School Performance in Adolescents With and Without Periventricular–Intraventricular
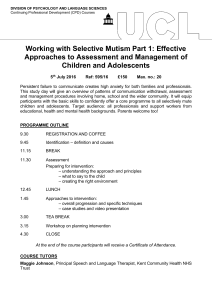
advertisement

School Performance in Adolescents With and Without Periventricular–Intraventricular Hemorrhage in the Neonatal Period Margot van de Bor* and Lya den Ouden† Long-term sequelae of preterm birth have been studied extensively up until the age of 5 to 8 years. However, the cognitive development of adolescents born preterm has received limited attention. The objective of this study is to determine school performance in adolescents born very preterm. We have followed up a cohort of 484 infants born before 32 weeks of gestation in whom cranial ultrasound was routinely and systematically performed. School performance was assessed in the surviving adolescents at 14 years of age. The outcome variable divided the adolescents into three groups: (1) normal, (2) slow learners, and (3) special education. School performance data were obtained from 278 of 304 surviving adolescents; 129 performed normally, while 107 were slow learners, and 42 needed special education. From the unadjusted odds ratios for the need of special education by the various perinatal factors, only the odds ratio for periventricular–intraventricular hemorrhage was significantly associated (2.56, 95% confidence interval 1.17-4.86). Logistic regression analysis revealed that, after correction for possible confounding factors, the odds ratios for special education were significantly higher for adolescents with all grades of periventricular–intraventricular hemorrhage. Less than 50% of adolescents born before 32 weeks gestation perform normally in school. Periventricular–intraventricular hemorrhage, including the lower grades, does have an unfavorable additional effect on school performance. © 2004 Elsevier Inc. All rights reserved. eriventricular–intraventricular hemorrhage (PIVH) in preterm infants has received ample attention in the past two decades. Due to a better understanding of the etiology and improved clinical management and treatment, the incidence of PIVH has declined over the past two decades from 30 to 40% in the early 1980s to less than 20% in the 1990s.1-5 Long-term sequelae of PIVH have been studied extensively up until the age of 5 to 8 years.6-9 The outcome data of children with more severe grades of PIVH are rather consistent. These children suffer mental retardation and cerebral palsy.6,7 However, the outcome of children with lower grades of PIVH is subject for discussion. Some authors report no independent effect of lower grades of PIVH on long-term outcome,10,11 while other researchers describe that children with lower grades of PIVH do have more disabilities and/or handicaps than children without PIVH in the neonatal period.8,12 PIVH impact on the academic achievement of adolescents remains to be explored. We reported before on the neurodevelopmental outcome at the age of 2 and 5 years of very preterm born children with and without PIVH in the P neonatal period, as part of the Project on Preterm and Small for gestational age infants in the Netherlands (POPS).6,13 The aim of this study is to assess school performance at the age of 14 years in the same study cohort. Methods During 1983, infants born in the Netherlands with a gestational age of less than 32 completed weeks and/or a birth weight below 1500 g participated in a prospective national survey on morbidity and mortality, which had a compliance rate of 94%.14 At that time, cranial ultraFrom the *Department of Pediatrics, University of Nijmegen Medical Center, Nijmegen, The Netherlands; and †TNO Prevention and Health, Leiden, The Netherlands. Address reprint requests to Margot van de Bor, MD, PhD, Department of Pediatrics, University of Nijmegen Medical Center, P.O. Box 9101, 6500 HB Nijmegen, The Netherlands; e-mail: m.vandebor@cukz.umcn.nl This study is part of the Project on Preterm and Small for gestational infants in the Netherlands (POPS). © 2004 Elsevier Inc. All rights reserved. 