: Which to measure, systemic or organ blood flow? Middle cerebral
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
147
artery and superior vena cava flow in very preterm infants. Arch Dis Child Fetal Neonatal Ed 87:F181-F184,
2002
Osborn D, Evans N, Kluckow M: Randomized trial of
dobutamine versus dopamine in preterm infants with
low systemic blood flow. J Pediatr 140:183-191, 2002
Goodman and Gilman’s: The Pharmacological Basis of
Therapeutics (ed 10), in Goodman, LS, Limbird LE,
Milinoff PB, et al (eds): New York, NY, McGraw-Hill,
1996
Alexander S, Mathie A, Peters J, et al: TiPS 12th Edition
Nomenclature Supplement, Londonpp1-146, Current
Trends, 2001
Rokosh DG, Simpson PC: Knockout of the ␣1A/C-adrenergic receptor subtype: the alpha 1A/C is expressed
in resistance arteries and is required to maintain arterial
blood pressure. Proc Natl Acad Sci USA 99:9474-9479,
2002
Tanoue A, Koshimizu TA, Tsujimoto G: Transgenic studies of ␣1-adrenergic receptor subtype function. Life Sci
71:2207-2215, 2002
Daly CJ, Deighan C, McGee A, et al: A knockout approach indicates a minor vasoconstrictor role for vascular ␣1B-adrenoceptors in mouse. Physiol Genomics 9:8591, 2002
Chruscinski AJ, Rohrer DK, Schauble E, et al: Targeted
disruption of the 2 adrenergic receptor gene. J Biol
Chem 274:16694-16700, 1999
Rohrer DK, Chruscinski A, Schauble EH, et al: Cardiovascular and metabolic alterations in mice lacking both
1- and 2-adrenergic receptors. J Biol Chem 274:1670116708, 1999
Jimenez M, Leger B, Canola K, et al: 1/2/3-adrenoceptor knockout mice are obese and cold-sensitive but
have normal lipolytic responses to fasting. FEBS Lett
530:37-40, 2002
Small KM, Wagoner LE, Levin AM, et al: Synergistic
polymorphisms of 1- and ␣2C-adrenergic receptors and
the risk of congestive heart failure. N Engl J Med 347:
1135-1142, 2002
Ozono R, O’Connell DP, Wang ZQ, et al: Localization of
the dopamine D1 receptor protein in the human heart
and kidney. Hypertension 30:725-729, 1997
Habuchi Y, Tanaka H, Nishio M, et al: M. Dopamine
stimulation of cardiac -adrenoceptors: the involvement
of sympathetic amine transporters and the effect of
SKF38393. Br J Pharmacol 122:1669-1678, 1997
Jose PA, Eisner GM, Felder RA: Dopamine and the
kidney: Role in hypertension? Curr Opin Nephrol Hypertens 12:189-194, 2003
Felder RA, Sanada H, Xu J, et al: G protein-coupled
receptor kinase 4 gene variants in human essential hypertension. Proc Natl Acad Sci USA 99:3872-3877, 2002
Jose PA, Eisner GM, Felder RA: The renal dopamine
receptors in health and hypertension. Pharmacol Ther
80:149-182, 1998
Eckhart AD, Ozaki T, Tevaearai H, et al: Vascular-targeted overexpression of G protein-coupled receptor kinase-2 in transgenic mice attenuates beta-adrenergic receptor signaling and increases resting blood pressure.
