SRS and SBRT are Ablative Therapies
advertisement
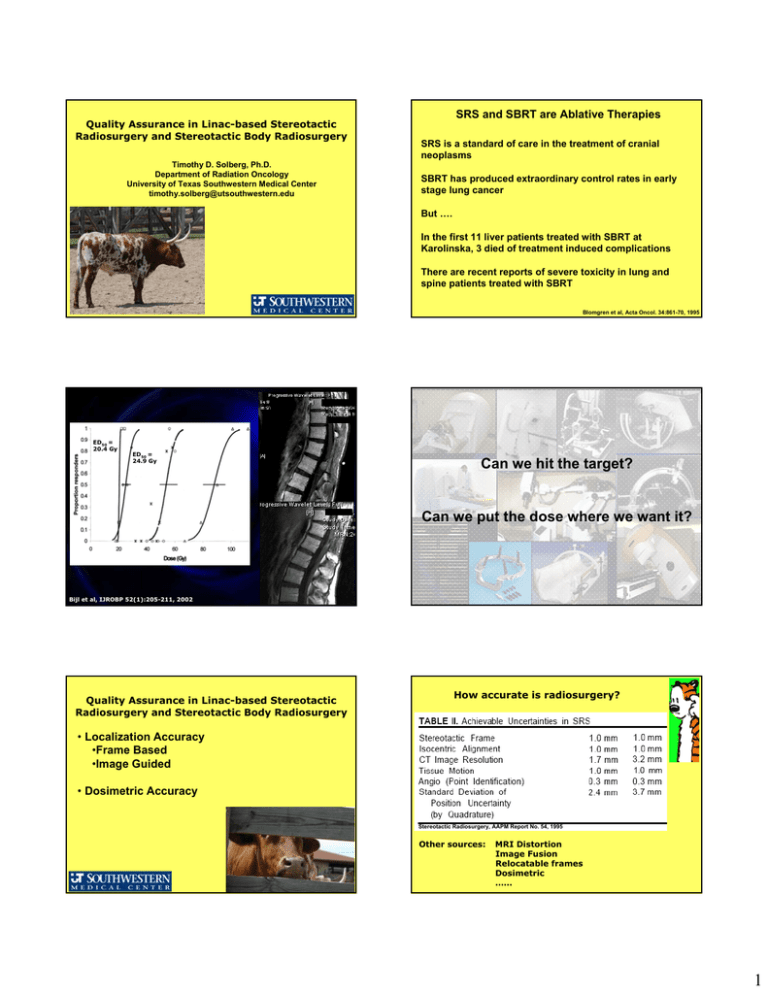
Quality Assurance in Linac-based Stereotactic Radiosurgery and Stereotactic Body Radiosurgery Timothy D. Solberg, Ph.D. Department of Radiation Oncology University of Texas Southwestern Medical Center timothy.solberg@utsouthwestern.edu SRS and SBRT are Ablative Therapies SRS is a standard of care in the treatment of cranial neoplasms SBRT has produced extraordinary control rates in early stage lung cancer But …. In the first 11 liver patients treated with SBRT at Karolinska, 3 died of treatment induced complications There are recent reports of severe toxicity in lung and spine patients treated with SBRT Blomgren et al, Acta Oncol. 34:861-70, 1995 ED50 = 20.4 Gy ED50 = 24.9 Gy Can we hit the target? Can we put the dose where we want it? Bijl et al, IJROBP 52(1):205-211, 2002 Quality Assurance in Linac-based Stereotactic Radiosurgery and Stereotactic Body Radiosurgery How accurate is radiosurgery? • Localization Accuracy •Frame Based •Image Guided • Dosimetric Accuracy Stereotactic Radiosurgery, AAPM Report No. 54, 1995 Other sources: MRI Distortion Image Fusion Relocatable frames Dosimetric …… 1 Frames & CT What About Body Frames? Invasive Non-invasive Maciunas et al, Neurosurgery 35:682-695, 1995 First successful spinal application Rigid skeletal fixation above and below the involved segments Linac delivery with circular collimators / arcs or IMRT System accuracy ≤ 2.0 mm 8-10 Gy Rx with no portion of cord receiving > 3 Gy Stereotactic Body Frame Reproducibility 5-8 mm for 90% of setups Diaphragmatic movement limited to 5-10 mm with pressure. Lax et al, Acta Oncol. 33:677-83, 1994 Setup accuracy evaluated in 30 patients using CT and port films; conclude that a 5 mm margin for PTV is sufficient if CT is performed prior to every treatment. Deviation of < 10 mm (AP and Lat) in 98% of targets. Wulf et al, Radiotherapy Oncology 55:225-236, 2000 Hamilton et al, Neurosurgery 36; 311-319, 1995 Other Frame Based SBRT Systems Negoro et al, IJROBP 50:889-898, 2001 In the initial characterization of the stereotactic body frame, the authors observed what reproducibility in patient setup 90% of the time: 1. less that 2.0 mm 2. 2.0 to 5.0 mm 3. 5.0 to 8.0 mm 4. 8.0 to 11.0 mm 5. > 12.0 mm Yenice Lohr al,al, IJROBP IJROBP 45:521-527, 55:583-593, 1999 2003Herfarth et al, IJROBP 46:329-335, 2000 Shiu etet 57:605-613, 2003 SBRT QA Rule #1: NO SBRT without modern image guidance 2 In the initial characterization of the stereotactic body frame, the authors observed what reproducibility in patient setup 90% of the time: 1. less that 2.0 mm 2. 2.0 to 5.0 mm 3. 5.0 to 8.0 mm 4. 8.0 to 11.0 mm 5. > 12.0 mm Correct answer: 3 Isocentric Accuracy: The Winston-Lutz Test Lax et al, Acta Oncol. 