0146-0005/04/2804-0000$30.00/0 doi:10.1053/j.semperi.2004.08.007 Seminars in Perinatology, Vol 28, No 4 (August), 2004: pp 295-303 295 296 van de Bor and den Ouden sound was routinely and systematically performed in 6 of the 8 neonatal intensive care units in the country. We studied prospectively the incidence of PIVH and subsequent neurodevelopmental outcome in a cohort of 484 infants born before 32 completed weeks, ie, all infants within that gestational age group who were admitted to any of the 6 neonatal intensive care units with cranial ultrasound scanning.15 Infants with congenital malformations were excluded from the study. Follow-up data for the surviving children at 2 and 5 years of age have been reported before.6,13 Cranial ultrasound was performed as soon as possible after admission to the neonatal intensive care unit. Further examinations were performed at least twice in the first week of life and weekly thereafter until discharge.2 Each hemorrhage was graded according to its maximal size during the first 2 weeks of life. The grading as described by Papile and coworkers was used: grade I, subependymal hemorrhage; grade II, intraventricular hemorrhage; grade III, intraventricular hemorrhage with ventricular distension; grade IV, parenchymal hemorrhage.15 Three infants in whom no hemorrhage was detected had dilated lateral ventricles on follow-up ultrasound scans and were excluded from the study cohort because they may have had periventricular leukomalacia.6 Serum total bilirubin determinations were done for all infants. They were initiated based on clinical criteria and repeated based on clinical and chemical criteria. The highest observed neonatal serum total bilirubin concentrations were used for our analyses.16 Neurodevelopmental outcome at 5 years was assessed during a home visit by one of three specially trained pediatricians, who were not familiar with the medical history of the child.17,18 Validated standardized tests were used to detect abnormalities in mental development, neurological status, vision and visual functions, hearing, and language and speech. Definitions of normal and abnormal findings in the various fields of neurodevelopment have been described in detail before.18 The World Health Organization classification of impairment, disability, and handicap was used.19 Impairment was defined as any loss or abnormality of psychological, physiological, or anatomical structures or functions. A disability was defined as any restriction or lack (resulting from an impairment) of ability to perform an activity in the manner or within the range considered normal for a human being. A handicap was defined as a disadvantage for a given individual, resulting from an impairment or a disability, that limits or prevents the fulfillment of a role that is normal (depending on age, gender, and social and cultural factors) for that individual. A handicap indicates the disadvantage experienced in society by an individual who lacks orientation, physical independence, mobility, or social integration. A handicap was defined as minor if it interfered, but not seriously, with everyday life and did not require extensive caretaking. A handicap was defined as major if it interfered seriously with everyday life and imposed a severe burden on the child, the caretakers, and society. School attendance at 5 years of age. Since compulsory education starts at the age of 5 years, school attendance (mainstream primary education or special education) was registered at the neurodevelopmental outcome assessment. Maternal education when the child was 5 years of age. The highest obtained diploma or certificate was used to categorize maternal education. A low educational level was defined as either only primary school education or secondary school education for a maximum of 4 years; a middle educational level was defined as a minimum of 5-6 years of secondary school education and less than 4 years of education after the completion of secondary school; a high level of education was considered to be at least 4 years of education after the completion of secondary school (including university degrees). School performance at 9 years of age. The assessment of the school performance at 9 years of age has been described extensively before.20 Questionnaires were sent to the parents of all children who participated in the follow-up study at 5 years of age. The questionnaire dealt with the following items: kind of school (mainstream education or special