Gestation and Foaling
advertisement

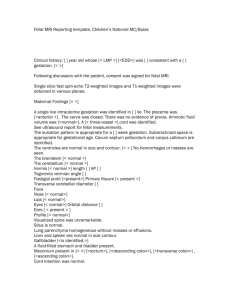
Gestation and Foaling Gestation Length • Average 338-343 days. • Normal gestation can range from 320-380 days. Gestation Length • Gestation length shorter in TB and SB (325-340) than Draft mares (350375d) • Mares bred in late winter & early spring have gestation lengths that average 10 d longer then those born in summer. • Mares with fillies foal on average 3 d earlier Early Embryo • 5-6 days enters uterus • Migrates to day 16. – Embryo migrates in the uterus for ~ 16 days to release a 'signal' that pregnancy is established. – Fixation of the embryo (gestational sac) occurs at ~ 16 days post ovulation Equine Gestation Hormones Progesterone/Progestogens • Progesterone initially rises, followed by a slight ↓ then ↑ to a peak at d 80, then gradually ↓ to 1-2 ng/ml during mid-late gestation (d 150). • Second ↑ associated with formation of accessory & secondary CL. • The 5 α pregnanes rise from mid gestation to term. – Produced from maternal cholesterol • Late gestation progestagen rises (last month of pregnancy) Equine Gestation Hormones Estrogens • Mare ovarian estrogens begin to ↑ at d 38-40. – From gonadotropin stimulation of luteal tissue – Late in gestation maternal estrogen production ↑. • D 70-80 a 2nd ↑ of estrogens from the fetal-placental unit occurs. – Secreted by fetal gonads. • • Fetal estrogens peak at about 210 d & decline & are basal Estrogens appear in the mare's urine in large amounts in the latter half of gestation. – Estrone sulfate: Can be measured with a kit. Derived from the placenta, it is an indicator of fetal viability. It declines within a few days of fetal death. Equine Gestation Hormones Equine Chorionic Gonadotropin (eCG) • 36-38 days - fetal tissue along the chorionic girdle begin to invade the endometrium & form the endometrial cups. • Endometrial cups - eCG-Equine Chorionic Gonadotropin • Produced ~ d 37-42, • Peak - d 60-80 • Endometrial cups start to decline, disappearing around d 120-150. • Causes luteinization of follicular waves to create secondary CLs. • Has an FSH-like action in many other species, it has LH-like activity in mares. Placenta • Placenta takes over progestagen production ~d 100 until foaling. • Complete placental formation is done at 150 days. DAY 150 - Firm placental attachment Impending Birth Vaccinate & Deworm 30 day prior Most Obvious • Hypertrophy mammary glands obvious from 8th month – Maiden may display little until just before foaling • Distention of the teats 4-6 d pre-foaling • Waxing of the teats 1-72 hrs pre-foaling • An increase in milk Ca 1-3 d pre-foaling Impending Birth More Subtle Signs • Softening and flattening of the muscles in the croup • Vulva becomes relaxed & elongated. Maximal hours before parturition • Visible changes in the position of the foal • Vulva – thick & puffy with edema and may elongate Stages of Parturition • Stage 1 – Onset: initial uterine contractions – End: rupture of chorioallantois (water bag) – 1-2 hr – Mare may stand up, lie down, roll, pace, look or bite at flanks, sweat, urinate Stages of Parturition • Stage 2 – Onset: rupture of chorioallantois – End: delivery of fetus – Timeline 30 min – Contractions occur in groups of 3-4 followed by a rest period of 3 to 5 minutes • When the chest is through the vulva the foal can breathe on its own. May go in & remove the amniotic sac. • Not breathing – rub foal, take straw and put in nose, breath into nose Foaling Emergencies May Need Assistance • Red mass evident at vulva (placenta seperation) • Strong straining & no feet evident at vulva within 5 min • Heavy straining with feet in vulva but no further progress in 10 min • One foot missing • No progress for more than 15 min after first water breaks • Rectovaginal perforation occurs • Mare foals while standing “Red Bag” Stages of Parturition • Stage 3 – Onset: delivery of fetus – End: passage of the fetal membranes – Expel placenta 1- 3 hrs post-foaling •Examine Placenta Fetal Membranes at Parturition • Allantochorion - Fusion of the allantois with the chorion results in the allatochorion. At term ~2/3 of placental weight. – Chorionic (villous) surface is intimately applied to the maternal endometrium and is responsible for the formation of microcotyledonary attachments. Grossly, it appears as a red velvet surface • Allantoamnion - allantois surrounds the amnion by the 4th week of gestation, forming the allantoamnion. – At term, this membrane is white and opaque, with large blood vessels coursing over the inner surface. – 1/3 of weight at term Fetus @ 3 months Fetal Membranes at Parturition • Umbilical cord - Results from the expansion of the amnion & allantois around the remnants of the yolk sac & vitelline duct – Anchors the fetus to the original implantation site at the base of the gravid horn on the dorsal wall of the uterus. – Cord length is directly correlated with the weight of the allantoamnion and the allantochorion. Important Features of the Equine Placenta • Cervical star visible as a region without the red villi and has radiating, bare, white areas from its center • Allantochorionic Pouches Maternal rejection of the endometrial cups results in their sloughing into adjacent invaginations of the overlying allantochorion. These appear as pedunculated structures forming a ring around the site of umbilical cord attachment at the dorsal wall of the pregnant horn. • Hippomanes are yellowish/green pasty concentration products of fetal urine and contain large numbers of birefringent crystals Placental with fetus showing the "cervical star", site of future rupture of membranes. Placenta Examination •Arrange the membranes in a capital "F" position, with the pregnant horn uppermost and the body forming the vertical bar of the "F" •Tip