33:677-83, 1994 Mechanical Uncertainties Is the projection of the ball centered within the field? A daily Lutz test is extremely important because: • The mechanical isocenter can shift over time • The AMC board in Varian couches can fail • The cone or MLC may not be repositioned perfectly after service Before (right) and After (left) relatively simple couch adjustment Isocentric Accuracy: The Winston-Lutz Test Is the projection of the ball centered within the field? Good results ≤ 0.5 mm A Lutz test with the MLC is also important because: • The Cone-based Lutz test does not tell you anything about the mechanical isocenter of the MLC • The MLC may not be repositioned perfectly after service Lutz test with 12 x 12 mm MLC field 3 End-to-end testing: evaluating multiple sources of uncertainty Structure Cylinder Cube Cone Sphere AP 0.0 20.0 -35.0 25.0 Phantom Specifications LAT VERT 0.0 30.0 -17.0 40.0 -20.0 40.0 20.0 32.7 iPlan Stereotactic Coordinates AP LAT VERT 1.0 0.4 30.8 20.8 -17.1 42.4 -34.6 -19.7 40.8 25.5 20.2 33.5 Verification of MLC shapes and isocenter System Accuracy Simulate the entire procedures: Scan, target, plan, deliver Resulting film provides measure of targeting accuracy … Offset from intended target Phantom with film holder Pin denotes isocenter 4 … as well as falloff for a multiple arc delivery 1 RPC Phantom Hidden Target Test scan, plan, localize assess 0.8 0.6 0.4 0.2 0 -1 -0.5 0 0.5 Lucy Phantom 1 Off Ax is Distance (m m ) Courtesy Sam Hancock, PhD, Southeast Missouri Hospital Imaging Uncertainties • Use CT for geometric accuracy • Use MR for target delineation “MRI contains distortions which impede direct correlation with CT data at the level required for SRS” Stereotactic Radiosurgery – AAPM Report No. 54 1.8 ± 0.5 mm shift of MR images relative to CT and delivered dose Shifts occur in the frequency encoding direction Due to susceptibility artifacts between the phantom and fiducial markers of the Leksell localization box Other References TS Sumanaweera, JR Adler, S Napel, et al., Characterization of spatial distortion in magnet resonance imaging and its implications for stereotactic surgery,” Neurosurgery 35: 696-704, 1994. Y Watanabe, GM Perera, RB Mooij, “Image distortion in MRI-based polymer gel dosimetry of Gamma Knife stereotactic radiosurgery systems,” Med. Phys. 29: 797-802, 2001. What do we do about MR spatial distortion? Use Image Fusion Frequency Encoding = L/R Frequency Encoding = A/P Y Watanabe, GM Perera, RB Mooij, “Image distortion in MRI-based polymer gel dosimetry of Gamma Knife stereotactic radiosurgery systems,” Med. Phys. 29: 797-802, 2001. 5 Fusion Verification But image fusion will not work well if anatomy has deformed According to Watanabe et al (2001), image distortion in stereotactic MR imaging: According to Watanabe et al (2001), image distortion in stereotactic MR imaging: 1. is completely random 1. is completely random 2. has a systematic component of approximately 2 mm in the frequency encoding direction 2. has a systematic component of approximately 2 mm in the frequency encoding direction 3. has a systematic component of approximately 2 mm in the phase encoding direction 3. has a systematic component of approximately 2 mm in the phase encoding direction 4. has a systematic component that