education), grade, and need for special assistance in school (extra help by teacher, remedial teaching, or speech therapy). One overall school outcome variable was created. The outcome variable divided the children into three groups: (1) normal: children in mainstream education at the appropriate level, either with or without special assistance; (2) slow learners: children in mainstream education one or 297 School Performance in Adolescents Born Preterm more grades below the appropriate level for age, either with or without special assistance; and (3) special education: children in special education. School performance at 14 years of age. Questionnaires regarding school performance were sent to the adolescents. They were requested to complete the questionnaires themselves. If the adolescent was unable to complete the questionnaire, the parents were asked to do so. In the Netherlands, after completing primary school at the age of 12 years, pupils choose one of the three levels of secondary school: (1) university preparatory education (VWO), (2) senior general secondary education (HAVO), or (3) preparatory secondary vocational training (VMBO). The school placement system aims to keep every adolescent in mainstream education. VWO lasts 6 years, HAVO 5 years, and VMBO 4 years. Special secondary education is limited and exists of education for adolescents with either cognitive and behavioral, motor, sensory, or multiple handicaps. One overall school outcome variable was created. This variable divided the adolescents into three groups: (1) normal: adolescents in the appropriate grade for age in one of the three levels of mainstream secondary education; (2) slow learners: adolescents in one of the three levels of mainstream secondary education one or more grades below the appropriate level for age; and (3) special education: adolescents in special education. Statistical Analysis Chi-square tests and analyses of variance were used to study the relationship between school performance at 14 years and various perinatal factors (gestational age, birth weight, gender, ethnicity, PIVH, need of assisted ventilation, maximum serum total bilirubin concentration), neurodevelopmental outcome data at 5 years, and school performance at 5 and 9 years. These tests were also used to determine the relationship between the various PIVH groups and the above-mentioned perinatal, follow-up, and school performance data. Logistic regression analysis was used to estimate the risk for the need of special education in adolescents with PIVH in the neonatal period. The following factors were considered as confounding factors and corrected for in the analysis: gestational age, birth weight, small for gestational age (⬍10th percentile), gender, ethnicity (Western European or other), days of assisted ventilation, maximum serum total bilirubin concentration, and maternal education. A P value of ⬍0.05 was considered to be statistically significant. Results School performance data at the age of 14 years were obtained from 278 (91.5%) of the 304 surviving adolescents. One hundred and twentynine (46.4%) adolescents performed normally in school; 107 (38.5%) appeared to be slow learners, whereas 42 (15.1%) participated in special education. The level of secondary education in relation to school performance is presented in Table 1. When compared with slow learners, adolescents with a normal school performance attended more frequently level A education. No significant relationship, respectively, between gestational age, birth weight, gender, eth- Table 1. School Type in Relation to School Performance at 14 Years of Age in Adolescents Born Very Preterm School Type A. VWO B. HAVO C. VMBO Cognitive/Behavioral Motor Sensory Multiple Unspecified Normal n ⫽ 129 (46.4%) Slow Learner n ⫽ 107 (38.5%) 29 35 65 5 26 76 Special Education n ⫽ 42 (15.1%) 19 6 4 3 10 298 van de Bor and den Ouden nicity, or mean days of assisted ventilation and school performance at 14 years was observed (Table 2). However, adolescents born at a gestational age of 26-27 completed weeks had a poorer school performance than adolescents born after ⱖ28 weeks of gestation. Less than 30% of the adolescents born at 26-27 weeks had a normal school performance, 51.2% were slow learners, and 