of the nonpregnant horn is the most likely part of the placenta to be retained •Placenta Examination •Weight •Length of umbilical cord & location •Appearance of gross lesions, missing pieces Allantochorion • • • Usually expelled with the allantoic surface outermost Examine both chorionic and allantoic surfaces. Color – Rich red or maroon color with the gross appearance of a velvet-like surface. – Pale or fibrotic areas indicate sites of placental detachment or lack of microcotyledon formation – Nonpregnant horn is generally paler than the rest of the chorion. • Thickness – Compared with the pregnant horn, the non-pregnant horn is thinner in section, puckered, and smaller in size. Allantochorion • Body Pregnancy – Although usually resident in one uterine horn with extension into the body of the uterus, the occasional fetus will develop largely within the body of the uterus. The characteristic placental finding is short, symmetrical placental horns • Exudate – Presence may be considered as presumptive evidence of microbial intrauterine infection Allantochorion Chronic Inflammation Cervical Star • Cervical Star Thickening – majority of Intrauterine infections ascend through an incompetent cervix. – Gross thickening, exudate, and a line of demarcation between this area and the adjacent placental body are characteristic findings of placentitis • Allantoamnion – assessed for uniform thickness and color – smooth, white, opaque, uniformly thin membrane. Allantochorion • Umbilical Cord – Assessment of length, degree of twisting, and the presence of any vascular compromise – Abnormal findings include cord seperation, excessive rotation, kinking, aneurysms, intramural hematomas, thrombosis, edema – 95% of normal equine pregnancies, the umbilical cord measures between 36 and 83 cm, with an average length of 55 cm Postpartum Mare & Foal Care Umbilical Cord Care • Allow foal to break fetal membranes. • Never cut the cord. • Spray umbilical cord stump with antiseptic solution 3-4X per day for 3-4 days Ascending placentitis Premature seperation Retained Placenta: Treatment • • • • • • • After 2 hrs Oxytocin Infusion of fluid into allantoic cavity Antibiotics Non-sterioidal anti-inflammatory drugs Frog support pads Deeply bedded stall Colostrum • First milk secreted by a mare coming into lactation Production • During last 2-4 weeks of gestation • Under hormonal influences Importance • Transfer of passive immunity to the suckling foal (“Liquid Gold”) Specificity of protection achieved by vaccinating pregnant mares 3060 days before parturition • Produced only once – beware of leakage! • Provides energy to foal • Encourages passage of meconium Colostrum Quality • Relates directly to antibody content • Good quality: ≥ 50 (70) g/L IgG and specific gravity > 1.060 Thick, sticky, yellow secretion Colostrum Quality • Decreased quality: Maiden mares and mares > 15 y of age Certain breeds (Standardbred) Shorter gestation (early foals) Sick mares Poor foaling conditions Colostrum Evaluating Colostrum Quality Colostrometer • Measures specific gravity/density of colostrum • Approx. 6 ml of colostrum needed • Specific gravity >1.060 indicates good quality Colostrum Evaluating Colostrum Quality ARS Refractometer • Designed for measurement of sugar concentration of solutions (BRIX type) • 1-2 drops of colostrum needed • Results in less than 1 minute http://www.arssales.com/equine/html/refractometer.html Colostrum Evaluating Colostrum Quality ARS Refractometer - Results Colostrum Volume • Average total volume: 5 liters (3.2-7.0 l) • Primiparous < multiparous mares • Decreased in stressed, injured or ill mares • Decreased in mares with mastitis or other damage to udder Colostrum Evaluating Colostrum Quality When? • Assess before foal suckles How? • Physical appearance Thick, sticky, yellow secretion indicates good quality Dilute, white or translucent secretion indicates poor quality Stall Side Tests Banking of Colostrum • Only good quality colostrum • Storage at -20ºC: – IgG concentration stable for 12 months – Other immune components (complement, etc) and nutritional components decrease significantly • Storage at -70ºC: – Permanent maintenance of all components Passive Transfer • Successful passive transfer depends on precise sequence of events – Antibodies must be present in colostrum – GI tract must absorb the large proteins whole- “pinocytosis” • Foal must receive within 1st 8-12 hrs of life • Requires 8-12 hours for antibodies to show up in the blood • Uptake declines to almost zero by 12-24 hours Antibody levels in Foal 1200 Mare IgG Foal IgG 1000 800 600 400 200 0 1 2 3 4 5 6 7 8 9 10 11 12 wk wk wk wk wk wk wk wk wk wk wk wk •Foal produced antibodies first appear in blood stream at about 3 weeks of age •Normal adult levels of foal produced antibodies by 4-5 months Foal Immune Status What are safe levels of IgG in the foal? • True safe levels not known • Goal: serum IgG > 800 mg/dl • If < 800 mg/dl = Failure of Passive Transfer (FPT) - As high as 20% of all foals Marginal FPT: IgG 400-800 mg/dl Partial FPT: IgG 200-400 mg/dl Complete FPT: IgG < 200 mg/dl Foal Immune Status Evaluation of serum IgG status When? Typically at 12-24 h after birth Peak serum levels of IgG achieved by 18h Absorption of immunoglobulins from small intestine essentially complete If failure of passive transfer: treat with IV plasma Can measure early at 6-12 h IgG first detected in foal’s serum at 6 h of age If no IgG or very low level at 6-12 h: can give colostrum to increase levels Foal Immune Status Evaluation of serum IgG status Snap Foal IgG Test • ELISA • Use whole blood, serum, or plasma • Calibrator spots indicate IgG levels of 400 and 800 mg/dl • Sample color is proportional to IgG content • Results in 10-15 min. • Expensive but convenient