depends on the MR slice thickness 4. has a systematic component that depends on the MR slice thickness 5. is insignificant and can be ignored for stereotactic applications 5. is insignificant and can be ignored for stereotactic applications Correct answer: 2 Y Watanabe, GM Perera, RB Mooij, “Image distortion in MRI-based polymer gel dosimetry of Gamma Knife stereotactic radiosurgery systems,” Med. Phys. 29: 797-802, 2001. Small field depth dose show familiar trends Dosimetric Uncertainty 120 Stereotactic Diode 6 12 18 24 30 36 42 100 Percent Depth Dose Standard Diode Small field measurements can be challenging; Diodes and small ion chambers are well suited to SRS dosimetry, but their characteristics / response must be well understood. 80 60 80 100 60 40 20 0 0 50 100 150 200 250 300 350 400 Depth (mm) Pinpoint Chamber 0.015 cc 6 Similar machines have similar characteristics Penumbra: Cones versus MMLC 3.5 120 36A 12A 36 UNMC 12 Penumbra, 80%-20% (mm) Percent Depth Dose 100 80 60 40 20 0 0 50 100 150 200 250 300 350 Cones MMLC 3 400 2.5 2 1.5 1 0.5 Depth (cm) 0 0 20 40 60 80 100 Nominal Field Size (mm) Diode Warnings!!! 3) Reference diode output to an intermediate field size 1) Diodes exhibit enough energy dependence that ratios between large and small field measurements are inaccurate at the level required for radiosurgery Measure output factors ≤ 2x2 cm2 using diode ≥ 2x2 and ≤ 4x4 cm2 using diode & chamber ≥ 4x4 cm2 using chamber Output Factor = Reading (FS)diode Reading (Ref’)diode X Reading (Ref’)IC Reading (Ref)IC 2) Diode response will drift over time Re-measure reference between each chance in field size Radiosurgery beams exhibit a sharp decrease in output with decreasing field size 3) Reference diode output to an intermediate field size Significant uncertainty NO! YES! Reading (6 mm)diode Reading (100 mm)diode Reading (6 mm)diode Reading (24 mm)diode X Reading (24 mm)IC Reading (100 mm)IC Don’t use high energy This means that with small collimators, treatment times can be long 7 Need proof that beam data acquisition for small fields is difficult? 1.20 Total Scatter Factor @ 98.5 cm SSD and 1.5 cm depth relative to 10 x 10 cm2 Field Totlal Scatter Factor 1.00 0.80 0.60 Surveyed Beam Data from 40 identical treatment units: 0.40 Percent Depth Dose Relative Scatter Factors 0.20 Absolute Dose-to-Monitor Unit CF Reference Condition 0.00 0.0 20.0 40.0 60.0 80.0 100.0 120.0 Applied statistical methods to compare data Collimator (mm) Observations of some treatment units: 6 mm x 6 mm MLC 110 110 100 90 Institution A 90 80 InstitutionAB Institution Institution C 80 70 Percent Depth Dose Percent Depth Dose 100 60 50 40 30 Institution A Institution B 6.0 % 70 10.3 % 60 50 40 30 20 20 10 10 0 0 50 100 150 200 250 300 350 400 450 0 Depth (mm) 0 50 100 150 200 250 300 350 400 450 Depth (mm) Observations of some treatment units: 5 mm collimator Observations of some treatment units: 15 mm collimator 1.2 1.2 1.2 1.2 11 Institution A Institution A Institution B 11 Tissue Maximum Ratio Institution A A Institution