19.5% needed special education, whereas approximately 50% of the adolescents born after a longer gestation performed normally in school. Adolescents with a PIVH in the neonatal period participated significantly more in special education than adolescents without PIVH. The mean maximum serum total bilirubin concentration in the neonatal period was significantly lower among the slow learners when compared with the other two school performance groups. Adolescents whose mothers had a higher level of education (assessed when the child was 5 years of age) were more likely to be without school problems at the age of 14 years; the difference, however, did not reach statistical significance (Table 3). From the adolescents that were disabled or handicapped at the age of 5 years, significantly more attended special education at 14 years of age than from those that were not handicapped, irrespective of the neurodevelopmental domain. Special education at 14 years of age was strongly related to the participation in special education at 5 as well as at 9 years. The unadjusted odds ratios for the need of special education at 14 years of age by the various perinatal factors are presented in Table 4. It appeared that from the perinatal factors only the unadjusted odds ratio for PIVH was significantly associated with the need of special education (OR 2.56, 95% confidence interval 1.174.86). Maternal education was not associated with the need of special education at 14 years (Table 5). The presence of a disability or handicap at 5 years of age as well as the need for special education at 5 and 9 years of age were all highly associated with the need of special education at 14 years of age. Since from the perinatal factors only PIVH was significantly related to participation in special education at 14 years of age, the study population was divided into three groups according to the presence and severity of PIVH. Table 6 shows the perinatal data in the various PIVH groups. Adolescents with PIVH had a significantly shorter gestational age and needed assisted ventilation significantly longer than those without PIVH. No differences between the vari- Table 2. Perinatal Data in Relation to School Performance at 14 Years of Age Gestational Age (wks) 26-27⫹6 28-29⫹6 30-31⫹6 Birth Weight (g) ⬍ 1000 1000-1249 1250-1499 ⬎1500 Gender Female Male Ethnicity (n ⫽ 274) Western European Other PIVH None All grades Assisted ventilation (days; mean ⫾ SD) Bilirubin (Mol/L; mean ⫾ SD) Normal n ⫽ 129 (46.4) Slow Learner n ⫽ 107 (38.5) Special Education n ⫽ 42 (15.1) 12 (29.3) 52 (49.0) 65 (49.6) 21 (51.2) 39 (36.8) 47 (35.9) 8 (19.5) 15 (14.2) 19 (14.5) NS 19 (35.2) 34 (45.3) 39 (47.6) 37 (55.2) 27 (50.0) 29 (38.7) 29 (35.3) 22 (32.8) 8 (14.8) 12 (16.0) 14 (17.1) 8 (11.9) NS 64 (47.8) 65 (45.1) 52 (38.8) 55 (38.2) 18 (13.4) 24 (16.7) NS 104 (45.0) 24 (55.8) 91 (39.4) 14 (32.6) 36 (15.6) 5 (11.6) NS 97 (44.9) 32 (51.6) 6.8 ⫾ 8.9 190.6 ⫾ 42.0 93 (43.1) 14 (22.6) 8.3 ⫾ 10.3 177.2 ⫾ 39.1 26 (12.0) 16 (25.8) 8.8 ⫾ 10.4 196.8 ⫾ 47.6 *Chi-square test or analysis of variance where appropriate. Percentages within each perinatal factor subgroup are shown between brackets. P* 0.005 NS 0.01 299 School Performance in Adolescents Born Preterm Table 3. Maternal Education, Handicaps at 5 Years, and Primary School Performance at 5 and 9 Years in Relation to Secondary School Performance at 14 Years of Age Maternal Education (n ⫽ 255) Low Middle High Disability or Handicap at 5 years (n ⫽ 274) Overall None Disability of which Handicap Minor Major Disability†/Handicap‡ Mental Neurological Vision Hearing Language/Speech School Performance at 5 Years (n ⫽ 250) Mainstream Special Education School Performance at 9 Years (n ⫽ 248) Normal Slow Learner Special Education Normal n ⫽ 129 (46.4) Slow Learner n ⫽ 107 (38.5) Special Education n ⫽ 42 (15.1) 49 (45.0) 35 (45.5) 41 (59.4) 46 (42.2) 33 (42.9) 18 (26.1) 14 (12.8) 9 (11.6) 10 (14.5) 115 (56.4) 12 (17.1) 4 (10.5) 1 3 80 (39.2) 27 (38.6) 9 (23.7) 7 2 9 (4.4) 31 (44.3) 25 (65.8) 12 13 2/1 4/3 -/2/5/1 6/2 1/-/1/1 18/2 20/13 10/8 2/1 4/2 24/12 0.00 0.00 0.00 0.01 0.00 121 (54.8) - 88 (39.8) 9 (31.0) 12 (5.4) 20 (69.0) 0.00 111 (86.6) 7 (10.6) 3 (6.5) 22 (16.2) 55 (83.3) 19 (41.3) 3 (2.2) 4 (6.1) 24 (52.2) 0.00 P* NS 