Mol Pharmacol 261:749-758, 2002
Kohout TA, Lefkowitz RJ: Regulation of G protein-cou-
148
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
Jones and Jose
pled receptor kinases and arrestins during receptor desensitization. Mol Pharmacol 63:9-18, 2003
Bengra C, Mifflin TE, Khripin Y, et al: Genotyping essential hypertension SNPs using a homogenous PCR
method with universal energy transfer primers. Clin
Chem 48:2131-140, 2002
Anwar MA, Ju K, Docherty CC, et al: Developmental
changes in reactivity of small femoral arteries in the fetal
and postnatal baboon. Am J Obstet Gynecol 184:707712, 2001
Nakanishi T, Kamata K, Nojima K, et al: Inotropic effect
of phenylephrine and myocardial ␣-adrenergic receptor
in newborn and adult animals. J Mol Cell Cardiol 21:
975-985, 1989
McCormack J, Gelband H, Villafane J, et al: In vivo
demonstration of maturational changes of the chronotropic response to ␣-adrenergic stimulation. Pediatr Res
24:50-54, 1988
Jose P, Slotkoff L, Lilienfield L, et al: Sensitivity of the
neonatal renal vasculature to epinephrine. Am J Physiol
226:796-799, 1974
Longo LD, Ueno N, Zhao Y, et al: Developmental
changes in alpha 1-adrenergic receptors, IP3 responses,
and NE-induced contraction in cerebral arteries. Am J
Physiol 271:H2313-H2319, 1996
Felder RA, Calcagno PL, Eisner GM, et al: Ontogeny of
myocardial adrenoceptors II. Alpha adrenoceptors. Pediatr Res 16:340-342, 1982
Shen H, Peri KG, Deng XF, et al: Distribution of ␣1adrenoceptor subtype proteins in different tissues of
neonatal and adult rats. Can J Physiol Pharmacol 78:237243, 2000
Slotkin TA, Lau C, Seidler FJ: -adrenergic receptor
overexpression in the fetal rat: distribution, receptor
subtypes, and coupling to adenylate cyclase activity via
G-proteins. Toxicol Appl Pharmacol 129:223-234, 1994
Sun LS: Regulation of myocardial -adrenergic receptor
function in adult and neonatal rabbits. Biol Neonate
76:181-192, 1999
Whitsett JA, Noguchi A, Moore JJ: Developmental aspects of ␣- and -adrenergic receptors. Semin Perinatol
6:125-141, 1982
Auman JT, Seidler FJ, Slotkin TA: -adrenoceptor con-
48.
49.
50.
51.
52.
53.
54.
55.
56.
57.
58.
trol of G protein function in the neonate: determinant
of desensitization or sensitization. Am J Physiol Regul
Integr Comp Physiol 283:R1236-R1244, 2002
Nakamura KT, Alden BM, Matherne GP, et al: Ontogeny
of renal hemodynamic response to terbutaline and forskoline in sheep. J Pharmacol Exp Ther 247:453-459,
1988
Felder RA, Jose PA: Development of adrenergic and
dopamine receptors in the kidney, in Strauss J (ed):
Homeostasis, Nephrotoxicity, and Renal Anomalies in
the Newborn Boston, Martinus-Nijhoff, 1986, pp 3–10
Lundstrom K, Pryds O, Greisen G: The haemodynamic
effects of dopamine and volume expansion in sick preterm infants. Early Hum Dev 57:157-163, 2000
Nguyen LB, Lievano G, Radhakrishnan J, et al: Renal
effects of low to moderate doses of dopamine in newborn piglets. J Pediatr Surg 34:996-999, 1999
Pearson RJ, Barrington KJ, Jirsch DW, et al: Dopaminergic receptor-mediated effects in the mesenteric vasculature and renal vasculature of the chronically instrumented newborn piglet. Crit Care Med 24:1706-1712,
1996
Pelayo JC, Fildes RD, Jose PA: Age-dependent renal
effects of intrarenal dopamine infusion. Am J Physiol
247:R212-R216, 1984
Felder RA, Felder CC, Eisner GM, et al: The dopamine
receptor in adult and maturing kidney. Am J Physiol
257:F315-F327, 1989
Chin A, O’Conner LN, Radhakrishnan J, et al: Endotoxemia and the effects of dopamine on renal functions of
neonatal piglets. Biol Neonate 81:196-202, 2002
Yoder B, Martin H, McCurnin DC, et al: Impaired urinary cortisol excretion and early cardiopulmonary dysfunction in immature baboons. Pediatr Res 51:426-432,
2002
Seri I, Tan R, Evans J: Cardiovascular effects of hydrocortisone in preterm infants with pressor-resistant hypotension. Pediatrics 107:1070-1074, 2001
Bourchier D, Weston PJ: Randomized trial of dopamine
compared with hydrocortisone for the treatment of hypotensive very low birthweight infants. Arch Dis Child
76:F174-F178, 1997