Institution B 0.8 0.8 0.6 0.6 0.4 0.4 0.8 0.8 0.6 0.6 0.4 0.4 0.2 0.2 0.2 0.2 00 00 00 50 50 100 150 Depth (mm) Depth (mm) 200 250 300 00 50 50 100 100 150 150 200 200 250 250 300 300 Depth (mm) (mm) Depth 8 Relative Output Factor: 6 mm x 6 mm MLC Relative Output Factor: 42 mm x 42 mm MLC Output Factor Output Factor ~45% ~6% Institution Institution Commissioning your system: Does calculation agree with measurement? End-to-end testing Dosimetric uncertainty Calculation Calculation arc-step = 10o arc-step = 2o Relative Dosimetry End-to-end testing Dosimetric uncertainty 1 isocenter 4 field box Dynamic Conformal Arcs 2 isocenters Absolute Dosimetry 2 isocenters IMRT 9 Difference between calculation and measurement: the first 160 IMRT patients Independent MU Calculations x = 0.26 1σ = 1.75 Agazaryan et al, JCAMP, 2003 End-to-end testing Evaluating multiple sources of uncertainty Conventional Localization RPC SRS Phantom Does not include MRI imaging Does not include image fusion Provides only a spherical target Hidden Target Precludes image-guided positioning image image-guided Point dosimetry limited by TLD accuracy Limited information on dose distribution Test results require return of phantom Courtesy Sam Hancock, PhD, Southeast Missouri Hospital Dosimetry Insert Courtesy Sam Hancock, PhD, Southeast Missouri Hospital 10 Absolute Dosimetry Lucy Prototype Imaging Insert MR contouring and dosimetry based on MR contours Circular volumes for image fusion Courtesy Sam Hancock, PhD, Southeast Missouri Hospital Courtesy Sam Hancock, PhD, Southeast Missouri Hospital MR Fusion Courtesy Sam Hancock, PhD, Southeast Missouri Hospital What about “Frameless Systems?” Treatment Plan and Film Dosimetry Courtesy Sam Hancock, PhD, Southeast Missouri Hospital kV cone beam CT A “frameless” stereotactic system provides localization accuracy consistent with the safe delivery of a therapeutic dose of radiation given in one or few fractions, without the aid of an external reference frame, and in a manner that is non-invasive. Frameless stereotaxis is inherently image guided Also required: Immobilization – need not be linked to localization Ability to periodically monitor / verify 11 (Stereo)photogrammetry the principle behind frameless technologies Stereophotogrammetry in Radiotherapy Spatial Resolution: 0.05 mm Photogrammetry is a measurement technology in which the threedimensional coordinates of points on an object are determined by measurements made in two or more photographic images taken from different positions Temporal Resolution: 0.03 s Localization Accuracy: 0.2 mm Optical Photogrammetry Stereophotogrammetry in Radiotherapy In a rigid object, optical stereophotogrammetry can achieve a localization accuracy of approximately: 1. 0.2 mm 2. 0.5 mm 3. 1.0 mm 4. 1.5 mm 5. 2.0 mm Bova et al, IJROBP, 1999 In a rigid object, optical stereophotogrammetry can achieve a localization accuracy of approximately: 1. 0.2 mm 2. 0.5 mm 3. 1.0 mm 4. 1.5 mm 5. 