0.00 *Chi-square test. †Including handicap. ‡A child could be diagnosed as having a disability or handicap in more than one field of neurodevelopment. Percentages within education or handicap subgroups are shown between brackets. ous PIVH groups, respectively, in birth weight, gender, ethnicity, and maximum serum total bilirubin concentration were observed. Table 7 shows data on maternal education and follow-up at 5 years of age in the various PIVH groups. Maternal education did not differ between the PIVH groups. Major handicaps, especially neurological, were observed significantly more in adolescents with grade III/IV PIVH. Significantly more adolescents with PIVH attended special education at 5, 9, as well as at 14 years of age, irrespective of the severity of PIVH (Table 8). Table 9 presents the level of secondary education in relation to school performance in the PIVH groups. With regard to performance in mainstream education, no striking differences between the groups were observed. Twenty-six adolescents of our initial cohort of 304 survivors6,13 did not return the questionnaires. Therefore, their school performance data were not obtained. Five of them had suffered from grade I/II PIVH. They were all hand- icapped at the age of 5 years (4 minor, 1 major), and 3 of them were in special education at the age of 9 years (no school performance data were available from the other 2 at 9 years). One adolescent was diagnosed with grade III/IV PIVH. He was so severely handicapped at the age of 5 years that he was not enrolled in any school program. In none of the other 20 nonresponding survivors was PIVH detected. Five of them were handicapped at the age of 5 years (4 minor and 1 major), and at the age of 9 years, 12 performed normally in school, 4 were slow learners, and 4 needed special education. To determine whether the need for special education at 14 years of age in our study group had causes other than PIVH in the neonatal period, stepwise logistic regression analysis was performed. Special education was used as a dependent variable and gestational age, birth weight, small for gestational age (⬍10th percentile), gender, ethnicity, length of assisted ventilation, maximum serum total bilirubin concen- 300 van de Bor and den Ouden Table 4. Unadjusted Odds Ratios and 95% Confidence Intervals for the Need of Special Education at 14 Years of Age by Perinatal Factors Odds Ratio Gestational Age (wks) 26-27⫹6 28-29⫹6 30-31⫹6 Birth Weight (g) ⬍ 1000 1000-1249 1250-1499 ⬎1500 Gender Male vs. Female Ethnicity Other vs. Western European PIVH All grades Assisted ventilation ⱖ 15 days vs. ⬍ 15 days Bilirubin ⱖ 150 Mol/L vs. ⬍ 150 Mol/L 95% Confidence Interval 1.43 0.97 1 0.57-3.56 0.43-1.91 1.28 1.41 1.41 1 0.45-3.68 0.54-3.68 0.55-3.64 1.24 0.63-2.41 0.57 0.19-1.70 2.56 1.17-4.86 2.04 0.94-4.43 1.62 0.82-3.22 tration, and maternal school education as possible confounding factors. They yielded an estimate of the odds (risk) on the need of special education when the data were adjusted for the confounding factors. The overall risk of the need of special education at 14 years was higher for adolescents with PIVH in the neonatal period when compared with those without PIVH (OR 2.33, 95% confidence interval 1.15-4.75). The OR for adolescents with grade I/II PIVH was 2.10 (95% confidence interval 1.01-4.35), whereas the OR for adolescents with grade III/IV PIVH was 3.99 (95% confidence interval 1.36-11.69). years of age.21 The worrisome finding that less than 50% of this very preterm born cohort had a normal school performance is in accordance with the literature. Hack and coworkers recently reported that very low birth weight survivors at the age of 20 years had an educational disadvantage and were less likely than normal weight controls to be enrolled in postsecondary study.22 Stjernqvist and Svenningsen reported that 38% of surviving extremely preterm born (⬍29 weeks of gestation) children performed at school below grade level at the age of 10 years; 8% performed far below grade level, whereas 30% performed below grade level and received special education within the normal school system.23 This is the first study to describe the effect of PIVH in the neonatal period on school performance in adolescents born preterm. We demonstrate that PIVH in preterm infants carries an increased risk of poor school performance. It has been frequently reported that the lower grades of PIVH do not independently affect long-term outcome.8,12 In this study, however, we observed that the risk of needing special education for adolescents with lower grades of PIVH (grades I/II) increased twofold, when compared with those without PIVH. When we had taken into account the poor neurodevelopmental outcome at 5 years and the need for special education at 9 years of the nonresponders with grade I/II PIVH, the risk would have been even more pronounced. The size of the hemorrhage may have been rather limited in grade I/II PIVH, but the events preceding the hemorrhage and the secondary Table 5. Unadjusted Odds Ratios and 95% Confidence Intervals for the Need of Special Education at 14 Years of Age by Follow-Up Data at 5 Years and Primary School Performance at 5 and 9 Years Discussion The compliance rate of our study was very high (91.5%). The overall school performance of our study cohort did not differ from the school performance of the remaining POPS cohort. School performance in our study cohort, however, was considerably poorer than in the general Dutch population (46.4% versus 80.6% normal performers, 38.5% versus 14.7% slow learners, and 15.1% versus 4.7% in special education) at 14 Maternal Education Low vs. middle and high Disability or Handicap at 5 Years Special Education at 5 Years Special Education at 9 Years Odds Ratio 95% Confidence Interval 1.32 0.61-2.88 17.22 7.60-39.02 22.47 8.96-56.36 29.12 11.22-75.61 301 School Performance in Adolescents Born Preterm Table 6. Perinatal Data in Adolescents With and Without PIVH in the Neonatal Period No PIVH n ⫽ 216 (77.7) PIVH Grade I/II n ⫽ 45 (16.2) PIVH Grade III/IV n ⫽ 17 (6.1) P* 29.4 ⫾ 1.5 1297 ⫾ 329 28.8 ⫾ 1.5 1258 ⫾ 291 28.2 ⫾ 1.5 1192 ⫾ 251 0.00 NS 106 (79.1) 110 (76.4) 17 (12.7) 28 (19.4) 11 (8.2) 6 (4.2) NS 179 (77.5) 33 (76.7) 6.3 ⫾ 8.6 184.6 ⫾ 42.2 38 (16.5) 7 (16.3) 10.9 ⫾ 10.7 190.5 ⫾ 46.5 14 (6.1) 3 (7.0) 15.9 ⫾ 13.7 196.8 ⫾ 29.6 NS Gestational Age (wks; mean ⫾ SD) Birth Weight (g; mean ⫾ SD) Gender [n, (%)] Female Male Ethnicity [n, (%)] (n ⫽ 274) Western European Other Assisted Ventilation (days; mean ⫾ SD) Bilirubin (Mol/L; mean ⫾ SD) 0.00 NS *Chi-square test or analysis of variance where appropriate. effect on corticogenesis and connectivity in the developing brain appear to be more harmful than previously acknowledged. Stewart and coworkers demonstrated that magnetic resonance imaging of the brains of 14-year-old adolescents born very preterm showed more lesions, eg, abnormalities of ventricles, corpus collosum, and white matter, than were observed by brain ultrasound imaging in the neonatal period.24 In that study, hemorrhages with parenchymal involvement were associated with permanent sequelae on magnetic resonance imaging. The observed abnormalities expressed themselves primarily in quantitative behavioral abnormalities rather than more conventional neurological impairments. Maalouf and coworkers detected with magnetic resonance imaging that all preterm infants ⬍30 weeks gestation, which had suffered from PIVH in the first days of life, further developed cerebral abnormalities until term.25 Inder and coworkers demonstrated that, at the term equivalent date, preterm infants, even those without periventricular white matter injury, have significantly smaller volumes of cerebral cortical gray matter than term infants.26 The quality of the ultrasound equipment that Table 7. Maternal Education and Follow-Up Data at 5 Years of Age in Adolescents With and Without PIVH in the Neonatal Period Maternal Education (n ⫽ 255) Low Middle High Disability or Handicaps at 5 Years (n ⫽ 274) Overall None Disability of which Handicap Minor Major Disability†/Handicap‡ Mental Neurological Vision Hearing Language/Speech No PIVH n ⫽ 216 PIVH Grade I/II n ⫽ 45 PIVH Grade III/IV n ⫽ 17 86 (43.7) 56 (28.4) 55 (27.9) 18 (41.9) 15 (34.9) 10 (23.2) 5 (33.3) 6 (40.0) 4 (26.7) 164 (77.0) 49 (23.0) 23 (10.8) 13 (6.1) 10 (4.7) 29 (64.4) 16 (35.6) 11 (24.4) 7 (15.5) 4 (8.9) 11 (68.7) 5 (31.3) 4 (25.0) 4 (25.0) 0.00 18/10 8/4 1/1 5/2 34/11 9/6 4/4 1/2/1 12/4 1/3/3 -/-/1/- NS 0.00 NS NS