2.0 mm X-ray Stereophotogrammetry Correct answer: 1 Schlegel et al, Radiotherapy and Oncology 29:197-204, 1993 Bova et al, IJROBP 38:875-882, 1997 12 X-ray Stereophotogrammetry Calibration of IGRT Systems Establish spatial dimensions Specify the isocenter Frameless (Image Guided) Radiosurgery Calibrate the x-ray system How do we know the system is targeting properly? End-to-end evaluation that mimics a patient procedure X-ray Identify target & plan Results of Phantom Data DRR (mm) Lat. Long. Vert. 3D vector Average -0.06 -0.01 0.05 1.11 Standard Deviation 0.56 0.32 0.82 0.42 Set up in treatment room Irradiate • Sample size = 50 trials (justified to 95% confidence level, +/- 0.12mm) Evaluate 1.2 Lateral Sup/Inf Ant/Post Single Fraction 1 0.8 0.6 0.4 0.2 0 -8.0 Comparison in 35 SRS patients and 565 SRT fractions -6.0 Single Fraction -4.0 -2.0 0.0 2.0 4.0 6.0 8.0 (mm) AP Lat Axial 3D vector Average 0.05 -0.06 0.26 1.01 Standard Deviation 0.55 0.67 0.72 0.54 13 1.2 Lateral Sup/Inf Ant/Post Multiple Fractions 1 1.2 Superior / Inferior Multiple Fraction Single Fraction 1 0.8 0.8 0.6 0.6 0.4 0.4 0.2 0.2 0 -8.0 -6.0 Multiple Fraction -4.0 -2.0 0.0 2.0 4.0 6.0 8.0 (mm) AP Lat Axial 3D vector Average 0.17 0.17 0.47 2.36 Standard Deviation 1.03 1.24 2.11 1.32 0 -8.0 -6.0 -4.0 -2.0 0.0 2.0 4.0 6.0 8.0 • Frameless localization appears equivalent to frame-based rigid fixation • Frameless localization improves accuracy of relocatable frames Localization using implanted fiducials Localization using implanted fiducials Courtesy Sam Hancock, PhD, Southeast Missouri Hospital Extracranial Applications - Spine Courtesy Sam Hancock, PhD, Southeast Missouri Hospital Extracranial Applications - Spine 14 Extracranial Applications - Liver What do you see on oblique radiographs of the chest or abdomen? Extracranial Applications - Lung The Better Approach Implanted Markers Not much Lots of redundancy End-to-end evaluation: Extracranial • Patient is marked • Immobilization device is marked • Location of IR markers is recorded • Table heights and shifts are provided 3D error 1.2 ± 0.4 mm 15 End-to-end evaluation: CyberKnife End-to-end evaluation: Calypso 3D error 1.1 ± 0.3 mm 3D σ = 0.34 mm (N=20) Chang et al, Neurosurgery 2003 Management of Respiratory motion is essential Can’t rely on the “Ignorance is Bliss” concept anymore Active Breathing Coordinator Eccles et al, IJROBP 64:751-759, 2006 Monitor the motion and limit it if necessary Courtesy Laura Dawson, PMH 16 Radiosurgery Guidelines ASTRO/AANS Consensus Statement on stereotactic radiosurgery quality improvement, 1993 RTOG Radiosurgery QA Guidelines, 1993 AAPM Task Group Report 54, 1995 European Quality Assurance Program on Stereotactic Radiosurgery, 1995 DIN 6875-1 (Germany) Quality Assurance in Stereotactic Radiosurgery/Radiotherapy, 2004 AAPM Task Group 68 on Intracranial stereotactic positioning systems, 2005 ACR Practice Guidelines for the Performance of Stereotactic Radiosurgery, 2006 ACR Practice Guidelines for the Performance of Stereotactic Body Radiation Therapy, 2006 AAPM Task Group 101, Stereotactic Body Radiotherapy, 2008 17