NS *Chi-square test. †Including handicap. ‡A child could be diagnosed as having disability and handicap in more than one field of neurodevelopment. Percentages within each PIVH subgroup are shown between brackets. P* NS 302 van de Bor and den Ouden Table 8. School Performance at 5, 9 and 14 Years of Age in Preterm Born Adolescents With and Without PIVH in the Neonatal Period School Performance at 5 Years (n ⫽ 250) Mainstream Special Education School Performance at 9 Years (n ⫽ 248) Normal Slow Learner Special Education School Performance at 14 Years (n ⫽ 278) Normal Slow Learner Special Education No PIVH n ⫽ 216 PIVH Grade I/II n ⫽ 45 PIVH Grade III/IV n ⫽ 17 P* 178 (91.3) 17 (8.7) 31 (77.5) 9 (22.5) 12 (80.0) 3 (20.0) 0.02 107 (55.4) 57 (29.5) 29 (15.0) 22 (55.0) 5 (12.5) 13 (32.5) 7 (46.7) 4 (26.7) 4 (26.7) 0.04 97 (44.9) 93 (43.1) 26 (12.0) 25 (55.6) 10 (22.2) 10 (22.2) 7 (41.2) 4 (23.5) 6 (35.3) 0.00 *Chi-square test. Percentages within the PIVH subgroups are shown between brackets. was used in this study in 1983, the year in which the study population was born, did not meet the quality standards we apply today. Five-megahertz transducers were still in use at that time. They were sensitive enough to detect PIVH reliably,24 but not to diagnose parenchymal cystic lesions. Therefore, detection of periventricular leukomalacia could not be reliably performed. We excluded three children from our cohort because they appeared to have dilated lateral ventricles on follow-up ultrasound scans without a detectable PIVH on the previous scans. Those infants could very likely have had periventricular leukomalacia.6 Despite the widely accepted policy in The Netherlands to withdraw life support from preterm infants with a very poor neurodevelopmental prognosis, eg, infants with severe periven- tricular hemorrhages, we still observed an almost fourfold increased risk for the need of special education in adolescents with grade III/IV PIVH in the neonatal period when compared with adolescents without PIVH. The incidence of PIVH in preterm infants ⱖ26 weeks of gestation has decreased in most neonatal intensive care units over the past two decades. The occurrence of PIVH appears to be gestational age-dependent; the shorter the gestation, the higher the risk of developing PIVH.2 Since survival rates of infants born after extremely short gestational ages (⬍26 weeks) have increased over the past decade,27 the beneficial effect of the reduction in PIVH for the longterm outcome may be blunted by the survival of infants of extremely short gestation. Considering the poor school performance of adolescents Table 9. Level of Secondary Education in Relation to School Performance at 14 Years of Age in Preterm Born Adolescents With and Without PIVH in the Neonatal Period No PIVH n ⫽ 216 Level A. VWO B. HAVO C. VMBO Cognitive/behavioral Motor Sensory Multiple Unspec. Normal n ⫽ 97 Slow learner n ⫽ 93 23 25 49 5 22 66 PIVH Grade I/II n ⫽ 45 Special education n ⫽ 26 11 4 2 2 7 Normal n ⫽ 25 Slow learner n ⫽ 10 5 8 12 — 4 6 PIVH Grade III/IV n ⫽ 17 Special education n ⫽ 10 5 — 1 1 3 Normal n⫽7 Slow learner n⫽4 1 2 4 — — 4 Special education n⫽6 3 2 1 — — School Performance in Adolescents Born Preterm born between 26 and 32 weeks gestation, the future academic achievement of infants born before 26 weeks of gestation is a great concern. Conclusion We observed that less than 50% of adolescents born before 32 weeks gestation have a normal school performance. While PIVH, even the lower grades, was related to disability at the age of 5 years, we now demonstrate that PIVH also has an unfavorable additional effect on school performance. References 1. van de Bor M, Van Bel F, Lineman R, et al: Perinatal factors and periventricular-intraventricular hemorrhage in preterm infants. Am J Dis Child 140:1125-1130, 1986 2. van de Bor M, Verloove-Vanhorick SP, Brand R, et al: Incidence and prediction of periventricular–intraventricular hemorrhage in very preterm infants. J Perinat Med 15:333-339, 1987 3. Philip AG, Allan WC, Tito AM, et al: Intraventricular hemorrhage in preterm infants: Declining incidence in 1980’s. Pediatrics 84:797-801, 1989 4. Hack M, Wright LL, Shankaran S, et al: Very-low-birthweight outcomes of the National Institute of Child Health and Human Development Neonatal Network, November 1989 to October 1990. Am J Obstet Gynecol 172:457-464, 1995 5. Volpe JJ: Intracranial hemorrhage: Germinal matrix-intraventricular hemorrhage of the premature infant, Volpe JJ (ed): Neurology of the Newborn (4th ed) Philadelphia, PA, WB Saunders, 2001, pp 428 – 493 6. van de Bor M, Ens-Dokkum M, Schreuder AM, et al: Outcome of periventricular–intraventricular haemorrhage at five years of age. Dev Med Child Neurol 35:3341, 1993 7. Vohr BR, Ment LR: Intraventricular hemorrhage in the preterm infant. Early Hum Dev 44:1-16, 1996 8. Whitaker AG, Feldman JF, Rossem RV, et al: Neonatal cranial ultrasound abnormalities in low birth weight infants: Relation to cognitive outcomes at six years of age. Pediatrics 98:719-729, 1996 9. Roth SC, Baudin J, McCormick DC, et al: Relation between ultrasound appearance of the brain of very preterm infants and neurodevelopmental impairment at eight years. Dev Med Child Neurol 35:755-768, 1993 10. Cooke RWI: Early and late cranial ultrasonographic appearances and outcome in very low birthweight babies. Arch Dis Child 62:931-937, 1987 11. DeCostello AM, Hamilton PA, Baudin J, et al: Prediction of neurodevelopmental impairment at four years from brain ultrasound appearance of very preterm infants. Dev Med Child Neurol 30:711-722, 1988 303 12. Ment LR, Schneider KC, Ainley MA, et al: Adaptive mechanisms of developing brain. The neurologic assessment of the preterm infant. Clin Perinat 27:303-323, 2000 13. van de Bor M, Verloove-Vanhorick SP, Baerts W, et al: Outcome of periventricular-intraventricular hemorrhage at 2 years of age in 484 very preterm infants admitted to 6 neonatal intensive care units in The Netherlands. Neuropediatrics 19:183-185, 1988 14. Verloove-Vanhorick SP, Verwey RA, Brand R, et al: Neonatal mortality risk in relation to gestational age and birthweight. Results of a national survey of preterm and very low birthweight infants. Lancet 1:55-57, 1986 15. Papile L-A, Burstein J, Burstein R, et al: Incidence and evolution of subependymal and intraventricular hemorrhage: A study of infants with birth weights less than 1,500 gm. J Pediatr 92:529-543, 1978 16. van de Bor M, Ens-Dokkum M, Schreuder AM, et al: Hyperbilirubinemia in low birth weight infants and outcomes at 5 years of age. Pediatrics 89:359-364, 1992 17. Veen S, Ens-Dokkum M, Schreuder AM, et al: Impairments, disabilities and handicaps of very preterm and very low birthweight infants at 5 years of age. Lancet 338:33-36, 1991 18. Schreuder AM, Veen S, Ens-Dokkum M, et al: Standardised method of follow-up assessment of preterm infants at five years of age: Use of the WHO-classification of impairments, disabilities and handicaps. Paediatr Perinat Epidemiol 6:363-380, 1992 19. WHO International Classification of Impairments, Disabilities, and Handicaps. Geneva, World Health Organization, 1980, p 207. 20. Hille ETM, Den Ouden AL, Bauer L, et al: School performance at nine years of age in very premature and very low birth weight infants: Perinatal risk factors and predictors at five years of age. J Pediatr 125:426-434, 1994 21. Centraal Bureau voor de Statistiek. http://statline.cbs.nl 22. Hack M, Flannery DJ, Schluchter M, et al: Outcomes in young adulthood for very-low-birth-weight infants. N Engl J Med 346:149-157, 2002 23. Stjernqvist K, Svenningsen NW: Ten-year follow-up of children born before 29 gestational weeks: Health, cognitive development, behaviour and school achievement. Acta Paediatr 88:557-562, 1999 24. Stewart AL, Rifkin L, Amess PN, et al: Brain structure and neurocognitive development and behavioural function in adolescents who were born preterm. Lancet 353: 1653-1657, 1999 25. Maalouf EF, Duggan PJ, Rutherford MA, et al: Magnetic resonance imaging of the brain in extremely preterm infants: normal and abnormal findings from birth to term. J Pediatr 135:351-357, 1999 26. Inder TE, Anderson NJ, Warfield SK, et al: Assessment of brain volumes in the premature infant: Comparison of cranial ultrasound measurements with quantitative volumetric MRI at term. Pediatr Res 51:452(abstr), 2002 27. Hack M, Fanaroff AA: Outcomes of children of extremely low birthweight and gestational age in the 1990’s. Early Human Dev 53:193-218, 1999